Nonsyndromic craniosynostosis (NCS) is common among children and is manifested by numerous combined and isolated functional and cosmetic defects that can affect the normal development of the child. The incidence of NeCS ranges from 0.3 to 1.4 cases per 1000 newborns [1–4]. Neurological symptoms were thought to be uncommon in NCS [5]. Currently, more and more evidence is accumulating that changes in the neurological status of NCS in children are more common than expected. The results of modern studies have shown that they can manifest themselves as hypertensive-hydrocephalic syndrome and ophthalmological disorders [6, 7]. In addition, NCS is accompanied by pronounced cosmetic defects, which can further worsen the child’s social adaptation.
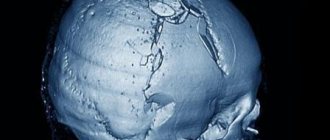
NeCS include scapho- (overgrowth of the sagittal suture) (Fig. 1, a), trigonocephaly (overgrowth of the metopic suture) (Fig. 1, b), unilateral overgrowth of the coronary (hemicoronal craniosynostosis - GCS) (Fig. 1, c) or half lambdoid suture (hemilyambdoid craniosynostosis - HLS) (Fig. 1, d), which leads to anterior or posterior plagiocephaly, respectively.
Rice. 1. Main forms of NeKS (according to CT data with 3D reconstruction of the skull). a — scaphocephaly (1 — absence of sagittal suture); b — trigonocephaly (2 — keeled deformity of the frontal bone); c — GKS (3 — absence of half of the coronary suture); d — GLS (4 — absence of half of the lambdoid suture).
Scaphocephaly is the most common form of NCS, ranging from 40 to 60%. It occurs with a frequency of 0.2 to 1 per 1000 newborns, more often (70-90%) in boys [8]. Scaphocephaly is an isolated monosynostosis and is not associated with any clinical syndrome; from 2 to 6% of children with this disease are close relatives [9]. It is characterized by a pronounced increase in the fronto-occipital size and a decrease in the biparietal size of the skull, which is limited due to the overgrowth of the suture. With this form, the skull becomes narrow and elongated in the longitudinal direction, which is compensatory in nature (Fig. 2, a).
Rice. 2. Characteristic changes in the shape of the skull with various NeCS. a - scaphocephaly; b — trigonocephaly; c — GKS; d — GLS (the icon marks the areas of damage to the cranial sutures.
Trigonocephaly occurs in 10% of cases [10, 11], more often (75-85%) in boys [8]. This type of craniosynostosis may be of a genetic nature due to abnormalities of chromosomes 3, 9, 11 and be combined with other anomalies of the development of the nervous system [12, 13]. It is impossible to predict the degree of brain damage in this disease. Trigonocephaly is more often than other NECs accompanied by cognitive impairment. Patients with almost equal frequency may experience both good compensation and pronounced impairments in the intellect and visual organs [14]. It manifests itself in the formation of a triangular deformation of the forehead with the formation of a bone keel extending from the glabella to the greater fontanel (BR). Noteworthy is the clear triangular deformation with its apex in the region of the glabella. The upper and outer edges of the orbits shift posteriorly, which is accompanied by an outward turn of the orbital plane and a decrease in the interorbital distance, and hypotelorism occurs [15]. The deformity is so unique that children with trigonocephaly are often consulted by geneticists and observed as carriers of hereditary neurological syndromes. With age, there is a slight correction of the forehead deformation due to smoothing of the apex of the ridge and the development of the frontal sinuses, but the pronounced curvature of the frontal bone, hypotelorism and outward rotation of the supraorbital edges are preserved (Fig. 2, b).
GCS occurs with a frequency of 1 in 10,000 newborns (17-25% of all non-CS), in 76% of girls [16]. The right half of the coronary suture is most often affected [17]. With GCS, flattening of the upper edge of the orbit and frontal bone on the affected side occurs with a compensatory overhang of the opposite half of the forehead, ipsilateral flattening of the zygomatic region and curvature of the nose in the same direction. GCS is also manifested by bite deformation associated with an increase in the height of the upper jaw and, as a consequence, displacement of the lower jaw on the side of the prematurely closed suture. Disturbances of cranial innervation are most often represented by unilateral strabismus in 50-60% of patients. Its causes are displacement of the shortened anterior cranial fossa, deformation of the upper wall of the orbit and trochlea with involvement of the internal oblique muscle [18] (Fig. 2, c).
The prevalence of HLS ranges from 0.9 to 4% [9]. Diagnosing it is difficult, since unilateral flattening of the occiput is often considered as positional, caused by the forced position of the child’s head on its side. Therefore, this form is more often than others regarded as a feature of the postpartum configuration of the head, but does not disappear in the first weeks of life, but, on the contrary, progresses with age (Fig. 2, d).
Correction of cranial deformation with NeCS is only possible through surgery. To achieve maximum functional and cosmetic effects, early surgical treatment of children with NCS is necessary. Therefore, early identification of children with this pathology is of fundamental nature [19, 20]. The need for surgical treatment of children at this age dictates the advisability of using the most minimally invasive methods. These methods include endoscopic correction, which allows minimizing surgical aggression and does not have a number of disadvantages that traditional surgery for non-CS has. The surgical aspects of correction of various forms of NeCS using this method were described by us earlier [21—23].
A long period of observation of children with various types of NeCS with good functional and cosmetic results after endoscopic correction, as well as the absence of surgical complications, allow us to conclude that the use of this method in the clinic is appropriate and safe. There has been an increase in the number of older children with developed craniosynostosis. It should be noted that all these patients were observed by neurologists and pediatricians at their place of residence, which suggests insufficient knowledge of the clinical manifestations of this pathology by outpatient service specialists.
The purpose of this work is to study the clinical manifestations of NeCS in children.
About the disease
Among the deformations of the skull there are congenital and acquired.
Congenital ones appear during pregnancy, and the child is born with a certain malformation. Acquired ones occur after childbirth, most often as a result of injury or certain intervention, such as surgery. Craniostenosis in children can be either congenital or acquired after birth. This defect is a premature fusion or absence of sutures in the bones of the skull, which normally should remain plastic for the natural growth and development of the child's brain. As a result, intracranial pressure increases and the shape of the skull changes. If we are talking about a developmental defect, craniostenosis in newborns may be accompanied by other defects that affect the brain and other organs of the body. In the case of an acquired disease, suture fusion occurs due to injury or surgery.
Craniostenosis occurs in one in 1000 newborns.
3242
send an SMS with the donation amount to this number
Craniostenosis, craniosynostosis and cranial deformities
Craniostenosis, craniosynostosis and cranial deformations are the result of premature or uneven ossification of cranial sutures (Greek kranion - skull; synostos - fusion; stenos - narrow, close). The incidence of craniostenosis is 1 in 1000 newborns. The immediate cause of the development of craniostenosis is seen in: a) metabolic disorders, which entails accelerated osteosynthesis of the skull bones (Greek osteon - bone; synthesis - connection, combination, composition); b) disorder of the blood supply to the bones and membranes of the brain; c) reducing the force acting through the dura mater on the cranial vault and promoting its stretching.
There are primary, or idiopathic (Greek idio - special; pathos - suffering, disease), and secondary craniostenosis. Primary craniostenosis is hereditary or associated with a hereditary predisposition. This, for example, is the symptom complex of Tersil (1942), which includes: 1) tower skull; 2) exophthalmos; 3) nystagmus; 4) mental retardation; 5) epileptic seizures; 6) intracranial hypertension and 7) optic atrophy with blindness. Primary craniostenosis is included in the clinical picture of many hereditary mental retardation syndromes with different types of inheritance. Secondary craniostenosis develops for various external reasons, such as inflammatory processes, vitamin D-deficiency rickets, phosphorus deficiency in the blood, overdose of thyroid hormone (in the treatment of hypothyroidism), X-ray exposure in the first half of pregnancy.
Normally, in newborns, all the bones of the skull are not fused, the anterior and posterior fontanelles are open. The posterior fontanel closes by the end of the 2nd month, the anterior one - during the 2nd year of life after childbirth. By the end of the 6th month, the bones of the calvarium are connected to each other by a dense fibrous membrane (Latin fiber - thread). By the end of the 1st year, the child’s head size is 90%, and by 6 years it reaches 95% of the adult’s head size. The closure of the sutures by connecting the jagged edges of the bones begins by the end of the 2nd year and is completely completed by the age of 12–14 years.
Premature overgrowth of the fontanelles and cranial sutures leads to a narrowing of the skull and a decrease in the volume of the cavity of the cranium. This interferes with normal brain development and creates conditions for liquorodynamic disturbances. With an increase in intracranial pressure, an associated hypertensive headache occurs (Greek hyper + Lat. tension - tension). The development of congestion in the fundus of the eye, concentric narrowing of the visual fields, and subsequently secondary atrophy of the optic nerves with a progressive decline in vision up to its loss are also possible. Typically, exophthalmos occurs on both sides, disorders of the oculomotor nerve, thinning of the skull bones, and the appearance of digital impressions in the bones of the calvarium, visible on x-rays. There is a high risk of developing mental retardation.
In case of secondary craniostenosis in the early stages of its formation, conservative treatment of the underlying disease can be effective. In case of primary craniostenosis, as well as secondary craniostenosis in the case of already developed significant intracranial hypertension, shunting and decompression therapy are indicated: the formation of craniectomy passages up to 1 cm wide along the line of suture ossification. Timely surgical treatment for craniostenosis ensures further normal development of the brain.
Premature or uneven overgrowth of the fontanelles and cranial sutures also leads to deformation of the skull. The shape of the skull is assessed taking into account the cranial index (CI) - the ratio of the transverse and longitudinal dimensions of the skull. Normally, or mesocephaly (Greek mesos - average), the CI is 76–80.0 in men, 77–81.9 in women. With premature overgrowth of the sagittal (Latin sagittal - arrow) suture dividing the skull into the right and left halves, dolichocephaly (Greek dolichos - long) occurs with a CI of less than 75. A variant of dolichocephaly is scaphocephaly (Greek skaphe - boat) or cymbalocephaly (scaphoid head), in which the elongation of the head is complemented by a protruding forehead and nape. There may also be a saddle-shaped skull - it is elongated and depressed in the parietal region.
With premature overgrowth of the coronal sutures (coronal or coronal synostosis), brachycephaly occurs (Greek brachys - short) - an increase in the transverse size of the head with a CI of more than 81. In this case, the face of children is flattened, and exophthalmos often occurs. With premature overgrowth of the coronal suture on one side, plagiocephaly (Greek plagos - oblique), or cross-headedness is formed: the skull is asymmetrical, the frontal bone on the side of the synostosis is flattened, on the same side there may be exophthalmos, as well as an increase in the middle and posterior cranial fossae.
If both the sagittal and coronal sutures heal prematurely, the growth of the skull continues only in height. As a result, a high conical skull is formed, somewhat flattened in the anteroposterior direction - acrocrania (Greek akron - limb), or tower skull. A variant of acrocrania is a pointed skull, or oxycephaly (Greek oxis - sharp) - a high skull, tapering upward and with a sloping forehead.
Premature fusion of the frontal suture is characterized by a narrow frontal and broad occipital bone. In this case, the frontal bones grow together at an angle, and a “ridge” is formed at the site of the frontal suture. If the posterior parts of the skull enlarge compensatoryly and its base deepens, trigonocrania occurs (Greek trigonon - triangle).
Brachycephaly, scaphocephaly and trigonocephaly are usually not accompanied by neurological pathology. If there is no brain damage, then there is no psychiatric pathology.
Return to Contents
Why is craniostenosis dangerous?
The absence of movable sutures in the skull severely limits the brain. Therefore, the sooner help comes for craniostenosis, the higher the likelihood of a complete cure for the child in the future. Compensation mechanisms in infants under 2 years of age are very high, but rehabilitation after this age turns out to be more complex and lengthy. If not treated promptly, the disease can cause the following conditions:
If you do not receive treatment in a timely manner, the disease can cause the following conditions:
- delayed physical, mental, intellectual development;
- disruption of normal brain functions;
- skeletal underdevelopment;
- compression and atrophy of the optic nerve up to complete loss of vision;
- headache;
- ophthalmological diseases;
- death.
Material and methods
An analysis was carried out of 56 cases of NCS of various forms in children who were treated at the Federal Center for Neurosurgery (Tyumen) in 2012 and the first half of 2013. Among the 56 children there were 45 (80%) boys and 11 (20%) girls , average age - 9.21±6.73 months. The ratio of NeCS was distributed as follows: 28 (50%) children had scaphocephaly, 21 (38%) had trigonocephaly, 7 (12%) had various forms of plagiocephaly. This ratio of HeCS forms is not typical. As already mentioned, trigonocephaly usually ranks 3rd in the NeCS structure. Unfortunately, we were unable to identify any patterns of such statistical features.
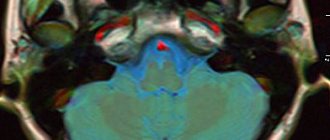
After admission to the clinic, all children underwent a CT scan with 3D reconstruction of the skull in order to clarify and verify the diagnosis. Complaints, gender, age, medical history, and the presence of concomitant pathology were analyzed. Together with a neurologist, the child’s neurological status was analyzed in detail at the time of admission to the clinic. The examination included a study of the functions of the cranial nerves, motor and sensory spheres, physiological reflexes (including age-related ones), and the coordination system.
Statistical analysis of the obtained information was performed using Microsoft Excel 2003 (Microsoft Corporation, USA). To describe quantitative data, the average values of the studied indicator and standard deviation were used. Data are presented as M
±
Sd
, where
M
is the average value,
Sd
is the standard deviation.
What is craniostenosis in children?
First of all, it depends on whether the child has other developmental defects. Sometimes pathology accompanies various syndromes - then it is called syndromic. For example, it can occur simultaneously with fusion of fingers or toes, cleft palate or lip, or cerebral hernia.
If fusion of the sutures in the bones of the skull occurs without other developmental defects, it is considered non-syndromic, that is, independent.
Doctors classify the disease into types based on which cranial sutures are fused:
- metopic,
- lambdoid,
- coronary,
- sagittal.
Synostosis - or suture fusion - can involve one to several sutures. There is a concept of pansynostosis - complete overgrowth of all seams. This type of pathology can be considered the most severe; it is less common than others.
How is craniostenosis treated in children?
There is only one way to eliminate the pathology - surgery. It is performed to restore the shape of the skull bones. After the bones take their natural shape, they are held together with mini-screws or mini-plates and surgical wires, which are removed after a year. They are removed after a year. During the operation, doctors use modern, technologically advanced biodegradable material, which does not need to be removed surgically - it gradually dissolves on its own, and in its place, the patient’s own bone tissue grows. This greatly simplifies the patient's recovery.
The best results can be expected if the surgery is performed between 3–4 months and 2 years of age. Severe deformations of the skull can sometimes be noticed only after the bones have completed their formation, that is, at the age of 5–6 years. In such cases, the pathology manifests itself as severe headaches, blurred vision and increased intraocular pressure, increased fatigue and irritability.
If the disease occurs as a response to craniotomy or after injury, the deformed section of the bone is removed and an implant made of modern material - polymer, metal or ceramic - is installed in its place.
Skull deformation in newborns
Skull deformation in newborns is a fairly common problem. Skull deformation occurs for many reasons. Correcting the shape of a child’s skull is not only possible, but also necessary. And, in some cases, a cranial orthosis (special helmet) can help with this. The age of the child in this case is of decisive importance - optimal results from correcting the shape of the skull with helmets can be achieved when treatment begins at the age of up to 5 months.
Often, parents seek help when time has already been lost, trying to follow various popular advice: laying the child in a certain position, performing a massage, using other paramedical methods (from homeopathy to osteopathy).
Although there is an effective and safe way to change the shape of the skull - correction of the shape of the head using cranial orthoses (helmets).
The method has been known since ancient times. In the culture of the Mayans, Incas, and some African tribes (for example, the Mangbetu), the shape of a child’s skull was changed by constructing special stocks. During the growth process, up to 12-15 months, the skull acquired the desired shape.
Currently, this feature of the growing body is used by doctors around the world to correct the shape of the head. The “block” is a cranial orthosis, which is made individually based on a three-dimensional model of the child’s head.
Dear Parents! Don't miss out! Seeking advice from a neurosurgeon will help you avoid many problems in the future. Attempts to correct the shape of the head using methods that are far from evidence-based medicine (osteopathy, homeopathy, spells) take time and do not produce results. If your child is diagnosed with craniostenosis, lost time can have a devastating impact on his health and quality of life.
Is there any cause for concern?
The simplest test that can be done at home and understand whether there is cause for concern and a visit to the doctor:
Look at your baby's head from the top, front and side. Does it differ from the conventionally accepted norm?
Have you checked? Everything is fine? Exhale and get ready for a walk.
If the shape of the child’s head raises questions, you should consult a doctor - a neurologist or neurosurgeon. The doctor will help determine whether the abnormality in your case is a deformity and prescribe treatment.
It won't go away on its own! No, miracles, of course, happen, but, alas, not in the case of skull deformation... History repeats itself over and over again: grandparents, friends and neighbors, and even, the saddest thing, doctors assure parents who have noticed a deformation of the skull in their child, that there is no need to worry, that after a year everything will go away on its own!!
You need to worry!
It is important to consult a neurosurgeon as early as possible and undergo prescribed examinations. If your doctor does not see deformation, and you still have doubts, it will be useful to find out the opinion of specialists in other clinics. It’s better to worry and act than to rely on “maybe” and “it will go away on its own,” and then reproach yourself for inaction.
If treatment with a helmet is started in a timely manner (at the age of 4 to 8 months), it gives very good results - you can see them on our website. In some cases, surgical treatment may be required; its necessity is determined by a neurosurgeon.