Organic damage to the central nervous system (CNS) is a diagnosis that indicates that the human brain is in an unstable state and is considered defective.
As a result of such lesions in the brain, degenerative disorders occur, destruction and death of brain cells or their necrosis. Organic damage is divided into several stages of development. The first stage is characteristic of most ordinary people, which is considered the norm. But the second and third require medical intervention.
Residual damage to the central nervous system is the same diagnosis, which shows that the disease appeared and persisted in a person during the perinatal period. Most often this affects infants.
From this we can draw an obvious conclusion. Residual organic damage to the central nervous system is a disorder of the brain or spinal cord that occurred while the child was still in the womb (at least 154 days from the date of conception) or within a week after his birth.
Mechanism of damage
One of all the “inconsistencies” of the disease is the fact that a disorder of this type belongs to neuropathology, but its symptoms may relate to other branches of medicine.
Due to an external factor, the mother experiences disruptions in the formation of the phenotype of cells that are responsible for the full list of functions of the central nervous system. As a result, fetal development is delayed. It is this process that can become the last link on the path to central nervous system disorders.
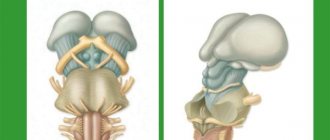
Regarding the spinal cord (this is also part of the central nervous system), corresponding lesions can appear as a result of incorrect obstetric care or inaccurate turns of the head when delivering the child.
Causes and risk factors
The perinatal period can also be called a “fragile period”, because during this time literally any unfavorable factor can cause the development of defects in the central nervous system of the infant or fetus.
For example, medical practice has cases that show that organic damage to the central nervous system is caused by the following reasons:
- hereditary diseases that are characterized by chromosome pathology;
- diseases of the expectant mother;
- violation of the birth calendar (long and difficult labor, premature birth);
- development of pathology during pregnancy;
- poor nutrition, lack of vitamins;
- environmental factors;
- taking medications during pregnancy;
- stress of the mother during pregnancy;
- asphyxia during childbirth;
- uterine atony;
- infectious diseases (and during lactation);
- immaturity of a pregnant girl.
In addition, the development of pathological changes can be influenced by the use of various dietary supplements or sports nutrition. Their composition can have a detrimental effect on a person with certain characteristics of the body.
Types of organic lesions and their causes
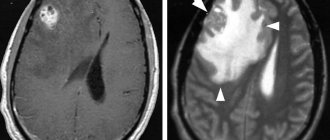
example of organic changes in the brain on MRI
Organic changes in the brain are varied not only clinically, but also in morphological expression. This may be a focus of necrosis resulting in a cyst after a cerebral infarction or hematoma, calcification after an infection, or foci of neuroglial proliferation - gliosis. Sometimes such changes do not manifest themselves at all and are accidentally discovered during an MRI, and then the neurologist most likely will not invent anything and make a diagnosis, so as not to complicate the life of a generally healthy person.
The conclusion about an organic lesion has the right to exist only with a combination of the morphological substrate and the corresponding symptoms, which would indicate that the lesions actually disrupt interneuronal connections and the function of the nervous tissue. It is advisable that the diagnosis be confirmed by CT or MRI.
An exception may be a long-term coma, up to 30 days or more, when there are no obvious signs of “organic” on MRI, but the duration of metabolic and hypoxic changes suggests diffuse organic damage to the nervous tissue.
The causes of organic brain damage can be:
- Acute vascular disorders with obstruction of the bloodstream or rupture of feeding vessels - intracerebral hematoma, infarction (strokes), subarachnoid hemorrhage - most often result in the formation of a single or several cysts filled with cerebrospinal fluid, and the symptoms are determined by the location and size of the cystic cavity;
- Intrauterine infections and intoxications, brain developmental defects, birth injuries and deep perinatal hypoxia are the causes of organic damage in early childhood;
- Parkinson's disease, in which damage to subcortical structures occurs with characteristic symptoms of movement disorders;
- Organic damage due to parasitic infestations, brain injury with disruption of its integrity, tumor, post-stroke cyst, accompanied by convulsions and psychiatric symptoms;
- Inflammatory processes in the brain and its membranes - meningitis, ventriculitis, encephalitis of meningococcal and pneumococcal etiology, especially in children - against the background of inflammation and the formation of adhesions in the interthecal space, the circulation of cerebrospinal fluid is disrupted, foci of gliosis appear in the brain substance as a result of alterative changes in encephalitis;
- Specific infections and invasions - tuberculosis or syphilitic brain damage, cryptococcosis, cysticercosis, preon infections, etc.
- Poliomyelitis, typhus, herpetic lesions of the central nervous system;
- Involvement of the brain in systemic connective tissue diseases - rheumatic chorea with the formation of peculiar granulomas, for example;
- Neoplasms of the brain and membranes, causing compression, atrophy, necrosis, hemorrhages in the nervous tissue with subsequent gliosis;
- Traumatic injuries - brain contusion of all degrees, open craniocerebral injuries, gunshot wounds, etc.;
- Severe intoxication - alcoholic encephalopathy, lead, mercury poisoning, etc.
- Pathological course of pregnancy, the influence of adverse factors and maternal diseases on the growing fetus, taking certain medications during pregnancy.
In addition to the above, severe cerebral atherosclerosis can also cause organic damage to the central nervous system if characteristic atrophic and scarring changes in the brain occur in combination with dementia, but such severe processes as multiple sclerosis and amyotrophic lateral sclerosis are not included in the group of organic changes. For these diseases, unlike organic damage, there are sections in ICD-10.
In the perinatal period, four main groups of organic brain lesions are identified:
- Traumatic injury;
- Hypoxic;
- Dysmetabolic and toxic;
- Infectious (usually viruses).
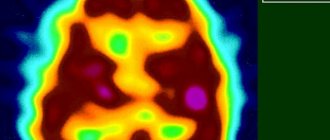
brain hypoxia (intrauterine or during childbirth) is the main reason for diagnosis in newborns
Such common diseases as osteochondrosis with damage to the spinal cord roots, compression of peripheral nerves and other disorders of the peripheral nervous system cannot in any way contribute to organic damage to the brain.
Classification of CNS lesions
Perinatal damage to the central nervous system is divided into several types:
- Hypoxic-ischemic . Characterized by internal or postnatal lesions of the brain. Appears as a result of chronic asphyxia. Simply put, the main cause of such damage is oxygen deficiency in the fetal body (hypoxia).
- Traumatic . This is a type of injury that occurs to a newborn during childbirth.
- Hypoxic-traumatic . This is a combination of oxygen deficiency with injury to the spinal cord and cervical spine.
- Hypoxic-hemorrhagic . Such damage is characterized by trauma during childbirth, accompanied by a failure of blood circulation in the brain with subsequent hemorrhages.
Symptoms depending on severity
In children, residual organic damage is difficult to see with the naked eye, but an experienced neurologist, already at the first examination of the baby, will be able to determine the external signs of the disease.
Often this is an involuntary trembling of the chin and arms, a restless state of the baby, a syndrome of tone disorders (lack of tension in the skeletal muscles).
And, if the damage is severe, it can manifest itself as neurological symptoms:
- paralysis of any limb;
- disturbance of eye movements;
- reflex failures;
- loss of vision.
In some cases, symptoms can only be noticed after undergoing certain diagnostic procedures. This feature is called the silent course of the disease.
General symptoms of residual organic damage to the central nervous system:
- unreasonable fatigue;
- irritability;
- aggression;
- mental instability;
- changeable mood;
- decreased intellectual abilities;
- constant mental anxiety;
- inhibition of actions;
- pronounced absent-mindedness.
In addition, the patient is characterized by symptoms of mental infantilism, brain dysfunction and personality disorders. As the disease progresses, the set of symptoms can be replenished with new pathologies, which, if left untreated, can lead to disability and, in the worst case, death.
Features of the course of pathology in childhood
The development of children with organic brain damage has some features and differs from that of their peers. Specialists and parents of children almost always face difficulties in education and training, since some functions may correspond to the age period or even be ahead of it, while others are seriously lagging behind. In this regard, the child’s behavior may not seem entirely correct - he does not obey, gives the impression of being ill-mannered and uncontrollable, gets tired quickly, may be too stubborn, inattentive, irritable, etc.
Timely diagnosis of organic brain damage makes it possible to work with such children purposefully, providing not only psychological and pedagogical support, but also medicinal support. If there is no diagnosis as such, then the psychologist’s task is to exclude organic pathology as the cause of behavioral characteristics or learning difficulties.
Children with organic brain damage have so-called damaged mental development, which includes relatively mild changes and disorders of moderate severity (minimal brain dysfunction, disorder of interhemispheric interactions), as well as conditions that indicate severe brain pathology - epilepsy, progressive disorder of the central nervous system with deep disorders of psycho-speech and motor development.
Minimal brain dysfunction is a mild degree of brain dysfunction, when learning abilities are reduced and there are some behavioral abnormalities. The prerequisites for the formation of this pathology in children are:
- Impact of harmful factors on a pregnant woman (gestosis, infections, intoxication, ethanol, medications, etc.);
- Birth injuries;
- Diseases, especially infectious ones, in the first 3 years of a baby’s life.
The listed factors can cause focal changes in the cortex and subcortex, which are characterized by an extreme variety of symptoms and are determined by the localization of the lesion. The most characteristic signs of minimal brain dysfunction are motor disorders:
- Awkward or excessive movements;
- Teak;
- Motor hyperactivity or severe slowness;
- Grimaces;
- Uncontrollable behavior.
These symptoms gradually decrease as the child grows, and with the right approach to educational activities and therapy in a teenager, they can be completely unnoticeable, unless they are discovered during an examination by a neurophysiologist or an EEG analysis.
In the case of unfavorable circumstances, such as injuries, operations, diseases of internal organs, infections, overwork, an unfavorable psychological climate in the family, the signs of brain damage deepen, and then minimal changes will turn into psychopathy, neuroses, convulsive syndrome, severe speech impairment, autism.
Due to the risk of worsening brain dysfunction with even mild organic damage, it is important for specialists to promptly identify children with disabilities and refer them for observation and treatment by a neurologist, for consultation with a psychologist, speech therapist, or defectologist.
Other manifestations of organic brain damage such as minimal dysfunction and cerebrasthenia are detected through a standard psychiatric examination. Patients have:
- Rapid mental fatigue and exhaustion;
- Reduced attention;
- Difficulty remembering;
- Uneven development of mental abilities when performing special tests (indicates against mental retardation);
- Emotional instability;
- Sensitivity to the assessment of a testing teacher or doctor.
Some patients with minimal impairments have age-appropriate development of personal qualities, while intellectual capabilities, memory, and learning are somewhat delayed. Such children worry about their inadequacy, are prone to stuttering, phobias, sleep disorders, tics, suffer from low self-esteem and are very responsive to the attitude and evaluation of people significant to them.
If the development of the volitional sphere and emotions is disrupted, then over time a psychopathic-like disorder may form, which will manifest itself in excessive excitability, emotional lability, touchiness, and irascibility. Patients with psychopathic-like syndromes are prone to such behavioral disorders as vagrancy, aggression, excessive sexual desire and attempts to realize it. Criticism of oneself and actions is reduced, self-esteem is inadequate.
The difference between a psychopathic-like syndrome and typical psychopathy is mental disorder and uneven underdevelopment of intelligence. Through research, it is possible to determine the exact location of the site of organic brain damage, which is especially important after injuries to the skull and central nervous system.
Interhemispheric dysfunction is a disorder in the development of one of the hemispheres of the brain or the interaction between the hemispheres. A patient with predominant activity of the right hemisphere may be left-handed with an unusual perception of the environment, figurative and symbolic thinking, while logical constructs, abstractions, and precise data are not easily perceived. In the first grades, difficulties appear with mathematics, lexical and grammatical analysis of sentences.
“Right-hemisphere” children have normal memory, attention, they are efficient, they remember visual images well in all details, they think as if in pictures, but the construction of logic and the search for patterns suffer greatly. The use of visual images and associations can significantly facilitate the learning process, therefore in elementary school it is important for the teacher not to concentrate on the standard program, but to make maximum use of visual aids, draw and encourage independent drawing of diagrams, tables, etc.
“Left-hemisphere” children, on the contrary, do poorly on tasks that involve the use of visual analysis. They have correct speech, read and write well, have logic, but may suffer from underdevelopment in the emotionally sensitive area.
Severe forms of organic brain damage are accompanied by profound disorders of speech, writing, and reading, which interfere with learning at school. It is important to teach such patients to recognize the emotions of others and express their own, and analyze the actions of others. Music, drawing, and special training have a beneficial effect on the development of the psyche. In adolescence, difficulties may arise when communication with peers gives way to the computer or spending time at home.
Necessary set of measures
It is no secret that diseases of this degree of danger are difficult to cure using single methods. And even more so, to eliminate residual organic damage to the central nervous system, it is even more necessary to prescribe complex treatment. Even with a combination of several therapy methods, the recovery process will take quite a long time.
To select the correct complex, you must strictly consult your doctor. Typically, the prescribed therapy includes the following set of measures.
Treatment with various medications:
- sedatives;
- psychotropic drugs;
- nootropics;
- antipsychotics;
- vitamins and minerals to improve brain function.
External correction (treatment with external stimulation):
- massage;
- treatment with special loads (kinesitherapy);
- physiotherapy (laser therapy, myostimulation, electrophoresis, etc.);
- reflexology and acupuncture.
Neurocorrection methods
Neurocorrection is a psychological technique that is used to restore impaired and lost functions of the brain.
If there are speech defects or neuropsychic disorders, specialists involve a psychologist or speech therapist in treatment. And in case of manifestation of dementia, it is recommended to seek help from teachers of educational institutions.
In addition, the patient is registered with a neurologist. He must undergo regular examination by the doctor who is treating him. The doctor may prescribe new medications and other therapeutic measures as the need arises. Depending on the severity of the disease, the patient may require constant monitoring by family and friends.
We emphasize that treatment of residual organic damage to the central nervous system during the period of acute manifestation is carried out only in a hospital setting, and only under the supervision of a qualified specialist.
Remember! Timely treatment of organic damage to the central nervous system can stop the development of complications, reduce the consequences of the disease, eliminate symptoms and completely rehabilitate the human nervous system.
Classification of perinatal lesions of the nervous system in newborns
Guidelines
Moscow, 1999
The classification project was discussed at the II Congress of the Russian Association of Perinatal Medicine Specialists. Moscow 1997
The methodological recommendations present fundamental approaches to the diagnosis of perinatal lesions of the nervous system, based on modern scientific advances and terminology used in the International Classification of Diseases and Related Health Problems, 10th revision (ICD 10).
The methodological recommendations are intended for pediatricians, neonatologists and neurologists of maternity hospitals, specialized hospitals for newborns and clinics.
The main developer is the Russian Association of Perinatal Medicine Specialists.
Leading experts took part in the preparation of the classification project
- Russian State Medical University
- Scientific Center for Obstetrics, Gynecology and Perinatology, Russian Academy of Medical Sciences
- Russian Medical Academy of Postgraduate Education
- Moscow Research Institute of Pediatrics and Pediatric Surgery
- Moscow Regional Research Institute of Obstetrics and Gynecology
- St. Petersburg State Pediatric Medical Academy
Core development team:
Ph.D. A.S. Burkova, Doctor of Medical Sciences N.N. Volodin, Ph.D. L.T. Zhurba, Doctor of Medical Sciences M.I. Medvedev, Ph.D. S.O. Rogatkin, Ph.D. O.V. Timonina.
The following people took part in the preparation of the classification project:
Doctor of Medical Sciences A.G. Antonov, Ph.D. E.N. Baibarina, Doctor of Medical Sciences Yu.I. Barashnev, Ph.D. A.M. Bolshakova, Ph.D. K.V. Vatolin, Ph.D. V.P. Geraskina, Ph.D. A.V. Gorbunov, Doctor of Medical Sciences G.M. Dementieva, Doctor of Medical Sciences M.S. Efimov, Doctor of Medical Sciences A.S. Petrukhin, Doctor of Medical Sciences G.M. Savelyeva, Doctor of Medical Sciences L.G. Sichinava, Academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences V.A. Tabolin, Doctor of Medical Sciences M.V. Fedorova, Doctor of Medical Sciences N.P. Shabalov.
Introduction
Deviations in the development of neuropsychic functions in young children in most cases have their roots in the perinatal period and are currently attracting increasing attention from researchers.
New opportunities have emerged in studying the origins of many diseases, pathological conditions and preventing irreversible consequences, often leading to severe childhood neurological disability.
In this regard, in the world literature of the last decade, “perinatal neurology” has emerged as an independent field of medicine, which reflects the achievements of specialists in various fields - obstetricians, neonatologists, pediatricians, neuropathologists, neurophysiologists, etc.
Modern methods for diagnosing the state of the nervous system of the fetus and newborn have been widely introduced into the clinical practice of obstetrics and neonatology: (neurosonography NSG, Doppler encephalography DEG, computed tomography CT, magnetic resonance imaging MRI, positron emission tomography PET, cerebral scintigraphy CSG, electroencephalography EEG, neuro-immunochemical identification of cerebral proteins, etc.).
The use of these advanced technologies in perinatal practice has made it possible to clarify the etiology, pathogenetic mechanisms, clinical and morphological structure, as well as the localization of cerebral disorders typical for different gestational ages, to develop unified approaches to terminology and to develop a new classification of perinatal damage to the nervous system of newborns.
This classification, in contrast to the previously used term “perinatal encephalopathy”, which reflects only the period of exposure to pathological factors and the general concept of brain dysfunction, provides for the division of neurological disorders of the neonatal period into 4 main groups depending on the leading mechanism of damage: I hypoxic, II traumatic , III toxic-metabolic and IV infectious.
In addition to the leading damaging factor, each of these groups distinguishes: nosological form, severity of damage and main neurological symptoms and syndromes.
Fundamentally new in the classification is the division of hypoxic brain damage into cerebral ischemia and intracranial hemorrhage.
In the heading “Intracranial birth injury”, in comparison with the previous classification, the number of nosological forms has been expanded: this block now includes subarachnoid and intraventricular hemorrhages.
The draft of this classification was compiled taking into account the terminological approaches used in ICD 10, which will make it possible to obtain the most reliable statistical data comparable to international standards, analyze the objective causes of morbidity and mortality, and develop effective methods for the treatment and prevention of early neurological disorders in children.
CLASSIFICATION OF PERINATAL NERVOUS SYSTEM LESIONS IN NEWBORNS
I. Hypoxic lesions of the central nervous system
| Pathogenetic characteristics | Nosological form | Main clinical symptoms and syndromes |
| I. A) P 91.0 Cerebral ischemia |
|
|
|
| |
|
| |
| I. B) P 52 Intracranial hemorrhages of hypoxic origin |
| No specific neurological symptoms |
|
| |
|
| |
|
| |
| The clinical picture depends on the location and volume of hemorrhage
| |
| I. B) Combined ischemic and hemorrhagic lesions of the central nervous system (non-traumatic) | The clinical picture and severity of the condition are determined by the leading type of lesion and localization |
II. Traumatic damage to the nervous system
| Pathogenetic characteristics | Nosological form | Main clinical symptoms and syndromes |
| II. A) P 10 Intracranial birth injury |
|
|
|
| |
|
| |
|
| |
|
| |
|
| |
| II. B) R 11.5 Birth injury of the spinal cord |
|
|
| II. B) R 14 Birth trauma of the peripheral nervous system |
Proximal Erb-Duchenne type (C 5-C 6) | Flaccid paresis of the proximal arm(s) |
| Flaccid paresis of the distal arm(s) Claude Bernard-Horner syndrome | |
| Flaccid total paresis of the arm(s) Claude Bernard-Horner syndrome Respiratory disorders rare | |
| Respiratory disorders (“paradoxical” breathing, tachypnea) Possibly asymptomatic | |
| On the losing side:
| |
|
III. Dysmetabolic and toxic-metabolic disorders of the central nervous system
| Pathogenetic characteristics | Nosological form | Main clinical symptoms and syndromes |
| III. A) P 70-P 71 Transient metabolic disorders |
|
|
|
| |
|
| |
|
| |
|
| |
|
| |
|
| |
| III. B) P 04 Toxic-metabolic disorders of the central nervous system |
|
|
IV. Damage to the central nervous system in infectious diseases of the perinatal period
| Pathogenetic characteristics | Nosological form | Main clinical symptoms and syndromes |
| IV. A) R 35 - R 37 Damage to the central nervous system due to intrauterine infections (TORCH syndrome) Encephalitis Meningitis Meningoencephalitis |
| |
| IV. B) CNS damage in neonatal sepsis Meningitis Meningoencephalitis Ventriculitis Encephalitis |
|
|
Comments
to the project “Classification of perinatal lesions of the nervous system in newborns”
In the first days of a child’s life, nosological diagnosis of lesions of the nervous system is often difficult due to the similarity of clinical neurological manifestations in various pathological conditions. Therefore, the classification shows the most common clinical symptom complexes characteristic of certain nosological forms.
In the first days of life, a syndromological diagnosis is allowed, but in the future it must be clarified. Obviously, the accuracy of the diagnosis increases as the newborn goes through various stages of nursing and depends on obtaining additional anamnestic data, clinical and laboratory tests.
The determining condition for accurate diagnosis is the accumulation, preservation and open exchange of standardized information received at various stages of medical care for newborn children.
The use of a syndromic approach when making a primary diagnosis allows neonatologists to more fully reflect the dynamics of the clinical picture in the absence of additional information and is justified in the conditions of obstetric institutions.
Examples of syndromic diagnosis: P 90 - newborn seizures (convulsive syndrome); P 91.3 - cerebral excitability of the newborn (hyperexcitability syndrome); P 91.4 - cerebral depression of the newborn (depression syndrome); P 91.5 - neonatal coma; P 91.8 - other specified disorders of the brain in a newborn (acquired hydrocephalus, intracranial hypertension, autonomic-visceral disorders); P 28.4 Other types of apnea in the newborn, etc.
The draft of this classification presents for the first time the differences in clinical neurological symptoms and syndromes, as well as the most typical types of cerebral damage in prematurely born and full-term children, which is due to the peculiarities of the blood supply to the brain in newborns of different gestational ages. The comments provide the most common clinical symptoms and syndromes depending on the degree of maturity.
The proposed classification contains ICD-10 indices corresponding to certain syndromes and nosological forms.
The basic principles for constructing a diagnosis of perinatal lesions of the nervous system in newborns should be based on a thorough analysis
- anamnestic information;
- clinical symptoms and syndromes;
- results of additional examinations
The logic of constructing a diagnosis for individual nosological forms is presented below.
Continued >>
Rehabilitation is all in the hands of the mother and doctors
Rehabilitation measures for this disease, as well as for its treatment, should be prescribed by the attending physician. They are aimed at eliminating existing complications in accordance with the patient’s age.
For remaining movement disorders, physical methods are usually prescribed. First of all, it is recommended to do therapeutic exercises, the main idea of which will be aimed at “revitalizing” the affected areas. Additionally, physical therapy relieves swelling of nerve tissue and restores muscle tone.
Mental development delays are eliminated with the help of special drugs that have a nootropic effect. In addition to the pills, they also conduct classes with a speech therapist.
Anticonvulsants are used to reduce the activity of epilepsy. The dosage and the drug itself must be prescribed by the attending physician.
Increased intracranial pressure should be eliminated by constant monitoring of cerebrospinal fluid. Pharmaceutical drugs are prescribed that increase and accelerate its outflow.
It is very important to eradicate the disease at the first alarm bells. This will enable the person to lead a normal life in the future.
Complications, consequences and prognosis
According to the experience of doctors, organic damage to the central nervous system in children can cause the following consequences:
- mental development disorders;
- speech defects;
- delayed speech development;
- lack of self-control;
- hysterical attacks;
- disruption of the normal development of the brain;
- post-traumatic stress disorder;
- epilepsy attacks;
- vegetative-visceral syndrome;
- neurotic disorders;
- neurasthenia.
In children, quite often such disorders affect adaptation to environmental conditions, manifestations of hyperactivity or, on the contrary, chronic fatigue syndrome.
Today, the diagnosis of “residual organic damage to the central nervous system” is made quite often. For this reason, doctors are trying to improve their diagnostic and treatment abilities.
The exact characteristics and features of a certain type of lesion make it possible to calculate the further development of the disease and prevent it. In the best case, suspicion of the disease can be completely removed.
Residual-organic borderline neuropsychiatric disorders
7. Residual organic borderline neuropsychiatric disorders _ _
Residual-organic disorders are considered to be a variety of neuropsychic disorders in children and adolescents caused by relatively persistent consequences of previously suffered organic brain damage (Kovalev V.V., 1979).
The main place among residual organic neuropsychic disorders is occupied by the consequences of early organic brain damage that occurred in the prenatal period, childbirth and in the first 3 years of life (hypoxia, ischemia, hemorrhage, intoxication, neuroinfection, hemolytic disease of the newborn). There are different opinions regarding which period of postnatal development should be considered early. Some researchers believe that this period is up to 1 year of age (Lempp R., 1974). If we accept that the differentiation of the layers of the cerebral cortex is completed by the age of 7 (Filimonov N.N., 1922), then the earliest should probably be considered the age before 7 years.
This is not a scholastic, but a specific and very complex problem. It comes down mainly to the technology for determining the proportion of dysontogenetic and organic deficiency disorders that arose in a child after the end of the organic process. Obviously, the earlier it arose, the more significant the proportion of manifestations of mental dysontogenesis will be. In addition, its manifestations will most likely be varied. For example, young children may have the following options: mental retardation, infantilism, transient or persistent mental retardation, delayed development of certain psychological functions, organic autism.
In older children, the number of variants and severity of manifestations of dysontogenesis itself, theoretically, gradually decreases as they grow older, and the residual symptoms themselves are limited mainly to dementia, psychoorganic and cerebrasthenic syndromes. It is considered established that residual organic failure of the central nervous system shows a dependence on the age at which the organic disease occurred: the earlier it occurred, the more severe, other things being equal, the residual symptoms.
In general, the number of combinations of manifestations of dysontogenesis, on the one hand, and symptoms of organic mental deficiency, on the other, cannot be accurately determined, especially since other factors also take part in symptom formation, such as heredity, hereditary and constitutional predisposition to the development of pathology, external mechanical, physical, chemical and psychotraumatic factors, upbringing, training, etc.
The term “residual” does not mean that residual phenomena are purely static. They can undergo certain dynamics - this is primarily regredient dynamics, in which the processes of reparation and progressive development predominate. Thus, according to a follow-up study (Aksentyev S.B., Barabash M.N. et al., 1965), 39.4% of patients with a previously established diagnosis of “residual organic failure of the central nervous system” turned out to be practically healthy after several years. The condition can be relatively stationary and, to one degree or another, compensated. The more fragile the compensation, the more easily decompensation states with different clinical pictures arise. The dynamics can be negative if the patient is often or constantly exposed to other unfavorable circumstances. Finally, with the participation of residual cerebral insufficiency and additional influences at a given age, a hereditary, constitutional and/or acquired predisposition to the development of a certain mental, neurological or somatic disease may appear. It is also important to take into account that, superimposed on the residual background, repeated organic damage can lead to more serious consequences.
The prevalence of residual central nervous system failure in children and adolescents is presented differently, depending on differences in approaches to their recognition. Thus, in the book “Morbidity of the Urban Population and Standards for Treatment and Preventive Care” (1967) the following information is provided (per 1000 children and adolescents). For boys: at the age of 1–2 years – 3.2; from 3 to 6 years – 2.9; from 7 to 12 years – 7.2; from 13 to 15 years – 7.6; from 16 to 19 years old – 4.9. For girls: aged 3 to 6 years – 1.4; from 7 to 12 years – 3.6; from 13 to 15 years – 8.1; from 16 to 19 years old – 4.9. These data indicate insufficient detection of this pathology in young children and its predominance in boys.
Foreign researchers give higher figures. According to F. Enke (1955), the prevalence of this pathology in the general population is 6.5%, according to R. Lempp (1974) – 17.9% (in school-age children). In children with difficulties in school adaptation and neurotic reactions, residual pathology is detected more often - from 32 to 93%. V.V. Kovalev points out that such indicators are the result of overdiagnosis, which occurs due to an overestimation of the diagnostic value of individual indicators (neurological microsymptoms, EEG data, manifestations of insufficiency of general or speech motor skills, anamnesis data), which are found with almost the same frequency in control studies of healthy children.
There are different taxonomies of residual organic neuropsychiatric disorders in children and adolescents. The following briefly presents the clinical variants of such disorders according to the pathogenetic taxonomy of V.V. Kovaleva (1979):
- predominantly dysontogenetic forms;
- predominantly encephalopathic forms;
- forms of mixed pathogenesis (encephalopathic-dysontogenetic).
Detailed descriptions of a number of disorders mentioned below are given in parts 2 and 3 of this book (see table of contents). Some disorders are presented in this section following the taxonomy of residual organic failure of the central nervous system.
Return to Contents