The external, otherwise called lateral, cutaneous nerve of the thigh is formed by nerve fibers emerging from the second and third lumbar spinal roots (LII-LIII, L2-L3). Rushing along the iliacus muscle, it passes under the inguinal (pupart) ligament and extends to the anterior outer femoral surface. In this area, closer to the pelvis, the nerve branches.
The lateral cutaneous nerve of the thigh consists only of sensory fibers, so when it is damaged, muscle function is not impaired.
Neuritis of the lateral cutaneous nerve of the thigh is its inflammatory lesion, the main symptom of which is pain - neuralgia.
general description
Damage (neuropathy) of the femoral nerve (G57.2) is damage to the femoral nerve in the area where it exits the retroperitoneum onto the thigh behind the inguinal ligament, manifested by weakness of the anterior thigh muscles, numbness or pain along the anterior inner surface of the thigh.
The syndrome is more common in women (65%), the peak incidence is observed at the age of 40–60 years.
Causes: isolated trauma or nerve damage during surgical interventions (surgeries in the pelvic organs, on the hip), compression by retroperitoneal hematoma, tumor, abscess. Toxic effects and metabolic changes in diabetes mellitus are also possible.
Treatment
At the First Medical Clinic, an integrated approach is used to treat neuritis (neuralgia) of the lateral cutaneous nerve of the thigh.
First of all, efforts are aimed at eliminating pain. Therapeutic blockades have proven especially effective in this regard - the introduction of local anesthetics or their mixture with anti-inflammatory drugs at the point of maximum sensation. The delivery of drugs directly to the affected area interrupts the transmission of nerve impulses and blocks the attack of pain.
To suppress inflammatory processes, relieve muscle spasms, eliminate or correct causative factors, local injection therapy - anti-inflammatory, muscle relaxant, antibacterial, painkillers, vitamins and other drugs are injected into the area of disorders.
The course of treatment for neuritis (neuralgia) of the lateral cutaneous nerve of the thigh may also include methods such as:
- transcutaneous electromyoneurostimulation - exposure to weak pulses of electric current to restore muscle activity, improve blood circulation and tissue nutrition;
- shock wave therapy;
- manual therapy and osteopathy;
- laser therapy;
- massotherapy;
- reflexology;
- ozone therapy;
- hirudotherapy;
- physical therapy, etc.
The required amount of therapeutic assistance can only be determined by a specialist after diagnostic procedures. If symptoms of neuritis (neuralgia) of the lateral cutaneous nerve of the thigh appear, we recommend that you contact the First Medical Clinic in a timely manner.
You can make an appointment for a consultation and appointment by phone
Clinical picture
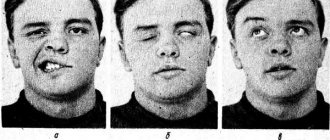
The disease develops gradually. The first complaint of patients is weakness in the leg (“doesn’t obey, as if it’s giving way”) (100%), difficulty walking (60%). Also concerning is pain in the leg, which increases with extension (90%). Less commonly noted is a decrease in sensitivity along the anterior inner surface of the thigh (40%).
An objective examination of the patient reveals pain below the inguinal fold, along the anterior inner surface of the thigh (70–90%), hypalgesia in the area of innervation of the femoral nerve; decreased knee reflex, weakness of the anterior thigh muscles, muscle atrophy.
Neuropathy of the external cutaneous nerve of the thigh
Neuropathy of the external cutaneous nerve of the thigh: this disease is expressed by damage to the lateral cutaneous nerve of the thigh in the groin area. The most common cause is age-related changes in the body. Neuropathy of the external cutaneous nerve of the thigh expresses itself as a disorder of the sensitivity of the skin, pain and numbness, and walking impairment may occur. The doctor makes a diagnosis after a full examination, and therapy is carried out using medications and physiotherapeutic methods.
Treatment of femoral nerve damage
- Symptomatic therapy (decongestants, analgesics).
- Exercise therapy, novocaine and hydrocortisone blockades.
- Surgical intervention in the inguinal ligament area.
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist.
Essential drugs
There are contraindications. Specialist consultation is required.
- Voltaren (non-steroidal anti-inflammatory drug). Dosage regimen: IM at a dose of 75 mg (contents of 1 ampoule) 1 time/day.
- Ketoprofen (non-steroidal anti-inflammatory drug). Dosage regimen: IM - 100 mg 1-2 times a day; after pain relief, it is prescribed orally in a daily dose of 300 mg in 2-3 doses, a maintenance dose of 150-200 mg/day.
- Fluoxetine (antidepressant). Dosage regimen: the initial recommended oral dose is 20 mg/day. Recommended doses can be increased or decreased until a therapeutic effect is achieved. The drug can be taken regardless of meals.
- Diacarb (a diuretic from the group of carbonic anhydrase inhibitors). Dosage regimen: adults are prescribed 250-500 mg once in the morning for 3 days, on the 4th day - a break.
- Milgamma (B complex of vitamins). Dosage regimen: therapy begins with 2 ml intramuscularly 1 time per day for 5-10 days. Maintenance therapy - 2 ml IM two or three times a week.
Symptoms of the disease
In most cases, changes in the body manifest themselves gradually. Initially, numbness may occur in areas of the skin on the side of the thigh, then spread to the front. A sensitivity disorder occurs - sensations of burning, coolness, tingling, etc. occur. At the initial stage of the disease, these manifestations are temporary, but with the development of pathology they become permanent. There is pain and difficulty walking. In certain cases, hair loss and thinning of the skin may occur.
Recommendations
Consultation with a neurosurgeon and magnetic resonance imaging of the retroperitoneum are recommended.
| • | Leading specialists and institutions for the treatment of this disease in Russia: |
| Doctor of Medical Sciences, Head of the Department of Russian State Medical University, Professor, Academician of the Russian Academy of Medical Sciences Gusev E.I. | |
| • | Leading specialists and institutions for the treatment of this disease in the world: |
| G. AVANZINI, Italy. |
Diagnosis and treatment of the disease
The diagnosis is made after all studies and collection of anamnesis of the disease. Consultation with additional specialists such as an orthopedist may be required. X-rays of the spine, ultrasound, CT, electromyography, and electroneurography are performed.
Treatment of neuropathy of the external cutaneous nerve of the thigh is carried out only in a combination of medication and physiotherapeutic, as well as reflexology methods. It is very important to eliminate the root cause of the disease.
Drugs are prescribed to reduce pain, anti-inflammatory drugs, analgesics, and sometimes it is necessary to resort to the administration of anesthetics. Vasoactive agents and metabolic pharmaceuticals are used. Physiotherapy and reflexology are provided. Sometimes it is necessary to resort to surgery, which involves decompressing the nerve.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 0.1 | 10 | 10 | 15 | 15 | 0 | 0 | 0.1 | 10 | 10 | 15 | 15 |
Lumbar plexus block (anterior approach)
Carlos A. Bollini, Carlos Sforsini, Luis Vascello
Femoral nerve blocks alone, or in combination with other nerve blocks, are the most commonly used regional block techniques in lower extremity surgery. If it is necessary to block all branches of the lumbar plexus, then the lateral cutaneous and obturator nerves should be blocked. Blocking the three lumbar plexus nerves that go to the lower extremity with a single injection is known as a 3-in-1 block and is discussed in this review. If a complete and unilateral block of sensation in the leg is necessary, then a combined block of the femoral, lateral cutaneous, obturator and sciatic nerves should be performed. We prefer the injection site located directly on the inguinal fold. This method is easy to implement. The method causes minor discomfort in patients; Most patients, especially younger patients, report a “feeling of tightness” associated with the insertion area—its proximity to the genitals. Our preferred method is peripheral nerve stimulation (PNS). The search for a motor response begins at intensity = 1 mA, with a duration of 0.1 ms and a frequency of 2 Hz. The needle is advanced until the appropriate muscle response occurs: up and down movement of the kneecap (“kneecap dance”) and/or twitching of the quadriceps muscle, level II: with < 0.5 mA, pulse width = 0.1 ms and frequency = 2 Hz Infusions are often given through a long-term femoral catheter. With a good knowledge of anatomy and mastery of the SPN method, nerve blockade of the lumbar plexus (anterior approach) or an isolated nerve is safe, effective and well tolerated by patients.
This blockade was first described by Labat in 1912 [1]. The femoral nerve can be blocked alone or together with other nerves. If it is necessary to obtain a block of all branches of the lumbar plexus [2], which go along one side to the lower limb, then the lateral cutaneous nerve of the thigh and the obturator nerve should be blocked. Blocking the lumbar plexus nerves that go to the lower extremity with a single injection is known as a 3-in-1 block [3], a method that will be discussed below. If a complete and unilateral block of sensation in the leg is necessary, then a combined block of the femoral, lateral cutaneous, obturator and sciatic nerves should be performed. The high success rate of video-assisted surgical techniques has already led to an increase in the rate of knee surgery, as well as an increase in the rate of reconstructive surgery on the joint.
Femoral nerve blocks alone, or in combination with other nerve blocks, are the most commonly used regional block techniques in lower extremity surgery.
Anatomical overview
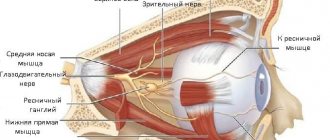
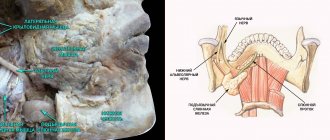
The femoral nerve is one of the terminal branches of the lumbar plexus. It starts from the dorsal roots L2-L3-L4. The nerve passes obliquely through the pelvis through the fibers of the psoas muscle, exits the psoas muscle at the inferior border, and then courses downward in the space between the psoas and iliacus muscles (Figure 1).
| Figure 1. The femoral nerve passes obliquely through the pelvis through the fibers of the psoas muscle, emerging from the psoas muscle at the lower border. |
The nerve exits the pelvis onto the thigh under the inguinal ligament posterior and lateral to the femoral vessels, separated from them by the fascia iliaca.
At or above the level of the inguinal ligament, the nerve divides into anterior branches: lateral and medial, and posterior branches or the quadriceps nerve (Figure 2).
| Figure 2. Preparation at the level of the inguinal ligament. Femoral nerve: 1 - deep branch; 2 – medial branch; 3 – lateral branch. A – inguinal ligament. B - femoral artery. C - femoral vein. |
The anterior lateral cutaneous nerve of the thigh lies more superficially. It is motor for the sartorius and sensory for the skin of the anteromedial thigh and medial knee. At the same time, the anterior medial cutaneous nerve of the thigh is motor for the pectineus and adductor longus muscles, and sensory for the upper and medial surface of the thigh.
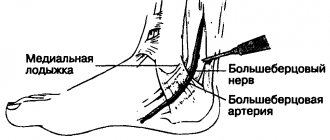
The posterior branch or quadriceps nerve is deeper. It divides into four motor branches for the four quadriceps muscles and also gives off sensory branches or the saphenous nerve, which supplies the anteromedial aspect of the knee and runs with the saphenous vein along the anteromedial aspect of the leg down to the medial malleolus.
It is important to emphasize that the femoral nerve is located in various aponeurotic spaces and deeper than the femoral vessels. The femoral artery and vein are located between the lata and fascia iliaca, while the nerve is located below the fascia iliaca [4].
The nerve passes lateral (outward) to the femoral artery and at a distance of 1 transverse finger from it (2 cm). Therefore, they are not part of the common neurovascular bundle, despite what occurs in the axillary fossa. This nerve is primarily motor (80%), and therefore localization is best accomplished with a peripheral nerve stimulator rather than with paresthesia techniques. You need to remember the “VAN” diagram (vein, artery, nerve).
Indications
- Postoperative pain relief for moderate to severe knee pathology.
- Patella fracture, quadriceps tendon rupture, knee arthroscopy. As a single method or in combination with other methods, for outpatient surgeries on the posterior cruciate ligament of the knee [5-9].
- Total knee replacement as a single method or in combination with sciatic nerve blockade, single and long-term administration [10-19].
- Preoperative analgesia in patients with a hip fracture to the medial third and/or transport from the ward to the operating room or to the x-ray room to move and position on the operating table, before performing an epidural or subarachnoid block in these patients [20, 21].
- Following quadriceps reconstruction, for the placement and removal of femoral plates and screws or total knee replacement (TKA) in patients requiring early postoperative mobilization.
- These techniques improve the assessment of acute knee injury during arthroscopy and other knee surgeries because blocking both nerves with a sufficient volume of local anesthetic blocks sensation in the entire lower extremity.
- For muscle biopsy in patients with malignant hyperthermia [22].
Equipment
- Marker
- Millimeter ruler
- 20 ml syringe
- 25-G needle
- Local anesthetic
- Peripheral nerve stimulator
- Skin electrode
- 22-G, 50mm insulated needle
- Catheter
Method
- The patient is in a supine position. The lower limb is positioned in slight adduction and external abduction of 10°-20° or in a “neutral position.” Light sedation.
- The operator is located on the opposite side.
- Anatomical landmarks are identified and marked with a marker: the inguinal ligament extends from the anterior superior iliac crest to the lateral edge of the pubic tubercle; pulsation of the femoral artery (Figure 3).
- For obese patients, an assistant should support the apron toward the head.
- The pulsation of the femoral artery is determined, the fingers of the hand are positioned, distributing pressure in such a way as to protect and close the artery below. The femoral artery is the most important landmark (Figure 4).
- Doppler ultrasound can be used to visualize the femoral artery.
| Figure 3. Anatomical landmarks: anterior superior iliac crest (ASIC), lateral border of the pubis, inguinal ligament, inguinal fold. |
| Figure 4. Pulsation of the femoral artery is detected and the fingers are positioned to distribute pressure to protect and close the artery below. The femoral artery is the most important landmark. |
Labat classic paresthesia method and procedure for catheter placement
- A “lemon peel” is made at a point located directly under the inguinal ligament closer to the lateral wall of the femoral artery pulsation. Since the finger feels the pulsation below the inguinal ligament, a “lemon peel” is placed on the finger below the line of the inguinal ligament (1-2 cm).
- A 22-G, 2-inch (5-cm) short-bevel needle is inserted perpendicular to the skin and then advanced slightly in the cephalic plane.
- Typically two “pops” are felt as the needle passes through the fascia lata and the fascia iliacus. A loss of resistance is felt as the needle passes through the fascia iliaca.
- The needle is advanced until these two “pops” are received or until a loss of resistance is felt. Paresthesia is not necessary with this method [24]. Patients may experience pain.
- If the paresthesia technique is used and paresthesia is not noted, the needle should be redirected laterally and/or medially. The nerve is located superficially approximately 2 to 3 cm from the surface of the skin.
Peripheral nerve stimulation method
The difference between this method and the classical method is based on the injection site. When performing this method, we prefer the injection site located directly on the femoral crease [23]. If this fold is not marked, patients are asked to flex the leg. If this is not possible, then the distal point is marked 5 cm from the inguinal ligament and lateral to the pulsation of the artery (Figure 5).
| Figure 5. Femoral crease and puncture site marked X. |
The search for a motor response begins at an intensity of 1 mA, with a duration of 0.1 ms and a frequency of 2 Hz. The needle is advanced perpendicular to the skin (Figure 6) or slightly cephalad until an appropriate muscle response is obtained: movement of the kneecap up and down (“kneecap dance”) and/or twitching of the entire quadriceps muscle, level II: ≤ 0.5 mA, with duration ripple 0.1 ms and frequency 2 Hz.
| Figure 6. The needle is advanced perpendicular to the skin or slightly cephalad until an appropriate muscle response is obtained: movement of the kneecap up and down (“kneecap dance”) and/or twitching of the entire quadriceps muscle, level II: ? 0.5 mA, with a ripple duration of 0.1 ms and a frequency of 2 Hz. |
The most common initial responses are isolated twitching of the sartorius muscle due to stimulation of the anterior lateral branch and twitching of the adductor muscle due to stimulation of the anterior medial branch. This may confuse the operator and be mistakenly interpreted as an appropriate response. If this occurs, the tip of the needle should be redirected laterally and advanced deeper, ignoring this twitching.
If the patient is in skeletal traction, the nerve will be deeper and, depending on the thickness of the thigh, the block will be more difficult to perform. If a neurolocalizer is to be used in these patients, we recommend starting with a low current < 1 mA, as the quadriceps twitch may occur abruptly when passing through the fascia iliaca and can be very painful.
In recent years, there has been some interest in the use of ultrasound to more accurately determine needle placement. Marhofer [25] showed that this method reduces development time and improves the quality of sensory blockade compared to the use of a neurolocalizer.
Local anesthetic
The choice of local anesthetic depends on the intended purpose. If the blockade is done for intra- and postoperative pain relief, then we use 0.25% or 0.5% bupivacaine in a volume of 10 - 15 ml with adrenaline 1:200,000 [4].
We only use 1.5% or 2% lidocaine or mepivacaine with epinephrine if we need rapid development of anesthesia, such as for muscle biopsies. Some authors refer to the addition of clonidine rather than epinephrine.
Comments
This method is easy to follow. The method causes minor discomfort in patients; Most patients, especially younger patients, report a “feeling of tightness” associated with the area of insertion—its proximity to the genitals.
- In most cases, mild sedation with 1 to 2 mg midazolam is sufficient.
- The development of the block takes from 20 to 30 minutes.
- In patients with pain in the early postoperative period, the blockade can be repeated.
We believe that the insertion site should be at the level of the femoral crease. Blocks closer to the inguinal ligament should only be performed in cases where insertion of a long-term infusion catheter is indicated [26].
Patients should be warned in advance that they should not walk or lean on the anesthetized leg while the blockade is in effect. Otherwise, they may fall.
Three-in-one blockade (3-in-1)
The purpose of this method, proposed by Winnie et al [3], is to block three nerves (femoral, lateral femoral cutaneous nerve and obturator nerve) with a single injection, since the femoral nerve is located in the space formed by the fascia iliaca. In this study, the author reported that three nerves were 98.6% blocked, but he was unable to determine how this could be determined.
Method
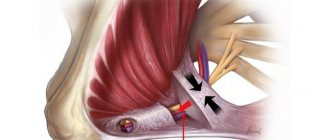
The needle is inserted at an identical point to the point described by Labat. It is located 1 - 2 cm lateral to the pulsation of the femoral artery and 1 cm distal to the inguinal ligament. But the needle is directed cephalically at an angle of 45° (Figure 7).
| Figure 7. Left: The needle is inserted 1-2 cm lateral to the femoral artery pulse and 1 cm distal to the inguinal ligament, the needle is directed cephalically at an angle of 40°. Right: The cannula is removed and the catheter is secured. |
- Once the femoral nerve has been identified by paresthesia or neural location, apply firm finger pressure distal to the insertion site and maintain pressure throughout the insertion.
- 30 ml of local anesthetic is injected. The catheter can be positioned 15 cm cephalad. In these cases, the catheter should be inserted as close as possible to the outer wall of the femoral artery.
There is a debate about whether three nerves are blocked or not. It was initially thought that a large volume of local anesthetic would rise through the fascia between the psoas and iliacus muscles, thereby blocking all three nerves. Clinically, the femoral and lateral femoral cutaneous nerves can be easily blocked. The local anesthetic rarely reaches the obturator nerve, thus 80% of the volume is wasted. This occurs due to the spread of local anesthetic below the fascia iliaca. Therefore, in reality, it is more of a “2-in-1 block” rather than a “3-in-1 block” [27-31].
In the few cases where the obturator nerve is blocked, it is definitely due to diffusion of the anesthetic to the subsarticular plexus, where the femoral and obturator nerves are located nearby.
When the 3-in-1 block is combined with a classic sciatic nerve block, a complete block of the lower extremity is achieved, eliminating adduction. Since the obturator nerve is not blocked, the patient will report knee pain. This suggests that articular branches from the posterior ramus of the obturator nerve may be lost with this combination of blocks. This is why, for postoperative analgesia or single leg surgery, it is better to combine a single femoral block with a parasacral sciatic nerve block [14] or an iliacus muscle block with a classic sciatic nerve block [32, 33].
Iliac - fascial blockade
Cadaveric dissection and clinical studies performed by Dalens et al [34] indicate that large volumes of local anesthetic injected under the ilioinguinal ligament and under the fascia iliaca can spread cephalad. The anesthetic solution first contacts the femoral nerve and the lateral femoral cutaneous nerve, and then can reach the femorogenital and obturator nerves.
Indications
Same as for 3-in-1 block, lumbar block and femoral block.
Equipment
- Marker
- "Children's" Touhy needle
- Catheter or single injection
- No nerve stimulator required
Method
The technique is identical for children and adults [34, 35].
- The patient is placed in a supine position with the limb locked in slight adduction, with an outward rotation of 10°.
- The anterior superior iliac crest and pubic tubercle are identified.
- Using a marker, the ilioinguinal ligament is marked on the skin, then it is divided into three equal parts. The needle insertion point is located 1 cm distal to the point where the lateral third of the ilioinguinal ligament joins the medial two thirds (Figure 8).
- After treating the skin with an antiseptic solution, a “baby” Touhy needle is inserted perpendicular to the skin with a cephalic inclination of 30°. First, the bevel is directed upward, and then it is rotated 180° towards the fascia. The needle is advanced cephalad. Both “pops” are determined, corresponding to the passage of the needle through two fascia (the first - when passing through the lata fascia, the second - through the iliac fascia).
- Under distal digital pressure, 30 ml of local anesthetic (for adults) is injected in parts.
- Based on: 0.7 ml/kg for patients weighing 20 kg or less, 5 ml for 20 - 30 kg, 20 ml for 30 - 40 kg, 25 ml for 40 - 50 kg and 30 ml for patients over 50 kg.
| Figure 8. Iliofascial block: The ilioinguinal ligament is marked with a marker on the skin and then divided into three equal parts. The needle insertion point is located 1 cm distal to the point where the lateral third of the ilioinguinal ligament joins the medial two thirds. |
Discussion
- The advantage is that no nerve stimulator is required.
- Easy execution.
- High incidence of femoral nerve and lateral femoral cutaneous nerve blocks; on the other hand, the frequency of obturator nerve blockade is extremely low (50-75%).
Lateral cutaneous nerve block of the thigh
This blockade was described in 1909 by Nystrom [36-38].
Anatomy
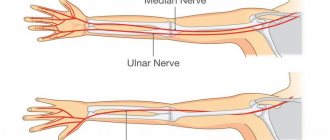
The lateral cutaneous nerve of the thigh is a small and purely sensory nerve. It innervates the anterolateral surface of the thigh to the knee. The corresponding area of innervation does not include the greater trochanter of the femur in the cephalic direction. It usually runs along the inner surface of the anterior superior iliac crest and crosses the fascia lata 3 to 4 cm below the inguinal ligament; however, it is a non-permanent nerve in its anatomical direction. After crossing the iliac arch, it divides into two branches. The nerve can be located either above or below the fascia iliaca (Figure 9).
| Figure 9. Anatomical variations in the course of the lateral femoral cutaneous nerve. |
Indications
- Narrow range of indications for performing an isolated block.
- For muscle biopsy in patients with suspected malignant hyperthermia.
- Anesthesia in combination with femoral and obturator blockades.
- Treatment of neuralgia of the lateral cutaneous nerve of the thigh.
- To obtain a skin implant.
- Preventing tourniquet pain along with other nerves.
- Postoperative pain during knee surgery, as a mono-method or in combination with other methods.
- Surgical treatment in the innervated area.
Method
- Classically, the patient is in the supine position.
- The anterior superior iliac spine is identified by palpation and marked.
- A “lemon peel” is made, located 2 cm caudally and 2 cm medially (Figure 10).
- The needle is inserted and directed cephalically until it encounters the bone of the anterior superior iliac spine along its inner surface.
- The needle is retracted posteriorly, a 1.5% lidocaine solution in a volume of 5-10 ml with adrenaline 1:200,000 is injected.
- At present, based on the results obtained by Shannon, the puncture should be performed only 1 cm caudal to and immediately inferior to the inguinal ligament. The introduction is the same as with the classical method.
- The insertion can also be carried out without directing the needle cephalically, by directly inserting the needle deep into the fascia lata. If the needle is blunt, a “pop” or loss of resistance will be felt as it passes through the fascia.
| Figure 10. The needle is inserted and directed cephalad to the bone of the anterior superior iliac crest on its inner surface. |
Due to significant anatomical variations in the course of the nerve, this latter option is considered a more rational method of administration, since it is a purely sensory nerve - using a nerve stimulator [39]. Shannon describes the patient reporting paresthesia along the lateral thigh. He uses 0.6 mA as the final value and injects 6 ml of 2% lidocaine with epinephrine, achieving 100% success versus 40% success with the classical method. The disadvantages of this method are that the participation of the patient is necessary.
Although the lateral area of analgesia is wide, it is not sufficient for proximal incisions in the greater trochanter of the femur.
Obturator nerve block
Anatomy
The obturator nerve is a mixed nerve formed by the union of the anterior branches of the L2, L3 and L4 roots. The connection occurs in the thickness of the psoas muscle. The nerve passes through the obturator foramen along with the obturator vessels. It is in close relationship with the inferolateral wall of the bladder, with the neck and prostate part of the male urethra. In urology, the nerve is often stimulated through the bladder wall, causing adduction of the leg. It divides into two branches: the anterior and posterior branches. The anterior branch innervates the hip joint and forms the subsarticular plexus, while the posterior branch innervates the adductor muscles, knee, and skin of the medial thigh. In 30% of cases there is an additional obturator nerve, which is formed from the branches of L3 and L4. This accessory nerve follows the same path as the obturator nerve, but it crosses the superior ramus of the pubis and gives branches to the hip joint and pectineus muscle [40].
Indications
- Necessary for diagnosis, prognosis and treatment in patients with adductor muscle spasm, multiple sclerosis, stroke complications, neuromuscular diseases and quadriplegia, i.e. in patients who cannot walk or wash themselves.
- Phenol poisoning or alcohol intoxication.
- Differential diagnosis of hip pain.
- In combination with femoral nerve and lateral femoral cutaneous nerve blocks (“3-in-1 block” and lumbar space block) for postoperative analgesia in knee surgery.
- Chronic hip pain due to osteoarthritis [41].
Classic method according to Labat [42, 43]
- In the supine position, the lower limb should be positioned with slight adduction.
- The symphysis of the pubic symphysis is palpated and the needle is inserted 1 - 2 cm lateral and 1 - 2 cm below the pubic tubercle. The femoral artery is located medial to the needle and halfway from the pulsation of the artery and the pubic tubercle (Figure 11).
- 22- G A 10 cm needle is inserted in a horizontal plane and advanced perpendicular to the skin below the adductor tendon to the lower edge of the superior ramus of the pubis. The depth at which the needle hits the bone should be noted.
- The needle is retracted and redirected laterally and slightly inferiorly, then advanced 1.5 to 2 cm beyond the previously noted depth (Figure 12), below the lower border of the bone edge of the ramus of the pubis until paresthesia appears. If paresthesia does not develop, then 10 - 15 ml of local anesthetic is infiltrated in a fan-shaped manner after careful aspiration.
- The same method is used with SPN starting at 2 mA or 0.1 ms. Twitching of the adductor muscles is observed at a current <0.5 mA, then 10 ml of local anesthetic is injected.
| Figure 11. Right leg: needle direction and puncture site. |
| Figure 12. The needle is retracted and redirected laterally and slightly inferiorly, and then advanced 1.5-2 cm above the previously noted depth. |
Access between adductor muscles [44]
- The patient is in the supine position with the leg adducted and externally rotated, the ankle of the blocked leg lies on the opposite leg (the “four” position).
- A skin mark is made 1-2 cm medial to the femoral artery just below the inguinal ligament.
- The adductor tendons are palpated.
- A 22-gauge 10 cm insulated needle is inserted just below the tendon approximately 2.5 to 3 cm from the pubic bone.
- The needle is directed to the mark made earlier 1 - 2 cm medial from the pulsation of the femoral artery, immediately below the inguinal ligament in the horizontal plane.
- The nerve runs at a depth of 3 - 6 cm.
- 10 ml of local anesthetic is injected after obtaining a twitch of the adductor muscles at a current of <0.5 mA.
- Be careful when inserting due to the proximity of the obturator vessels.
Discussion
In patients with an accessory obturator nerve and a good obturator block, there will eventually be spasm in the adductor muscles. An accessory obturator nerve block is performed by injecting a local anesthetic along the anterior edge of the superior ramus of the pubis, in the middle of the obturator foramen arch [45].
In patients who cannot assume the required position due to their spasticity, the branches of the obturator nerve are blocked separately. The anterior branch is blocked first using the adductor tendon as a guide.
The needle is inserted 2 cm below the cephalic tendon insertion. Above this tendon, the needle is directed 2 - 3 cm in the frontal plane and 10 ml of local anesthetic is injected in a fan-shaped manner.
After 20 minutes, hip adduction is achieved and the posterior edge of the adductor tendon is determined. The needle is inserted at an angle of two fingers from the pubic bone, then the needle is directed 3 - 4 cm laterally in the cephalic direction. 10 ml of local anesthetic is injected. Both nerves can be identified using SPN.
This method is contraindicated in patients with infections in the specified area.
Aspiration is always required before insertion as this is an area with a good blood supply.
Links
- Labat G. Regional Anesthesia: Its Technique and Clinical Applications. Philadelphia, PA, W. B. Saunders, 1923.
- Rouviere H., Delmas A. Anatomic Humana Tome, 3. Masson, 1996, p. 474.
- Winnie AP, Ramamurthy S., Durrani Z. The inguinal paravascular technique of lumbar plexus anesthesia: the “3-in-1 block”. Anesth Analg 1973, 52:989-996.
- Bridenbaugh PO The lower extremity: somatic blockade, in Cousins MJ, Bridenbaugh PO (eds): Neural Blockade in Clinical Anesthesia and Management of Pain (ed 2). Philadelphia, PA, JB Lippincott, 1988, pp 417-440.
- Mulroy MF, Larkin KL, Batra MS, et al. Femoral nerve block with 0.25% or 0.5% bupivacaine improves postoperative analgesia following outpatient arthroscopic anterior cruciate ligament repair. Reg Anesth Pain Med 2001, 26:24-29.
- Jankowski CJ, Horlocker TT, Rock MJ, et al. Femoral 3-in-1 nerve block decreases recovery room time and charges and time to hospital discharge after outpatient knee arthroscopy. Reg Anesth Pain Med 1998, 23:S60.
- Goranson BD, Lang SA, Cassidy JD, et al: A comparison of three regional anesthesia techniques for outpatient knee arthroscopy. Can J Anaesth 1997, 44: 371-376.
- Goranson B., Lang SA, Dust WN Combined femoral 3-in-1 nerve block and intraarticular local anesthesia for knee arthroscopy. Reg Anesth 1995, 20: S29.
- Vloka JD, Hadzic A., Mulcare R., et al: Femoral and genitofemoral nerve blocks versus spinal anesthesia for outpatients undergoing long saphenous vein stripping surgery. Anesth Analg 1997, 84: 749-752.
- Wang H., Boctor B., Verner J. The effect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Reg Anesth Pain Med 2002, 27:139-144.
- Edwards ND, Wright EM Continuous low-dose 3-in-1 nerve blockade for postoperative pain relief after total knee replacement. Anesth Analg 1992, 75:265-267.
- Serpell MG, Millar FA, Thomson MF Comparison of lumbar plexus block versus conventional opioid analgesia after total knee replacement. Anesthesia 1991, 46: 275-277.
- Hirst GC, Lang SA, Dust WN, et al. Femoral nerve block: single injection versus continuous infusion for total knee arthroplasty. Reg Anesth 1996, 21: 292-297.
- Singelyn FJ, Deyaert M, Joris D, et al. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one, block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg 1998, 87: 88-92.
- Bollini CA, Barclay F, Butler S, et al. Bloqueo combinado de los nervios ciatico y femoral para la analgesia postoperatoria en el reemplazo total de rodilla. Rev Arg De Anesthesia 2004, 62:249-258.
- Marchiano AE, Cwik J, Dontelli L, et al. Epidural versus femoral nerve sheath catheter for postoperative analgesia following knee arthroplasty. Reg Anesth 1996, 21: S10.
- Allen JG, Denny NM, Oakman MB Postoperative analgesia following total knee arthroplasty: a study comparing spinal anesthesia and combined sciatic femoral 3-in-1 block. Reg Anesth Pain Manage 1998, 23: 142-146.
- Allen HW, Liu SS, Ware PD, et al. Peripheral nerve blocks improve analgesia after total knee replacement surgery. Anesth Analg 1998, 87: 93-97.
- Mansour NY , Bennetts FE An observational study of combined continuous plexus and single-shot sciatic nerve blocks for post-knee surgery analgesia. Reg Anesth 1996, 21:287-291.
- Berry FR Analgesia in patients with fractured shaft of femur. Anesthesia 1977, 32: 576-577.
- Singelyn FJ, Vanderelst PE, Gouverneur JM Extended femoral nerve sheath block after total hip arthroplasty: continuous versus patient controlled techniques. Anesth Analg 2001, 92:455-459.
- Madej TH, Ellis FR, Halsall PJ Evaluation of “3 in 1” lumbar plexus block in patients having muscle biopsy. Br J Anaesth 1989, 62:515-517.
- Vloka JD, Hadzic A., Drobnik L., et al: Anatomical landmarks for femoral nerve block: a comparison of four needle insertion sites. Anesth Analg 1999, 89: 1467-1470.
- Khoo ST, Brown TCK Femoral nerve block: the anatomical basis for a single injection technique. Anesth Intensive Care 1983, 11:40-42.
- Marhofer P., Nasel C., Sitzwohl C., et al. Magnetic resonance imaging of the distribution of local anesthetic during the three-in-one block. Anesth Analg 2000, 90: 119-124.
- Singelyn FJ, Vanderelst PE, Gouverneur JM Extended femoral nerve sheath block after total hip arthroplasty: continuous versus patient-controlled techniques. Anesth Analg 2001, 92: 455-459.
- Woodley D., Lang SA, Yip RW The femoral 3-in-1 nerve block dose-response relationship revisited. Anesth Analg 1994, 78: S236.
- Ritter JW Femoral nerve “sheath” for inguinal paravascular lumbar plexus block is not found in human cadavers. J Clin Anesth 1995, 7:470-473.
- Cauhepe C., Oliver M., Colombani R., et al. The “3-in-l” block: myth or reality? Ann Fr Anesth Reanim 1989b 8:376-378.
- Parkinson SK, Mueller JB, Little WL, et al. Extent of blockade with various approaches to the lumbar plexus. Anesth Analg 1989, 68: 243-248.
- Seeberger MD, Urwyler A. Paravascular lumbar plexus block: block extension after femoral nerve stimulation and injection of 20 vs. 40 ml mepivacaine 10 mg/ml. Acta Anaesthesiol Scand 1995, 39: 769.
- Farny J., Drolet P., Girard M. Anatomy of the posterior approach to the lumbar plexus block. Can J Anaesth 1994, 41: 480-485.
- Farny J., Girard M., Drolet P. Posterior approach to the lumbar plexus combined with a sciatic nerve block using lidocaine. Can J Anaesth 1994, 41: 486-491.
- Dalens B., Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block of children. Anesth Analg 1989, 69: 705-713.
- Capdevila X., Biboulet P., Bouregba M. et al. Comparison of the three in one and fascia iliaca compartment block in adults: clinical and radiographic analysis. Anesth Analg 1998, 86: 1039-1044.
- Hopkins PM, Ellis FR, Halsall PJ Evaluation of local anesthetic blockade of the lateral femoral cutaneous nerve. Anesthesia 1991, 46: 95-96.
- Brown DL Lateral femoral cutaneous block, in Brown DL (ed): Atlas of Regional Anesthesia (ed 1). Philadelphia, PA, WB Saunders Co., 1992, pp. 99-101.
- Gerard M., Lang SA The lateral femoral cutaneous nerve block revisited: a new transinguinal approach. Anesth Analg 1993, 76: S208.
- Shannon J., Lang SA, Yip RW Lateral femoral cutaneous nerve block revisited: a nerve stimulator technique. Reg Anesth 1995, 20: 100-104.
- Hong Y., O'Grady T., Lopresti D., et al. Diagnostic obturator nerve block for inguinal and back pain. A recovered opinion. Pain 1996, 67: 507-509.
- James CDT, Little TF Regional hip blockade. A simplified technique for the relief of intractable osteoarthritic pain. Anesthesia 1976, 31: 1060-1070.
- Labat G. Regional Anesthesia: Its Technique and Clinical Applications. Philadelphia, PA, W. B. Saunders, 1923.
- Vlocka JD, Hadzic A. Obturator and genitofemoral nerve block. Tech Reg Anesth Pain Manage 1999, 3:1:28-32.
- Wasseff MR Interadductor approach to obturator nerve blockade for spastic conditions of adductor thigh muscles. Reg Anesth 1992, 18: 13-17.
- Parks C.R., Kennedy F.Jr. Obturator nerve block: a simplified approach. Anesthesiology 1967, 28: 775-776.
Techniques in Regional Anesthesia and Pain Management (2006) 10, 150-158