Meningitis is a severe infectious inflammatory disease of the membranes of the brain and/or spinal cord. The causative agent of meningitis can be bacteria, viruses, pathogenic fungi and some protozoa. The disease has a clear clinical picture (high fever, headache), and if it occurs, you should immediately consult a doctor. With modern medical treatments, meningitis is highly treatable.
However, it is very important to seek medical help immediately, as the disease has a high tendency to progress and can lead to serious consequences and death of the patient. When the first signs of meningitis appear, you can seek help at the Yusupov Hospital. Experienced doctors will quickly diagnose and begin treatment. A timely visit to the hospital will save time and avoid serious consequences.
Symptoms
Prognosis for a diagnosis of meningitis depends on the timeliness of diagnosis and initiation of treatment. The first signs of the disease are:
- headache;
- a sharp increase in body temperature;
- attacks of nausea and vomiting. In this case, after vomiting, the patient does not experience relief;
- numbness of the muscles in the neck;
- feeling of weakness and general malaise;
- lethargy, agitation. Sometimes hallucinations may appear;
- lack of appetite;
- diarrhea.
These symptoms include the following:
- feeling of pressure in the eye area;
- pain when pressing in the eyebrow area, under the eye or in the trigeminal nerve area;
- inflammation of the lymph glands;
- Brudzinski's symptom - when tilting the head or pressing on various parts of the body, legs and other parts of the body move reflexively;
- Kernig's symptom - the legs at the knee joint stop extending due to tension in the posterior thigh muscles;
- Bekhterev's symptom - when tapping on the zygomatic arch, the facial muscles contract;
- Mendel's symptom - the occurrence of pain when pressing on the area of the external auditory canal;
- Pulatov’s symptom – when the skull is tapped, the patient experiences pain;
- Lesage's symptom - in young children the large fontanelle is tense and pulsating. If you take the baby under the armpits, he throws his head back and reflexively presses his legs towards his stomach.
Nonspecific symptoms of meningitis can also be identified, including:
- body muscle spasms;
- increased blood pressure;
- hearing loss;
- impaired visual function – possible double vision, strabismus, ptosis, nystagmus;
- runny nose, cough, sore throat;
- bradycardia and tachycardia;
- increased irritability;
- drowsiness.
Diagnostics
Before treating meningitis, the doctor must find out the etiology of the disease. For this purpose, additional research is prescribed:
- general blood test - to identify inflammatory changes;
- general urinalysis - severe meningitis and sepsis can lead to kidney damage;
- spinal puncture with examination of cerebrospinal fluid;
- biochemical blood test - to determine the degree of damage to internal organs;
- bacteriological culture of mucus from the nasopharynx to identify meningococcus, pneumococcus;
- bacteriological examination of cerebrospinal fluid and blood - if purulent meningitis is suspected;
- stool tests to detect enteroviruses and polio viruses (PCR);
- A blood test to determine the acid-base balance and coagulation system is prescribed for severe meningitis and infectious-toxic shock.
In addition, the doctor may need the results of other studies:
- electrocardiograms of the heart - in case of serious condition of the patient and symptoms of damage to the heart muscle;
- chest x-ray - if pneumonia is suspected, which often accompanies pneumococcal meningitis.
Make an appointment
Treatment
Doctors at the Yusupov Hospital adhere to the principles of treating patients with meningitis, which include preventing further spread of the pathological process and preventing the development of complications. Neurologists take an individual approach to the treatment of each patient. Complex therapy includes:
- etiotropic treatment (destruction of bacteria that cause inflammation of the meninges);
- detoxification therapy;
- measures aimed at reducing intracranial pressure;
- anti-inflammatory therapy with corticosteroid hormonal drugs;
- treatment of intracranial and extracranial complications;
- relief of convulsive syndrome;
- normalization of body temperature.
Antibiotics for meningitis in adults at the prehospital stage are used only in cases where emergency delivery of the patient to the Yusupov Hospital is impossible for some objective reason within 2.5 or 3 hours.
The introduction of antibiotics for meningitis at an earlier time (up to 60 minutes) is justified only if there is a strong suspicion of the meningococcal nature of the disease when the symptoms of meningitis are combined with hemorrhagic rashes that do not disappear with pressure. Antibiotics for bacterial purulent meningitis are administered only parenterally. Antibacterial tablets are not effective for meningitis. If the meningococcal nature of the disease is suspected, antibiotics for meningitis are administered only against the background of established anti-shock therapy in the presence of vascular access due to the high risk of impaired blood supply to tissues and the development of acute adrenal insufficiency against the background of low blood pressure.
At the prehospital stage of treatment of meningitis, third generation cephalosporins are administered. Penicillin for meningitis in this case is less effective, since in Russia there is no mandatory vaccination against Haemophilus influenzae and a hemorrhagic rash can be a manifestation of meningitis caused by Haemophilus influenzae, which is insensitive to penicillin. If there is information about severe allergic reactions in the patient to beta-lactam antibiotics, sodium chloramphenicol succinate (chloramphenicol) is administered. The administration of an antibiotic is not a reason to delay hospitalization of the patient.
For patients with bacterial purulent meningitis, empirical antibacterial therapy begins no later than an hour after admission to the neurology clinic. If the patient has contraindications to immediate lumbar puncture, antibiotics for meningitis begin to be administered immediately after collecting a blood sample for bacteriological examination. If the patient’s condition is stable, there are no contraindications to cerebrospinal puncture, and it is possible to obtain cerebrospinal fluid within one hour of the patient’s admission to the neurology clinic, antibacterial therapy begins after a cystoscopic examination of Gram-stained cerebrospinal fluid smears.
When empirically selecting antibiotics for patients suffering from meningitis, neurologists take into account:
- patient's age;
- conditions preceding the disease (developmental defects, trauma, neurosurgical interventions, immunodeficiency states, cochlear implantation);
- availability of vaccination against meningococcus, Haemophilus influenzae, pneumococcus;
- the possibility of contact with infectious patients;
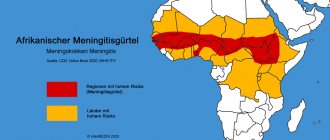
- staying in countries with a high incidence of bacterial meningitis;
- regional characteristics of pathogens causing neuroinfectious diseases.
Antibiotics for meningitis of unknown cause
In the presence of an unfavorable background preceding meningitis, newborns and children under one month are prescribed the following antibiotics for meningitis: ampicillin and an aminoglycoside (gentamicin) or cefotaxime.
If the pneumococcal nature of the disease is suspected, the use of vancomycin is indicated. In children from 3 months to 18 years of age, meningitis is caused mainly by pneumococci, Haemophilus influenzae, and meningococci. Patients are prescribed antibiotics that belong to the third generation cephalosporins (cefotaxime or ceftriaxone). If the pneumococcal nature of meningitis is suspected, if strains of bacteria resistant to cephalosporins are present in the region, vancomycin or rifampicin is added to the treatment regimen. If a patient develops meningitis due to a skull fracture, the cause of inflammation of the meninges may be pneumococci, Haemophilus influenzae, or β-hemolytic streptococcus. In this case, neurologists at the Yusupov Hospital use a combination of third-generation cephalosporins with vancomycin.
In case of penetrating head trauma, after neurosurgical interventions, the causative agents of meningitis are Staphylococcus aureus, aerobic gram-negative bacteria. They are most sensitive to the combination of vancomycin with cefepime, ceftazidime or meroneme. If meningitis develops after shunt placement, the same combinations of antibiotics are effective.
At the onset of meningitis, similar symptoms (impaired consciousness, convulsions, fever, meningeal symptoms) and the results of cerebrospinal fluid examination (mixed pleocytosis) do not exclude viral encephalitis. Doctors at the Yusupov Hospital prescribe acyclovir intravenously in all doubtful cases, pending the results of the final examination of the patient, along with antibacterial therapy. After laboratory tests and clarification of the nature of meningitis, antibiotic therapy is adjusted.
Antibiotic therapy for established meningitis pathogens
If, when examining the cerebrospinal fluid obtained during the first lumbar puncture, laboratory technicians identify the causative agent of meningitis, doctors at the Yusupov Hospital prescribe antibiotics to which the identified microorganisms are sensitive.
Cefotaxime, ceftriaxone, and penicillin act on meningococci. Alternative antibacterial drugs are the antibiotics meronem and chloramphenicol. With the development of septic shock and multiple organ failure, doctors give preference to cephalosporins. The main antibiotics that doctors prescribe to treat patients with pneumococcal meningitis are cefotaxime and ceftriaxone. Cefepime, meronem and chloramphenicol are used as reserve antibiotics. When penicillin-resistant strains circulate in the region, combination antibiotic therapy with third-generation cephalosporins in combination with vancomycin or rifampicin is prescribed.
Haemophilus influenzae type b is not sensitive to penicillin. If it is the cause of meningitis, neurologists prescribe ampicillin, cefotaxime, ceftriaxone or chloramphenicol. Cefepime or meronem are used as alternative antibiotics. Streptococci serotype B are sensitive to the antibiotic cefotaxime. Neurologists at the Yusupov Hospital individually select doses and frequency of antibiotic administration depending on the patient’s age. For cryptococcal meningitis, 5-flucytosine and amphotericin B are used, and for tuberculosis meningitis, pyrazinamide, rifampicin, isoniazid and ethambutol are used.
The duration of antibacterial therapy is determined individually for each patient, depending on the cause of meningitis, the characteristics of the course of the disease and the presence of complications. The average duration of antibiotic therapy, depending on the causative agent of meningitis with an uncomplicated course of the disease, is as follows:
- meningococcal meningitis – 7 days;
- hemophilic – from 7 to 10 days;
- pneumococcal – from 10 to 14 days;
- listeria – 21 days;
- streptococcal (group B) – 14 days.
For bacterial meningitis caused by gram-negative enterobacteriaceae or Pseudomonas aeruginosa, antibiotics are administered for 21 days. Antibiotics are discontinued when the symptoms of meningitis completely reverse and cerebrospinal fluid levels return to normal. For meningococcal meningitis, antibiotic therapy is stopped if there are no infectious agents in the cerebrospinal fluid and nasopharyngeal swabs.
Complex treatment of meningitis
In addition to antibiotics for meningitis, doctors at the Yusupov Hospital prescribe glucocorticoids to patients.
Dexamethasone is administered before starting antibiotic therapy or simultaneously with the first dose of antibiotic. If there are indications for prescribing dexamethasone after starting antibiotic treatment, it is administered in the first 4 hours after injection of the antibacterial drug. Dexazone is not prescribed later than 12 hours from the start of antibiotic therapy for meningitis. When prescribing glucocorticoids, neurologists take into account that, by reducing the severity of inflammatory changes in the meninges, they help reduce the permeability of the blood-brain barrier to antibacterial drugs and lead to a decrease in the concentration of antibiotics in the subarachnoid space. This fact is especially taken into account when using vancomycin in patients with pneumococcal meningitis. Long-term use of glucocorticoids in patients with meningitis leads to suppression of the immune system and can cause the development of secondary bacterial complications and activation of viral infections. For signs of septic shock and manifestations of acute adrenal insufficiency, glucocorticoids are also prescribed.
Detoxification therapy is prescribed to maintain circulating blood volume and adequate blood supply to brain tissue. When conducting infusion therapy, doctors use isotonic solutions of sodium chloride, glucose or dextrose, Ringer's solution. All patients with meningitis at the Yusupov Hospital are monitored for blood glucose levels at least once a day.
If there are signs of shock, sodium chloride is administered as an emergency intravenous bolus over 5-10 minutes. If symptoms persist or progress, 0.9% sodium chloride solution or 5% human albumin is reintroduced. If symptoms continue to persist after administration of fluid in a volume of 40 ml/kg, a third injection of 0.9% sodium chloride or 5% human albumin is administered over 5-10 minutes. If the measures taken are ineffective, the patient is immediately transferred to artificial ventilation, vasoactive drugs are added, and infusion therapy is continued.
For infusion therapy with an increasing increase in intracranial pressure and the threat of developing cerebral edema, a mannitol solution is used, followed by the administration of furosemide to prevent “recoil” syndrome. If seizures develop, patients are given diazepam or midozal. If convulsive status develops, valproates (Convulex, Depakine) are used. If epileptic activity persists, patients are connected to a ventilator and sodium hydroxybutyrate or sodium thiopental is administered. For the purpose of immunocorrection, intravenous immunoglobulins enriched with IgM - pentaglobin - are used. They are effective on the first day of the disease. If patients develop acute renal failure, plasmapheresis sessions are performed.
You can undergo a course of adequate treatment of meningitis with antibiotics by first making an appointment and calling the Yusupov Hospital. The clinic’s doctors individually select an antibacterial therapy regimen and use antibiotics that have a minimal range of side effects. Timely adequate treatment with antibiotics can prevent complications of meningitis.
Prevalence, etiology and general treatment approaches
Infections of the upper respiratory tract (URT) and ENT organs are among the most common diseases. In the structure of overall morbidity in Moscow, they account for approximately 19% and are in second place among all pathologies [1].
Approximately 5–15% of adults and 5% of children suffer from some form of sinusitis [1]. In Russia, about 10 million people suffer from acute sinusitis annually [2], and at least 80% of them are people of working age [3]. It is also one of the most widespread diseases in children.
The share of acute otitis media in the structure of diseases of the ENT organs accounts for 20–30% [4, 5]. In Europe, its incidence in the adult population is 1–5% per year [6]. In the United States, acute otitis media occurs annually in 10 million people [5], affecting about 14% of the population [7]. During the first year of life, 62% of children experience at least one episode of the disease; by the age of two to three years – 80–94% [8, 9]. Acute otitis media occupies a leading position in the structure of seeking medical care in pediatrics, accounting for 33% of all doctor visits [8,9].
The main clinical manifestation of tonsillopharyngitis is a sore throat, which is observed in an adult on average two to three times a year [10]. Pharyngitis caused by group A beta-hemolytic streptococcus is one of the most common bacterial infections in children under two years of age. Chronic tonsillitis occurs in 2–3% of children aged 3 years, 6.5% – 5–6 years old, 12–13% – 10–12 years old, and 25–35% of people aged 18–20 years [11]. Its prevalence among frequently ill children aged 2–6 years reaches 43% [12].
Infections of the upper respiratory tract and ENT organs are potentially dangerous in terms of the development of serious complications and deaths, the risk of which increases significantly in the case of irrational treatment of the primary disease. Thus, tonsillitis and pharyngitis can be complicated by infections of neighboring organs (otitis media, sinusitis, bronchitis), and also cause severe regional complications (peritonsillar, lateral pharyngeal and retropharyngeal abscesses, etc.), requiring emergency surgical interventions, and systemic complications - rheumatism, glomerulonephritis, vasculitis, etc. Acute otitis media is one of the leading causes of meningitis, brain abscess and thrombosis of the asigmoid sinus [4]. Sinusitis can lead to the development of severe orbital and intracranial complications.
Infections of the upper respiratory tract and ENT organs are also associated with significant financial losses. For example, in the USA, direct and indirect costs associated with acute otitis media exceed $3.5 billion per year [13], and $3.5 billion is spent annually on the treatment of acute bacterial sinusitis [14], including in children up to 12 years – 1.8 billion [15]. In Russia, the average duration of temporary disability for acute sinusitis is 11.6 days [16]. Economic losses caused only by temporary disability are estimated at 232 million US dollars, or 0.15% of the gross domestic product of the Russian Federation [16]. Thus, the correct choice of treatment for infections of the upper respiratory tract and ENT organs is, along with clinical, of great economic importance. Adequate treatment of these infections is also an important factor in the prevention of bacterial resistance.
Unfortunately, the widespread increase in the resistance of the main causative agents of infections of the upper respiratory tract and ENT organs to many antibacterial agents, including first-line drugs, significantly limits the choice of antibiotics for empirical therapy. For example, the spread of beta-lactamase-producing strains of H. influenzae and M. catarrhalis and the emergence of penicillin-resistant pneumococci are already calling into question the legality of using amoxicillin as a first-line drug for acute otitis media and other community-acquired infections [17].
In addition, in recent years there have been changes in the etiological structure of infections of the upper respiratory tract and ENT organs, which necessitates a revision of approaches to the management of patients with infections of this localization. First of all, this is due to the increasing role of “atypical” bacterial pathogens (M. pneumoniae, C. pneumoniae) in the etiology of acute respiratory diseases (ARI), laryngotracheitis and other respiratory tract infections, especially in young people and children [18]. For example, in a randomized study whose participants included 353 children aged 1 to 14 years with recurrent acute respiratory infections and 208 healthy children (control group), “atypical” pathogens were identified in 54% of patients in the main group compared to 3.8% children from the control group (p < 0.0001) [18]. This study also showed that short-term (within a month) and long-term (within six months) clinical benefit was observed significantly more often in patients receiving azithromycin along with symptomatic therapy than in children receiving symptomatic therapy alone. Moreover, the long-term clinical effect of azithromycin (reduction in the frequency of relapses) was expressed in infections caused not only by “atypical” pathogens, but also by other pathogens. The results of the study led to the conclusion that “atypical” bacteria play a fairly large role in the occurrence of recurrent respiratory tract infections in children and that long-term therapy with azithromycin can not only significantly improve the course of an acute episode of the disease, but also reduce the risk of relapses.
Another recent study showed that, if not adequately treated, acute tonsillopharyngitis in children associated with atypical bacteria can lead to unfavorable outcomes and is associated with a high risk of relapse [19]. These data make us more critical of modern recommendations, which do not support the use of antibiotics in most patients with acute infections of this localization, and contribute to increasing the role of macrolides in their therapy.
Currently, azithromycin has actually already acquired the status of a first-line antibiotic for the treatment of infections of the respiratory tract and ENT organs, despite the fact that in most recommendations it is given the position of a drug alternative to beta-lactams [20]. This is due to the favorable pharmacological properties of azithromycin, proven effectiveness and safety, and the increasing etiological role of atypical pathogens.
Rationale for the feasibility of using azithromycin for infections of the respiratory tract and ENT organs from a pharmacological point of view
Like other macrolides, azithromycin is active against the main causative agents of infections of the respiratory tract and ENT organs (S. pneumoniae, S. pyogenes, M. catarrhalis), including atypical pathogens (mycoplasma, chlamydia). Its advantage over other macrolides is its clinically significant activity against the common causative agent of acute otitis media and acute bacterial sinusitis, H. influenzae. Like other macrolides, azithromycin has a bacteriostatic effect, but due to its unique pharmacokinetic properties it is capable of creating very high interstitial and intracellular concentrations and, accordingly, has a bactericidal effect, including on pathogens located inside cells [21].
Azithromycin is characterized by post-antibiotic effects against S. pyogenes, S. pneumoniae, H. influenzae, L. pneumophila. In terms of the duration of the post-antibiotic effect against a number of microorganisms, for example, H. influenzae and Legionella pneumophila, it is superior to clarithromycin [22, 23]. The effect of azithromycin is enhanced by its anti-inflammatory and immunomodulatory properties [24].
Azithromycin differs from erythromycin and other macrolides in improved pharmacokinetic properties: it is superior to other antibiotics of this group in acid resistance (300 times higher than erythromycin), is more consistently absorbed from the gastrointestinal tract and has greater bioavailability. The high lipophilicity of azithromycin determines its wide distribution in the body (volume of distribution - 31 l/kg) and good penetration into tissues and biological fluids. Its concentrations in various tissues after a single administration are 20–1000 times higher than those in blood plasma [25, 26]. Very high concentrations of the drug are created in the respiratory tract and ENT organs: in bronchial secretions, lungs, alveolar fluid, tonsils, adenoids, middle ear and paranasal sinuses [27, 28]. They far exceed the minimum inhibitory concentrations of the antibiotic for the most common pathogens that cause infections in the corresponding localization.
Azithromycin is significantly superior to erythromycin in its ability to penetrate into the paranasal sinuses [29]. Its maximum concentrations in the mucous membrane of the maxillary sinus are created within two hours after administration and significantly exceed the level of the antibiotic in the blood serum. Research conducted at the L.S. Strachunsky showed that two hours after taking 500 mg of azithromycin, its concentrations in the mucous membrane of the maxillary sinus were eight times higher than those in the blood serum, while the maximum concentrations of erythromycin were approximately three times lower than serum concentrations [30]. In a placebo-controlled study in animals with experimental rhinosinusitis, azithromycin, creating high concentrations at the site of infection, ensured rapid clearance of bacteria and disappearance of inflammation [31]. In contrast, the new fluoroquinolone with bactericidal action, moxifloxacin, which creates low concentrations in the lesion and has a short post-antibiotic effect, had little effect on bacterial clearance and the inflammatory process [31].
Azithromycin very quickly reaches high concentrations in the tonsils and adenoids. 2–24 hours after administration, its concentrations in the tonsils exceed the MIC for S. pyogenes by 30 times [30]. The half-life of azithromycin from tonsil tissue reaches 3.2 days [32]. In children aged two to eight years who received a three-day course of treatment with an azithromycin suspension at a dose of 10 mg/kg/day, the level of the antibiotic in the tonsils and adenoids four days after completion of therapy was more than 900 times higher than its serum concentrations [26]. In patients with recurrent or chronic tonsillitis, after oral administration of azithromycin at a dose of 250 mg twice daily, high concentrations of the drug in the tonsils persisted for seven days [26].
High levels of azithromycin are detected in the mucous membranes of the ethmoid sinus and in the tympanic cavity [26]. In children with otitis media, within 24 hours after the start of therapy, azithromycin concentrations in the middle ear reach 8–9 mg/kg [33].
Data on antibiotic concentration levels in the respiratory tract and ENT organs obtained in pharmacokinetic studies are summarized in the table.
Azithromycin is metabolized to a small extent with the formation of inactive metabolites [36]. The drug is excreted primarily in bile. Elimination of azithromycin has a biphasic nature, the half-life from the body is 35–79 hours [37, 38] and does not change with renal and liver failure and cirrhosis of the liver [39, 40].
Favorable pharmacokinetic properties make it possible to take azithromycin once a day in short courses of three to five days, and for some infections even as a single dose. No significant differences in the pharmacokinetics of the antibiotic (accumulation in macrophages, tissue and cellular concentrations) were found when using three- and five-day courses of treatment [41].
The unique regimen of azithromycin provides it with advantages over other antibiotics in terms of patient adherence to therapy. This is facilitated by the possibility of using it regardless of food intake. Although azithromycin is recommended to be taken before meals, several targeted studies have demonstrated that food does not significantly affect the bioavailability of this antibiotic in various dosage forms [42]. The advantage of azithromycin in pediatrics is the favorable organoleptic properties of the pediatric suspension of the drug [43, 44].
Azithromycin is well tolerated. Adverse reactions with its use rarely develop. The incidence of adverse drug reactions in adults and children is about 9% [45], while with erythromycin treatment it reaches 30–40% [46]. Serious adverse reactions with the use of azithromycin in clinical studies were recorded extremely rarely, and their cause-and-effect relationship with the drug has not been definitively established. According to the results of meta-analyses, the rate of azithromycin discontinuation due to adverse reactions is 0.7% for lower respiratory tract infections and 0.8% for upper respiratory tract infections [47, 48].
Azithromycin has low allergenic potential. Allergic reactions are observed in less than 1% of patients, while when treated with penicillins they develop in 10% of cases, and with cephalosporins in 4% [46]. The most common side effects are azithromycin dyspeptic disorders, the incidence of which, according to several controlled clinical studies, ranges from 6 to 9% [49]. Thus, in pediatric clinical studies, diarrhea was observed in 1–6% of participants, abdominal pain in 1–4%, nausea in 0.5–2%, and vomiting in 1–6%. Elevated liver enzyme levels occurred in 0–1% of children receiving azithromycin versus 2–4% of children receiving erythromycin [49].
The absence of a pronounced effect on the enzymes of the cytochrome P450 system in the liver provides azithromycin with a low potential for clinically significant drug interactions, which determines its fairly high safety when used in combination with other drugs. In this indicator, azithromycin is superior to most macrolides, which, in terms of their effect on cytochrome P450, are arranged in the following order: clarithromycin > erythromycin > roxithromycin > azithromycin > spiramycin [50].
The use of azithromycin is quite safe during pregnancy. It is the only semi-synthetic macrolide classified by the FDA as category B. This category includes drugs that do not have an adverse effect on the fetus and the course of pregnancy in animal experiments. There are also clinical data confirming the safety of azithromycin in pregnant women [29].
The use of macrolides for empirical treatment of infections of the respiratory tract and ENT organs is also justified from the point of view of the low level of resistance to them in common pathogens of this localization in Russia. According to the multicenter study PeGaS-1 (2000), the frequency of pneumococcal resistance to azithromycin is 5%, to erythromycin – 6%, to clarithromycin – ranges from 2 to 13% [24]. Moreover, according to Japanese authors, azithromycin remains active against pneumococci resistant to other macrolides [51]. “Overcoming” the low level of resistance of microorganisms is apparently associated with the pharmacokinetic properties of azithromycin.
Evidence of the effectiveness of azithromycin for infections of the upper respiratory tract and ENT organs
The high effectiveness of azithromycin for infections of the upper respiratory tract and ENT organs in adults and children has been proven in controlled clinical studies. Between 1991 and 2001, the effectiveness of azithromycin in infections of the upper respiratory tract and ENT organs was studied in at least 29 randomized clinical trials, which included 7240 patients, including 4263 children [52]. Along with five-day courses of treatment, shorter treatment regimens have also been studied to improve adherence to treatment and reduce its cost. Three-day courses of azithromycin therapy were compared with 7–14-day courses of clarithromycin, roxithromycin, phenoxymethylpenicillin, amoxicillin/clavulanate, and cefaclor. In most studies, a short course of azithromycin was not inferior in clinical and bacteriological effectiveness to standard courses of comparator drugs, and in some it was even superior to them.
Currently, azithromycin is the only antibiotic approved by the FDA for short-term use in acute bacterial sinusitis. The basis for approval was the results of a multicenter, randomized, double-blind trial involving 936 patients [53]. It compared the effectiveness and safety of two treatment regimens: azithromycin 500 mg once daily for 3 or 6 days and amoxicillin/clavulanate 625 mg 3 times daily for 10 days. The effectiveness of all treatment regimens was the same, however, when treating with amoxicillin/clavulanate, side effects were observed more often (51.1%) than when using 3-day (31.1%; p < 0.001) or 6-day courses of azithromycin (37.6 %; p < 0.001). There were also more patients in the amoxicillin/clavulanate group who dropped out of the study (n = 28) due to side effects than in the azithromycin groups (n = 7 and 11, respectively, for the 3- and 6-day courses).
The comparable effectiveness of three-day courses of azithromycin with standard courses of treatment with amoxicillin/clavulanate was confirmed in three more clinical studies, and in two of them the effect of azithromycin developed faster than the effect of the comparison drug. The results of a domestic randomized clinical and pharmacoeconomic study showed that a three-day course of azithromycin provides cure for acute sinusitis in a shorter period of time than a ten-day course of amoxicillin/clavulanate, more effectively prevents relapses of the disease, is better tolerated, is characterized by fewer adverse reactions than the comparison drug, and is more profitable from an economic point of view [54].
Controlled studies have demonstrated the high clinical and bacteriological effectiveness of azithromycin for tonsillopharyngitis in adults and children. It has been shown that azithromycin is not inferior in clinical effectiveness to phenoxymethylpenicillin and erythromycin. There is evidence of faster relief of symptoms of the disease in patients receiving three- and five-day courses of azithromycin, compared with patients receiving a standard course of phenoxymethylpenicillin and roxithromycin [55, 56]. At the same time, some studies have revealed a lower bacteriological effectiveness of azithromycin compared to phenoxymethylpenicillin [57–59] and a higher rate of disease relapses in the long term in patients treated with azithromycin [60, 61]. This may be due to the insufficient dose of azithromycin used in these studies.
A meta-analysis of controlled clinical trials showed that the effectiveness of azithromycin for tonsillopharyngitis largely depends on the dose and treatment regimen [58]. In children, the course dose of the drug should be 60 mg/kg (3 days at 20 mg/kg or 5 days at 12 mg/kg). According to the results of the meta-analysis, at this course dose, azithromycin was significantly (p < 0.00001) superior in effectiveness to 10-day courses of treatment with comparison antibiotics. Moreover, bacteriological failure in children receiving azithromycin at a course dose of 60 mg/kg was observed five times less often than when using ten-day courses of comparison antibiotics. On the contrary, at a course dose of 30 mg/kg, azithromycin was inferior (p = 0.02) in effectiveness in pediatrics to standard courses of comparison antibiotics. In children, three-day treatment regimens were less effective than five-day ones. In contrast, in adult patients, three-day treatment regimens were superior to five-day regimens. When using three-day treatment regimens (500 mg/day) in adults, there was a trend towards higher efficacy of azithromycin compared with ten-day courses of comparison antibiotics (p = 0.14).
The only clinical study used a single dose of azithromycin (30 mg/kg) in patients with tonsillitis, which was not inferior in effectiveness to a ten-day course of treatment with a comparator antibiotic [62], but the question of the possibility of using a single dose of azithromycin for the treatment of acute tonsillopharyngitis requires further study.
Azithromycin has proven to be an effective treatment for acute otitis media. It has been shown to be effective in three- and five-day courses in clinical studies, and in 2003 it was approved by the FDA for the treatment of acute otitis media in children in a single dose.
The effectiveness and safety of a single dose of azithromycin (30 mg/kg) have been studied in a fairly large number of clinical studies in children with uncomplicated acute otitis media. The summarized results of four studies indicate that, in general, the clinical effectiveness of a single dose of azithromycin in children with acute otitis is 84%, including for infections caused by Streptococcus pneumoniae - 91%, Haemophilus influenzae - 77%, Moraxella catarrhalis - 100 %, Streptococcus pyogenes – 64%, mixed infection of S. pneumoniae and H. influenzae – 25% [63]. The drug was very well tolerated: side effects were rare and mainly manifested as mild transient gastrointestinal disorders. In the two largest studies, the incidence of side effects with azithromycin was lower than that of the comparator antibiotics amoxicillin and amoxicillin/clavulanate.
According to the results of a meta-analysis, the frequency of failure when using short (less than five days) courses of azithromycin and 7-10-day courses of amoxicillin does not differ [64]. At the same time, azithromycin is significantly less likely (19%; p < 0.05) to cause side effects than amoxicillin.
Thus, azithromycin meets almost all the requirements for “ideal” drugs for the treatment of infections of the upper respiratory tract and ENT organs:
· exhibits high activity against the main pathogens of infections in a given localization, including “atypical” pathogens, the etiological role of which has recently been increasing;
· has favorable pharmacokinetic properties, allowing one to achieve high concentrations of the antibiotic at the site of infection and apply it once a day in short courses;
· has proven efficacy and safety in adequate clinical studies and is well tolerated by patients;
· thanks to the convenient treatment regimen and good tolerability, it allows for high patient adherence to treatment;
· is associated with low levels of resistance in major pathogens and may “overcome” low levels of resistance due to unique pharmacokinetic properties.
Rehabilitation
Patients at the Yusupov Hospital who have had meningitis require observation by a neurologist for the next 2 years.
Regular examination in the first year should be carried out once every 3 months, then once every 6 months. Recovery from meningitis is complex, complex and multifaceted. One of the components of the rehabilitation period after meningitis is a diet aimed at restoring the patient’s strength without causing irritation to the gastrointestinal tract. The preferred methods of cooking are boiling, including steaming, stewing, and baking. It is recommended to eat lean meat: rabbit, chicken, veal, lean fish. Vegetables and fruits must be heat-treated to prevent irritation of the sensitive mucous membrane by coarse fiber. Consumption of dairy products is necessary to further enrich the body with protein. Patients are recommended to drink jelly, compotes, and weak tea.
Physiotherapy plays an important role in restoring the body of a patient who has suffered meningitis. Doctors at the Yusupov Hospital prescribe classical massage and various hardware techniques. Electrophoresis of vitamins and medications helps relax or stimulate the desired muscle groups. Patients with coordination and cognitive impairments are prescribed the use of electrosleep, magnetic therapy, and magnetic laser therapy to restore central nervous system functions. The selection of individual physiotherapeutic techniques aimed at treating the consequences of meningitis at the Yusupov Hospital is carried out by qualified physiotherapists, depending on the patient’s condition.
A separate and extensive area of recovery after meningitis is physical therapy. Qualified physical therapy doctors at the Yusupov Hospital develop individual programs for patients to help restore movement skills.
The everyday adaptation of patients is provided with the help of occupational therapy. This complex technique is aimed at restoring the amplitude, strength and coordination of movements.
Cognitive therapy helps restore attention, memory and logical thinking.
Rehabilitation after meningitis is a long and painstaking process, the effectiveness of which requires the experience and knowledge of doctors, which the specialists of the Yusupov Hospital fully possess, as well as the perseverance, consistency and patience of patients.
General recovery regimens are aimed at relieving symptoms, improving function and overall well-being of the patient. In addition, they help improve motor, sensory, cognitive and behavioral function.
The Yusupov Hospital in Moscow is a modern multidisciplinary clinic that offers medical care and care services at the highest level. The Neurology Clinic of the Yusupov Hospital provides comprehensive diagnosis and treatment of meningitis using modern and high-precision equipment, which allows us to identify the disease at an early stage and select the most effective treatment regimen for each patient.
You can make an appointment for diagnosis and treatment with a doctor at the Yusupov Hospital, and find out the cost of the medical services provided by calling or visiting the clinic’s website. The coordinating doctor will answer all your questions.
Make an appointment
Features of use
There are several principles for the use of drugs from the group of antibiotics that require mandatory compliance. Violations of them can lead to serious consequences. The drug should always be prescribed by an otolaryngologist, and if not, then by a therapist.
1. At the initial visit, if it is not possible to wait for the results of the smear, a broad-spectrum drug is prescribed for treatment, effective against the main pathogens of the identified pathology. After the results of the study are received, the treatment regimen will be edited if necessary.
2. If there is no result, the drug must be replaced. In such a situation, a second smear may be necessary, since failure of treatment most likely means that a mistake was made in choosing the medicine. If the patient does not comply with the dosage regimen, then the lack of effect from the antibiotic is associated with the development of a drug-resistant form of the pathogen.
3. Minimum course duration is 7 days. Be sure to complete the treatment completely. Even if it seems that the medicine is no longer needed, you should definitely continue taking it. Otherwise, if the patient does not complete the course, it will cause the appearance of a particularly persistent pathogen, against which antibiotics from this category will be useless in the future.
4. When choosing a drug, it is necessary to study the patient’s chart in order to determine which antibiotic drugs have already been administered recently. In this case, you need to choose a different remedy, since the previous one may no longer be effective enough. It is highly undesirable to use the same drug several times in one year. This is allowed only if there is no other way out;
Also, the patient must inform the attending physician about what medications he is taking, since not all drugs can be combined with antibiotics. In this case, therapy is based on a special plan if it is not possible to stop the medication.
Complications
The disease is characterized by an acute course and begins with an increase in body temperature.
Patients complain of severe headaches and vomiting, which does not bring relief. The so-called meningeal syndrome is associated with one of the most obvious symptoms of meningitis - stiffness of the neck muscles. Patients develop drowsiness, photophobia, dizziness, and in some cases, convulsions and even loss of consciousness.
The most common and relatively harmless consequence of meningitis is asthenic syndrome, which manifests itself as causeless malaise, weakness, and low mood. It can last from 3 months to 1 year.
However, according to modern researchers, in 30% of patients who suffered meningitis, the disease caused the development of the following complications:
- intellectual disabilities;
- paresis, paralysis;
- loss of vision;
- hearing loss (sensorineural hearing loss);
- hydrocephalus;
- convulsive syndrome;
- ischemic stroke.
You can make an appointment for diagnosis and treatment with a doctor at the Yusupov Hospital, and find out the cost of the medical services provided by calling or visiting the clinic’s website.
The coordinating doctor will answer all your questions. Make an appointment
Infographic: the whole truth about meningitis
The colder it gets outside, the more often the classic “put on a hat or you’ll get meningitis” sounds. In reality, a hat has practically nothing to do with meningitis - no headdress can protect against a dangerous infectious disease. Let's figure out what you need to know about meningitis, and also find out what common misconceptions about this disease we encounter regularly.
What is meningitis?
Meningitis is an inflammatory process that affects the membranes of the spinal cord and/or brain. Inflammation is caused by pathogenic microorganisms - bacteria, viruses, fungi and even protozoa.
The most common (and least dangerous) is viral meningitis, which is often a complication of influenza, measles, mumps and other viral diseases. The peak of its distribution is late summer and autumn.