We offer consultations via Skype or WhatsApp.
Emotionally unstable (labile) personality disorder is characterized by increased excitability, impulsivity, low ability to self-control and emotional imbalance. Like other personality disorders, it is a character pathology (“severe character”) rather than a disease. An experienced psychotherapist can help with the disorder.
Important
A “difficult character”, the inability to cope with one’s emotions is a reason to seek help from a psychotherapist.
Another name for aggressive, epileptoid, excitable, explosive personality disorder. Doctors sometimes treat it as two separate disorders—impulsive disorder and borderline personality disorder.
A common characteristic of people with both types of emotionally unstable personality disorder is that they have difficulty controlling themselves and obeying norms and rules due to poor self-control and impulsivity. Personality traits make it difficult to establish and maintain contacts with others. Treatment with a psychotherapist for such people is an opportunity to accept the characteristics of their psyche and learn to live in harmony with others.
Symptoms of epileptoid personality disorder
If we talk about the classification of emotionally unstable personality disorder, ICD-10 divides it into two subtypes:
- Impulsive.
- Borderline.
Emotionally unstable personality disorder of the impulsive type is characterized by severe emotional lability (frequent change of mood for no reason), a tendency to impulsive actions and aggressive outbursts with an inability to restrain itself. People with this disorder have a hard time withstanding criticism and reproach.
Epileptoids are characterized by jealousy, suspicion, a tendency to manipulate, irritability and outbursts of anger.
Emotionally unstable borderline personality disorder is less characterized by aggressive behavior towards others, but such people are prone to self-harm, even suicidal behavior. Read more about borderline disorder.
According to ICD-10, the disorder is characterized by general features of a personality disorder and specific features. The general criteria are as follows:
- begins to manifest itself in childhood and adolescence, persists into adulthood;
- it is difficult to identify clear phases of recovery/exacerbation;
- character traits prevent you from communicating with loved ones and strangers, and prevent you from developing professionally;
- a person is often self-centered, incapable of empathy (sympathy for other people), and constantly strives for pleasure.
Specific symptoms of the impulsive (explosive) type of emotionally unstable personality disorder:
- Impulsivity in thoughts and actions.
- Low ability to self-control.
- Outbursts of anger.
- Tendency to cruel and antisocial behavior.
- Intolerance of blame and criticism.
To diagnose the impulsive type of emotionally unstable personality disorder, the psychotherapist talks in detail with the client.
Differential diagnosis is carried out with other personality disorders (borderline, hysterical), as well as with epilepsy. For this purpose, a pathopsychological study is used (performed by a clinical psychologist), EEG, and Neurotest.
An integrated approach to diagnosis is necessary so that the doctor can prescribe the most effective treatment for a given person.
Don't diagnose yourself!
If your mood changes every day, this does not mean that you are bipolar. If you don't feel like getting off the couch on weekends, it's not depression. Cutting your hands is not a nervous breakdown, but may well be a common desire to attract attention. Self-medication will not lead to anything good! And it will only make things worse. Perhaps if I had gone to the doctor at 18, instead of seven [years after the onset of the disease], I would not have had scars for life. Both in the hands and in the heart.
Emotionally unstable personality disorder - treatment
People with emotionally unstable personality disorder especially urgently need the help of a psychotherapist. A specialist can teach them to control their emotions and prevent the negative impact of emotional outbursts on others (with impulsive disorder) and on the person himself (with borderline personality disorder).
Labile personality disorder has been described as one of the most difficult diagnoses to treat. Establishing contact with a person who suffers from an emotionally unstable personality disorder is not an easy task for a psychotherapist. Inexperienced specialists avoid a strong alliance with such patients so as not to lose their own peace of mind.
But it is important to remember that a personality disorder is not a disease; the patient does not have damage to the nervous system. Consequently, with proper treatment, it achieves serious positive results. People with borderline and aggressive personality disorders should be treated by an experienced psychotherapist.
Important
Psychotherapy is the main non-drug treatment method for mental disorders. Unlike medications that eliminate symptoms, it works with the cause - allowing you to achieve long-term, lasting results.
The main treatment method for emotional personality disorder is psychotherapy. Drug treatment is not used in all cases. Medication support is sometimes necessary if the personality disorder is combined with other illnesses, such as depression.
The most effective techniques for working with people who suffer from emotionally labile personality disorder are cognitive behavioral therapy and dialectical behavior therapy. They help patients become aware of the thoughts and feelings that influence their actions and teach them how to control themselves.
If all the doctor’s recommendations are followed and, most importantly, the patient’s desire to interact with the psychotherapist, therapy has a lasting positive effect. At the same time, the specialist does not seek to change the patient’s personality, but helps to accept himself and learn to live in harmony with himself and others.
Author: Specialist of the Alliance Mental Health Center
Prices for services
| 6,000 rub. | |
| Individual psychotherapy session with a subscription for 10 sessions | 6,000 rub. 5,400 rub. |
| 8,000 rub. | |
| Biofeedback therapy session (I-st) with a subscription for 10 sessions | 4,000 rub. 3,600 rub. |
SpecialistsDeputy Head of the Center, psychotherapist, psychiatrist
- Individual psychotherapy
- Family psychotherapy
- Psychopharmacotherapy
- Rational psychotherapy
Psychotherapist, psychiatrist
- Suggestive therapy
- Reconstructive-personal psychotherapy
- Rational psychotherapy
- Individual psychotherapy
Psychotherapist, psychiatrist
- Individual psychotherapy
- Family psychotherapy
- Cognitive behavioral psychotherapy
- Reconstructive-personal psychotherapy
Psychiatrist, psychotherapist
- Ericksonian hypnosis
- Neurolinguistic programming
- Cognitive behavioral psychotherapy
- Holotropic Breathwork
Psychotherapist, psychiatrist
- Body psychotherapy
- Cognitive behavioral psychotherapy
- Child-parent relationships
- Art therapy
The International Classification of Diseases, 10th Revision, lists BPD as “Emotionally unstable personality disorder (F60.3).”[2] It is this name that is common in Russia. This disorder is also called borderline disorder.
The causes of BPD are not completely clear, but it is becoming increasingly clear that the appearance of this disorder is due to genetic, brain, and social factors. Borderline disorder occurs 5 times more often in people with disrupted family relationships (neglected by parents, active criticism and rejection from loved ones). BPD is 3 times more common in women than in men.[3]
Unfavorable life factors (for example, physical or emotional abuse) also play an important role in the appearance of this deviation. A number of neurophysiological studies have shown that the manifestations of the disorder are associated with frontal-limbic groups of neurons.[4][5][6]
Prevalence
According to a 2008 study, the prevalence of the disorder in the population is 5.9%. About 20% of psychiatric hospitalizations are for patients with BPD.[7]
Emotional lability refers to sudden mood swings: panic or sadness may be replaced by attacks of aggression, then a burning feeling of guilt may arise, etc.
Separation anxiety is the anxiety that a person experiences due to separation from home and loved ones.
Description
BPD is a relatively common disorder that causes significant impairment in a person's life. Psychotherapy with people with BPD is usually quite difficult, and there is a significant risk of negative treatment outcome, regardless of the treatment approach used (Mays, 1985). Direct application of behavioral techniques with borderline patients is less effective than with other clients (Mays, 1985), and until recently some authors believed that these clients could not be effectively treated with cognitive psychotherapy (Rush & Shaw, 1983). However, with the development of the cognitive-behavioral approach to BPD (Freeman, Pretzer, Fleming, & Simon, 1990; Linehan, 1981, 1987a, b; Millon, 1981, 1987; Pretzer, 1983; Young, 1983, 1987; Young & Swift, 1988) It has become possible to develop principles for the effective use of cognitive psychotherapy with this complex population.
Pathogenesis of borderline personality disorder
As with other mental disorders, the pathogenesis of BPD is multifactorial and not fully understood. According to some studies, borderline disorder shares similarities and causes with post-traumatic stress disorder (PTSD). In addition, their pathogenetic relationship is possible.
Most researchers agree that a history of childhood chronic emotional trauma contributes to the development of BPD. However, it is worth noting that insufficient attention is paid to studying the role of other pathogenetic factors: congenital brain dysfunctions, genetics, neurobiological factors and social environmental factors.
Social factors refer to the interaction of people in the process of growing and maturing in their families, surrounded by friends and other individuals.
Psychological factors include personality and temperament, adaptation to the environment, and developed skills to cope with stress.
Genetics
The heritability of BPD is approximately 40%. In reality, it is quite difficult to achieve an objective assessment of genetic factors. For example, the twin method can give overestimated indicators due to the presence of traumatic factors in the common family of siblings.[9] However, one study found that BPD is the third most heritable personality disorder out of ten. A study in the Netherlands (Trull & colleagues) found that genetic material on chromosome nine is associated with symptoms of BPD. Based on this, scientists concluded that genetic factors play a key role in the individual characteristics of the disorder in each individual patient. The same researchers previously found that 42% of BPD symptoms are determined by genetics and 58% by environmental influences.[10]
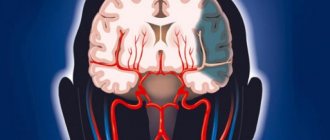
Features of the brain
A number of studies in the field of neuroimaging in BPD have shown the presence of reduction (decrease) of brain matter in specific areas. These departments are normally involved in regulating the response to stress and regulating the emotional sphere. We are talking about the hippocampus, the orbital-frontal areas of the cerebral cortex (prefrontal cortex), and the amygdala.[11]
- The amygdala is smaller in absolute volume and more active in people with BPD. Reduced amygdala volume has also been found in patients with obsessive-compulsive disorder. One study found abnormally high activity in the left amygdala of people with BPD when they looked at cards depicting people in negative emotions. Because the amygdala generates all emotions, including negative ones, this unusually high activity may explain the intense and prolonged emotional expressions of fear, grief, anger and shame experienced by people with BPD. The same fact is interpreted by their ability to subtly recognize the emotions of other people.[12]
- The prefrontal cortex tends to be less active in individuals with BPD, especially when memories of their “emotional abandonment” are recalled. This relative decrease in activity is most pronounced in the right anterior gyrus . Given the role of the prefrontal cortex in regulating emotional arousal, the relative inactivity of these areas may explain the difficulty people with BPD have in regulating their emotions and responding to stress.[13]
- The hypothalamic-pituitary-adrenal (HPA) axis regulates the production of cortisol , which is released in response to stress. Levels of this adrenal hormone are actually higher in people with BPD than in the general population. This is a sign of HPA axis hyperreactivity. Hyper-reactivity may explain a higher biological response to stress and greater vulnerability to disturbing factors. Also, high cortisol levels are associated with a high risk of suicidal behavior.[12]
Neurobiological factors (estrogens)
A controlled study in 2003 found that BPD symptoms in women were predictably associated with estrogen (female sex hormone) levels during the menstrual cycle.[14]
Personal development factors (childhood trauma)
There is a strong relationship between child abuse, especially child sexual abuse, and the development of BPD.
Children who experience chronic self-maltreatment and difficulty forming attachments early in life are hypothesized to be on the path to developing BPD.[15]
“I believed - they understand me!”
The last four years have been very difficult for me: a painful relationship (with Stockholm syndrome), months of lying under a blanket without leaving the house, lack of appetite, minus 6 kg per month. And tears, tears, tears. Without a reason.
It was painful for my friends to look at me; they did not understand what was wrong with me. And when I started to faint from lack of strength and hunger, I went to the doctor.
I was scared, ashamed, incomprehensible. For the first twenty minutes of the appointment, I was simply silent. I was lucky with the doctor.
During my first visit, I gained confidence in the doctor; they told me that I was not alone, and that they would help me. They prescribed several medications and released me. We agreed to meet in two weeks and call each other every three days. The most important thing is that I believed that they understand me!
The obsessive desire to throw myself under a train disappeared approximately on the sixth or seventh day. Tears on the tenth. I started laughing at a stupid meme in the morning, and then all day with my colleagues after about two weeks. The anxiety did not go away, social phobia intensified, and insomnia also accompanied me. But overall I became calmer and more smiling.
Now, thanks to a psychiatrist, I know the reason for my fears - this is the fear of not being accepted in society. I'm trying to hide and disappear because I'm afraid that I'm not like that, I'm not funny, I'm not cheerful, I'm talking nonsense and in general, have you seen yourself in the mirror?
Classification and stages of development of borderline personality disorder
American psychologist Theodore Millon identified 4 subtypes of BPD:[16]
1. Sad Borderline Disorder (includes avoidant or dependent personality traits).
- Characteristic features: compliance, humility, loyalty, modesty; feeling of vulnerability and constant danger; the individual experiences feelings of hopelessness, depression, helplessness and impotence.
2. Touchy borderline disorder (includes passive-aggressive personality traits).
- Characteristic features: negativism (opposition to everything), impatience, anxiety, as well as stubbornness, defiant behavior, gloominess, pessimism; a person is easily offended and quickly disappointed.
3. Impulsive borderline disorder (includes histrionic and antisocial personality traits).
- Characteristics: capriciousness, superficiality, frivolity, feverish and seductive behavior; fearing loss, a person easily falls into agitation (excitement); gloominess and irritability; potentially suicidal intent.
4. Self-injurious borderline disorder (includes depressive and masochistic, as well as self-destructive personality traits).
- Characteristic features: isolation, self-punishment, anger, conformity, deference, ingratiation, progressively rigid and gloomy state; there is a risk of suicide.
Severity of personality disorder[17]
| Degrees of severity of personality disorders |
| Light |
| Average |
| Heavy |
Interpretation Neuropsychic instability (the opposite concept is neuropsychic stability) is a tendency to breakdowns of the nervous system under significant physical and mental stress.
This concept includes various pre-morbid conditions (extreme variants of the mental norm) with a hidden, not expressed, or moderately expressed, but compensated form of the course, caused by deficits in the functioning of the nervous system and reducing the adaptive capabilities of the body. In the origin of neuropsychic instability, the determining role is played by the biological inferiority of the nervous system (congenital or acquired) in combination with unfavorable psychological and social factors. Neuropsychic instability gives rise to: suicidal attempts, self-harm, desertion, assault, evasion of official tasks, irritability, conflict, withdrawal, isolation, posturing, inability to perform due to forgetfulness, tearfulness, non-resistance to humiliation. Sources of neuropsychic instability: mental illness, illness (meningitis, encephalitis), traumatic brain injury, alcoholism, drug addiction, substance abuse, family troubles, mental retardation. Methods for identifying persons with neuropsychic instability: observation, analysis of documents, conversation, analysis of independent characteristics, testing, analysis of performance results, experiment, correspondence with parents, medical examination. Psychological and pedagogical dictionary of a naval unit teacher educator. - Novorossiysk: Publisher: Novorossiysk. G.A. Bronevitsky, G.G. Bronevitsky, A.N. Tomilin. 2005.
See what “Nervous-mental instability” is in other dictionaries:
- Neuropsychic instability - <*> Neuropsychic instability is understood as a tendency to disturbances in mental activity under significant mental and physical stress... Source: Order of the Minister of Defense of the Russian Federation dated January 26, 2000 N 50 (as amended on May 12, 2005) About... ... Official terminology
- MENTAL TRAUMA - MENTAL TRAUMA, experiences that are unpleasant or frightening, b. or m. deeply disrupting basic mental and somatic processes. These experiences can be of a different nature, both in content and affective coloring, as well as in intensity and... ... Big Medical Encyclopedia
- Interrogation in a conflict situation is one of the procedural forms of professional communication between an investigator and interrogated persons for various, often incompatible (as opposed to interrogation in a conflict-free situation) purposes. Often a conflict situation of interrogation is characterized by active... ... Encyclopedia of modern legal psychology
- PSYCHOHYGIENE - PSYCHOHYGIENE. Contents: I. Subject and tasks P……………749 II. History of the psychohygienic movement. . . 751 III. Methods and content of psycho-hygienic work: P. industrial…………….. 753 P. mental work…………… 755 … Great Medical Encyclopedia
- Psychogram of a customs service specialist - A section of the professiogram, which reflects in scientific psychological concepts the system of requirements of the customs profession for the psychological and psychophysiological qualities of a customs officer and the measure of their severity. Fundamentals of professionography and systems... ... Encyclopedia of modern legal psychology
- NEURASTENIA is a state of disorder characterized by irritable weakness, excessive fatigue, and increased fatigue. Neurasthenia was described as a specific disorder by the American physician J. Baird (1839–1883) in his work... ... Encyclopedic Dictionary of Psychology and Pedagogy
- Carbon disulfide - CS2, a compound of sulfur and carbon. Colorless liquid, density 1.2927 g/cm3, tkip 46.26°C, melting point 112.1°C. Solubility in water is insignificant; it can be mixed with alcohol, ether, and chloroform in any proportions. Vapors at 236 °C... ... Great Soviet Encyclopedia
- Traumatic brain injury - I Traumatic brain injury Traumatic brain injury is mechanical damage to the skull and (or) intracranial formations (brain, meninges, blood vessels, cranial nerves). Accounts for 25-30% of all injuries, and among deaths with... ... Medical Encyclopedia
- Narcology - This article needs to be completely rewritten. There may be explanations on the talk page... Wikipedia
- Neuroses are (neuroses; Greek neuron nerve + ōsis) reversible borderline mental disorders, recognized by patients, caused by the influence of traumatic factors and occurring with emotional and somatovegetative disorders. The main reason... ... Medical encyclopedia
InterpretationTranslationEmotional instability is the tendency to exhibit excessively strong, short-lived, unpredictable and maladaptive emotional reactions.
* * * – emotional lability, a tendency to express sharply and unpredictably strong emotions, easy variability of feelings and moods, especially as a result of inadequate reactions to weak stimuli. Wed. the image of Nozdryov in “Dead Souls” by N. Gogol, Sheila Castleside in “Blackout at Gretley” by J. Priestley.
Wed. instability of behavior.
Encyclopedic dictionary of psychology and pedagogy. 2013.
See what “Emotional instability” is in other dictionaries:
- EMOTIONAL INSTABILITY - The tendency to be emotionally labile, to express one’s unpredictably strong emotionality extremely sharply... Explanatory Dictionary of Psychology
- Emotional lability - Instability of emotional states, rapid change of one emotional reaction to another. E. l. is one of the signs of incoordination, disorders of higher nervous activity and the human psyche as a whole... Adaptive physical culture. Concise encyclopedic dictionary
- Lability of affect is instability of mood, its constant fluctuations, frequent changes for minor reasons or for no apparent reason. In clinically significant cases, it is considered a manifestation of emotionally labile psychopathy. Synonyms: Emotional... ... Encyclopedic Dictionary of Psychology and Pedagogy
- Neuroses are a group of functional neuropsychic disorders, the main causes of which are intrapsychic conflict (in psychoanalysis) and/or a traumatic situation (in domestic psychiatry), see Neurosis. Different types are known... ... Encyclopedic Dictionary of Psychology and Pedagogy
- Nursing - I Nursing. Nursing is a set of activities that provide comprehensive care for the patient, fulfillment of medical prescriptions, creation of optimal conditions and environment conducive to a favorable course of the disease, the fastest ... ... Medical encyclopedia
- infantilism - a; m. [from lat. infantilis infantile, children]. 1. Honey Developmental retardation, manifested in the preservation in an adult of physical or mental traits characteristic of a child. Suffer from infantilism. 2. Book. Behavior, character traits of an adult ... Encyclopedic Dictionary
- Dialectical behavior therapy (DBT) was created around 1987 by American psychologist Marsha M. Linehan to treat patients suffering from borderline personality disorder. This approach helps reduce the risk... ... Wikipedia
- Neuroses are (neuroses; Greek neuron nerve + ōsis) reversible borderline mental disorders, recognized by patients, caused by the influence of traumatic factors and occurring with emotional and somatovegetative disorders. The main reason... ... Medical encyclopedia
- Mental retardation - This article should be Wikified. Please format it according to the article formatting rules. Mental retardation (abbr. DPR) is a violation of the normal pace of mental development, when individual mental functions ... Wikipedia
- Psychogram of a customs service specialist - A section of the professiogram, which reflects in scientific psychological concepts the system of requirements of the customs profession for the psychological and psychophysiological qualities of a customs officer and the measure of their severity. Fundamentals of professionography and systems... ... Encyclopedia of modern legal psychology
Books
- My little bastard. A little about children with attention deficit hyperactivity disorder, Guy Sebeus. What to do if the child is completely uncontrollable? If he doesn’t hear any requests or orders? What to do if the parent committee demands that he be removed from the class because he interferes with the learning of others... Read more Buy for 145 rubles audiobook
| Organic personality disorder | |
| The frontal lobe of the brain (in red), when damaged, this syndrome occurs. | |
| ICD-10 | F |
| ICD-9 |
Organic personality disorder (personality disorder of organic etiology)
- a personality disorder caused by disease, damage or dysfunction of the brain.
About depression
I hate periods when I am a corpse, a vegetable. I can't get up, I can't eat, I can't talk. I just lie face down in the pillow. Every now and then my morale rises sharply for a few seconds, I pick up the phone to call/text one of my friends and drag myself out of the room. But this happens a couple of times a day and for a few seconds. Then I fall face first into the pillow and start bawling.
Tomorrow or the day after tomorrow I will wake up as if nothing had happened and begin to live the life of a successful, joyful person for the next week or two. And then everything will come back again. Or not.
18 hours of sleep. When a friend called me at one o'clock in the afternoon about a meeting, and I could not wake up normally, I already suspected something was wrong. I couldn’t go to the meeting, so I rescheduled it for the evening. Now I got up, went to the kitchen... and burst into tears because I ran out of coffee. I'm broken.
Clinical picture
Organic personality disorder is characterized by significant changes in the pattern of behavior habitual before the illness. Drives, needs and expression of emotions are impaired. Cognitive performance is usually reduced in the areas of anticipation and planning, similar to the impairments in frontal lobe syndrome.
This disorder can manifest itself as a personality syndrome in limbic epilepsy, as a consequence of a lobotomy, after a leucotomy, damage to the frontal lobes of the brain (or damage to other surrounding areas of the brain).
The development of a characteropathic variant of psychoorganic syndrome with organic brain damage is classified as pseudopsychopathy[1].
With the frontal lobe syndrome of the frontal variant, dissocial personality disorder develops. ADHD and other behavioral disorders may occur in childhood.
Diagnostics
The diagnostic criteria of the International Classification of Diseases, 10th Revision (ICD-10) require the presence of 2 or more of the following features:[2]
- significantly reduced ability to cope with goal-directed activities, especially those that require a long time and do not quickly lead to success;
- altered emotional behavior, characterized by emotional lability, superficial unjustified fun (euphoria, inappropriate playfulness), which is easily replaced by irritability, short-term bouts of anger and aggression. In some cases, the most striking feature may be apathy;
- expressions of needs and drives may arise without regard to consequences or social conventions (the patient may commit antisocial acts, such as theft, make inappropriate sexual demands, exhibit gluttony, or fail to observe personal hygiene);
- cognitive impairment in the form of suspicious or paranoid thoughts or excessive preoccupation with a single, usually abstract topic (such as religion, “right and wrong”);
- pronounced changes in the pace and flow of speech production, with features of random associations, over-inclusion (expanded inclusion of side associations in the topic), viscosity and hypergraphia;
- altered sexual behavior (hyposexuality or change in sexual preference).
Statistical data
It occurs in 1-3% of US adults, of whom 75% are women. 50-70% of patients with this disorder are found to abuse alcohol or drugs.
An important sign of the disorder is suicidal or self-harming behavior, the percentage of completed suicides is about 28-30%.
A common feature of the disorder is multiple low-risk suicide attempts due to minor incidents, and in rare cases, dangerous suicide attempts attributed to comorbid depression. As a rule, the trigger for attempts is interpersonal situations.
Etiology
ICD-10 provides an indication of the cause of personality disorder:
- due to traumatic brain injury (F07.00)
- in connection with vascular disease of the brain (F07.01)
- in connection with epilepsy (F07.02)
- due to brain tumor (F07.03)
- in connection with HIV infection (F07.04)
- in connection with neurosyphilis (F07.05)
- in connection with other viral and bacterial neuroinfections (F07.06)
- in connection with other diseases (F07.07)
- due to mixed diseases (F07.08)
- due to an unspecified disease (F07.09).
- due to complicated diabetes mellitus
Literature
- Alexei Franulic, Elizabeth Horta R.
Organic personality disorder after traumatic brain injury: cognitive, anatomic and psychosocial factors. A 6 month follow-up (English) // Brain Injury : journal. - 2009. - Vol. 14. - doi:10.1080/026990500120538.
>ICD-10 Personality DisordersSpecific This page was last edited on March 21, 2021 at 08:49 pm. Sources used:
- https://cmzmedical.ru/zabolevaniya/emotsionalno-neustoychivoe-rasstroystvo-lichnosti/
- https://probolezny.ru/pogranichnoe-rasstroystvo-lichnosti/
- https://millitary_psychology.academic.ru/709/neuro-psychological_instability
- https://psychology_pedagogy.academic.ru/21209/emotional_instability
- https://wiki2.org/ru/organic_personality_disorder