Reasons for the development of neuralgia
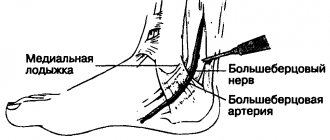
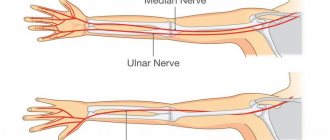
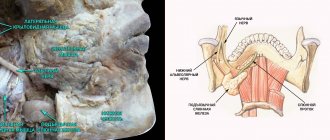
The development of neuralgia in certain nerve fibers is due to their anatomical features. Thus, pathological lesions often develop in nerves that pass through narrow channels and openings.
Essential (primary) neuralgia develops for no apparent reason; clinical examination in this case does not reveal other diseases. It is believed that the cause of essential neuralgia may lie in the pressure that is exerted on the nerve fibers by the vascular arteriovenous connections.
Symptomatic (secondary) neuralgia is caused by systemic pathological processes, such as multiple sclerosis. In multiple sclerosis, the myelin sheath surrounding the nerve fiber is destroyed. The myelin sheath ensures the conduction of nerve impulses and protects the nerve fiber. Further destruction of the nerve fiber occurs. Neuralgia can also be caused by a growing tumor compressing the nerve fiber or a traumatic lesion.
Prevention
Specific prevention of neuralgia of the intercostal nerves has not been developed; general strengthening measures will help prevent the development of pathology. Recommended:
- avoiding hypothermia;
- hardening of the body;
- a healthy lifestyle, including regular moderate physical activity and a rational, balanced diet;
- measures to help prevent spinal curvature or treat an existing curvature;
- timely treatment of spinal diseases, chest injuries, pathologies of internal organs;
- work in comfortable conditions, with prolonged forced body positions, take breaks for a short warm-up.
Symptoms of neuralgia
Neuralgia is characterized by sudden, paroxysmal, piercing, “shooting” pain. Pain syndrome may be accompanied by changes in the color and temperature of the skin in the affected area, as well as local muscle cramps.
Most often, patients suffer from trigeminal neuralgia and intercostal neuralgia.
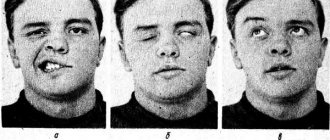
Trigeminal neuralgia is characterized by unbearable pain in the face, gums, and lacrimation. Painful attacks are provoked by talking, chewing, brushing teeth, shaving, and low ambient temperatures. At the same time, redness of the face and spasm of facial muscles occur. Trigeminal neuralgia is characterized by the presence of trigger zones - areas of the skin, touching which can provoke a painful attack.
When examining patients, it is important to exclude all possible secondary variants of trigeminal neuralgia.
With the development of intercostal neuralgia, patients complain of severe pain in the ribs, aggravated by coughing or sneezing. It has been noted that intercostal neuralgia often accompanies osteochondrosis of the thoracic spine.
Treatment of intercostal neuralgia using traditional methods
There are many folk recipes that can be used to treat intercostal neuralgia at home. However, I would like to note that since the reasons causing it are quite serious, you should not self-medicate and check whether the disease can go away on its own. Secondly, it is necessary to accurately confirm the diagnosis, excluding pathologies of the cardiovascular system and other disorders. Otherwise, the underlying disease can be triggered.
- Sage baths with sea salt help relieve tension and reduce pain.
- Rubbing with tincture of valerian or infusion of birch buds is effective - their effect is in no way inferior to industrially produced ointments. However, it is better not to apply alcohol compresses at night - prolonged exposure to alcohol can lead to burns.
- Warming up also helps, but the thermal effect for intercostal neuralgia should not be direct, that is, do not apply a heating pad, hot potato or egg, but wrap yourself in a downy scarf or knitted woolen item. If you heat the painful area too much, the pain will go away for a short time and then such an effect will only increase the swelling of the soft tissues and bring even greater pain.
- For topical application to affected areas, use black radish juice or horseradish juice. Compresses based on steamed flax seeds help a lot.
To prevent chronic neuralgia, it is important to eliminate the effects of harmful concomitant factors, such as psycho-emotional stress, heavy physical activity, alcohol abuse, and also to treat existing diseases of the nervous system, systems and organs, etc.
Treatment of neuralgia
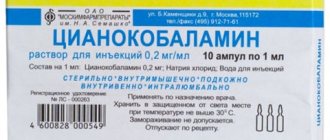
For primary neuralgia, the administration of B vitamins, novocaine injections, and vascular drugs is indicated.
Treatment of secondary neuralgia should be aimed at eliminating the cause that caused the damage to the nerve fibers.
Anticonvulsants are used in the treatment of trigeminal neuralgia. This group of drugs has a pronounced analgesic effect.
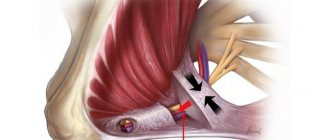
In some cases, if indicated, it is possible to perform neurosurgical intervention - vascular decompression.
Diagnostics
With neuralgia, the patient can first contact a therapist, general practitioner, or ENT doctor, but an accurate diagnosis is made by a neurologist after a neurological examination and additional studies.
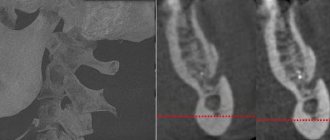
General tests are carried out (general blood and urine tests, blood glucose tests), and special methods are also used for specific neuralgia (MRI, radiography, tests for infections, electroneuromyography, lumbar puncture and others).
Causes of postherpetic neuralgia
Once a person has had chickenpox, the virus remains in the body for life. With age, the immune system weakens (particularly from taking medications or chemotherapy) and the virus can become more active, resulting in shingles.
Damage to nerve endings during rashes leads to postherpetic neuralgia. When damaged, nerve fibers cannot send signals from the skin to the brain as they normally do. Instead, they transmit amplified signals, and the patient feels excruciating pain that can last for months or even years.
Causes of neuropathy of the external cutaneous nerve of the thigh
The most common cause of the disease is pressure on a nerve in the pelvic area. The pathology can be provoked by the use of a corset, too tight underwear, tight belts, pregnancy or excessive weight. Fractures, injuries, spinal diseases, and neuro-reflex abnormalities can also have an effect. All this leads to irreversible transformations, which involve further rubbing of the nerve against the ligament when a person bends over or moves the hip.
Compression of the lateral cutaneous nerve occurs at the level of the iliacus muscle. Among the root causes may be a hematoma in the abdominal cavity, varicose veins, inflammatory processes, surgery or tumors. The disease can develop against the background of bad habits, such as alcoholism, and other diseases (diabetes mellitus, infections, rheumatism).
Analgesic methods
Today, in medical practice, special attention is paid to the elimination of pain. Different countries practice the organization of diverse institutions, the main task of which is the treatment of pain, including pain of unknown origin. As a rule, it is preferable to eliminate pain without the use of narcotics: local anesthetics, blockade of nerve fibers with novocaine, peloid therapy (hot mud applications) are used. Cortisone blockades, which were widely used in the past, are practically not used today, since they have lower effectiveness and are poorly tolerated by patients.
Drug therapy
Drug therapy involves the use of the following groups of drugs:
- Anticonvulsants (Lyrica, Neurontin, others). These drugs have shown good effectiveness against neuropathic pain. However, they have a number of side effects, the most common of which are decreased concentration, drowsiness and swelling of the legs;
- Antidepressants. Some antidepressants (Amitriptyline, Duloxetine) affect the production of special brain substances that are responsible for both depressive states and the perception of pain. Doctors often prescribe minimal doses of antidepressants in the complex treatment of postherpetic neuralgia. Their main side effects include: drowsiness, dry mouth, dizziness;
- In cases of severe pain and insufficient effectiveness of other drugs, patients may be prescribed narcotic analgesics.
Information about the disease
This disease was first described back in 1895 by a neurologist from Russia V.K. Roth and a doctor from Germany M. Bernhardt. Thus, neuropathy of the external cutaneous nerve of the thigh has another name - Bernhardt-Roth disease. Most patients with this diagnosis are over 50 years of age, and the majority are men. Sometimes neuropathy of the external cutaneous nerve of the thigh occurs in pregnant women in the last trimester of pregnancy.
It is worth noting that neuropathy is mostly unilateral, but bilateral nerve destruction can also occur (20%). It is assumed that the pathology can be inherited.
Epidural administration of anesthetics and steroid hormones
Spinal epidural block involves the injection of drugs into the epidural space, which leads to loss of sensation in the area of impact. This means that this procedure involves introducing the active substance directly into the source of pain. Achieving a therapeutic effect in this case is possible due to the following factors:
- analgesic properties of the drug;
- the maximum possible concentration in the affected area;
- reflex action at all levels of the nervous system.
Peroneal nerve neuropathy - how to recognize and treat
The human body is vulnerable to mechanical damage. Most of them are treatable, but in some cases there may be negative consequences. This is not a recurrence of damage, but a new problem. Such consequences include ligament rupture and muscle tissue damage. We are talking about problems with the peroneal nerve - neuropathy. This disease is rare, but takes on a chronic form and has periods of remission accompanied by acute pain. The results of treatment for neuropathy are not always satisfactory - the patient receives temporary relief, but the treatment process is long-term.
It has been noted that a large percentage of patients who develop neuropathy are people:
- Professionally or forcibly spending a lot of time in one position.
- Having fractures of the leg bones, which leads to a long stay of the limbs in a cast.
Both cases are characterized by muscle atrophy, which can result in nerve neuropathy.
Common causes of the disease
The main cause of the disease is trauma to the fibula: bruise, pearl or crack. Nerve damage occurs where it presses against the bone. The length of the affected area varies between a few millimeters and centimeters. This is how tunnel syndrome is formed.
By disrupting blood circulation in damaged tissues, this causes atrophy of muscle tissue and the development of formations in the affected areas. There are known cases of the appearance of neuropathy of the tibial nerve as side effects of intoxication, alcoholism, and drug addiction. It is possible that a cancerous tumor may appear in areas of nerve damage or damage to a ligament called the talofibular ligament.
The danger is that in many cases it all starts with a minor injury, which is paid little attention to and no help is sought. This makes neuropathy difficult to recognize in its early stages.
How to recognize
The following are considered symptoms of neuropathy:
- The area in which the affected nerve is located (lower leg and foot) loses sensitivity to the effects of temperature fluctuations.
- The appearance of pain in a wide range: from mild to severe. Worsened by walking, jumping or squatting.
- The toes become unbendable. This leads to inconvenience in wearing shoes.
- The foot loses its ability to move. This may result in the use of crutches and, in some cases, a wheelchair.
- At the site of disease development (locally), the temperature may rise and the skin may turn red.
The appearance of such symptoms after a leg injury should force a person to consult a doctor and begin treatment if necessary. Inactivity can cause poor posture and, in worst cases, cause neuropathy (compression-ischemic). This will mean that the nerve endings are compressed to such an extent that they begin to die. It is no longer possible to restore such tissue in any way.
How to cure
Patients who develop peroneal nerve neuropathy are treated in a stepwise manner. First you need to relieve the patient of pain and discomfort in general. Then the level of inflammatory processes is localized and reduced. Most often, such measures are sufficient.
Non-hormonal anti-inflammatory drugs are used as the main drugs for treatment: ketorol, diclofenac or nimesulide.
Despite the apparent simplicity of therapy, medications can only be taken with a prescription prescribed by a doctor and after clearly reading the contraindications for their use.
The rapid restoration of nerve tissue is greatly helped by a course of vitamin B. Such drugs are sold in pharmacies, and the course of treatment consists of twenty injections. The most effective are B1, B6, B12. The full course will consist of 60 injections. In addition to restoring nerve tissue, it is necessary to establish blood circulation at the site of inflammation. This can be achieved by taking the medications Trental, Cavinton. After completion of the inflammatory process, the patient is recommended to undergo exercise therapy, massage, gymnastics, and physiotherapy. Folk remedies: lotions and compresses have a beneficial effect on the restoration of areas affected by peroneal nerve neuropathy.
Folk remedies
Here are some simple recipes:
- One way to combat inflammation is goat milk. They moisten gauze and apply it to the inflamed area for two to three minutes. This needs to be done several times during the day until recovery.
- Thoroughly mix two tablespoons of turpentine with three tablespoons of water, pour the resulting solution onto a piece of bread and apply to the sore spot for seven minutes. The procedure should be done before bedtime so that the sore leg is immediately placed in a warm place. You need to complete the course once every two days until recovery. The effect lies in the warming property of turpentine.
It is necessary to clearly understand that folk remedies do not replace medical care provided by doctors, but only supplement it after consultation with the treating doctor.
Surgical intervention
In advanced cases, the treatment methods described above will not lead to the patient’s recovery.
This can happen if the pain occurs frequently and is very severe. For treatment, a plaster splint is applied and orthoses are even prescribed to fix the joint. Failure to achieve a positive result after using these methods will lead to surgery. In such severe cases, only surgery will eliminate the cause of inflammation and restore blood conduction in the muscle tissue, which will contribute to the rehabilitation of the peroneal nerve. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Prognosis for coccydynia
Anococcygeal pain syndrome is very difficult to cure, since it is quite difficult to determine the etiological factors influencing its development, and it often has a pronounced psychopathological component. But still, with an integrated approach, correct and thorough examination of the patient, it is possible to select appropriate treatment tactics and free the patient from this disease.
Anococcygeal pain syndrome is not associated with fatal pathologies of the pelvic organs, spinal bones and perineum; it also does not lead to the development of somatic complications and cannot cause death. But still, coccydynia causes great discomfort and worsens the patient’s quality of life, so it cannot be ignored; patients need to be patient, undergo a full examination and follow all the recommendations of the attending physician.
Ultrasonography
Ultrasound examination of the abdominal cavity makes it possible to diagnose the condition of organs, to exclude concomitant pathologies, and also to evaluate intestinal motility.
To diagnose this disease, other specialists are often involved - a urologist, gynecologist, andrologist. If no other diseases can be identified, and a symptom complex exists, the doctor can make a diagnosis - anococcygeus pain syndrome. Particular attention is paid to the psycho-emotional state of the patient, because there is a high probability that the cause of anococcygeus pain syndrome is a mental imbalance.
Therapeutic exercise and rehabilitation methods
Using physical therapy techniques, it is possible to improve the condition of nervous and muscle tissue, restore muscle tone and partially restore the functions of damaged nerves. During physical exercise, metabolism increases, breathing and blood supply to tissues improves, and the body's resistance to the negative influences of external factors is normalized. Exercise therapy and other methods of rehabilitation for neuralgia are necessarily included in the recovery plan (during non-exacerbations). It has been established that a complex of exercise therapy methods in combination with electrical stimulation is especially effective.
Classification of coccydynia
The classification of coccydynia implies the presence of two types of this disease:
- primary coccydynia, the cause of development is direct injury to the coccyx;
- secondary coccydynia has many etiological factors (proctological, urological, gynecological pathologies, etc.).
This form includes two subtypes:
- anorectal pain (pain in the perineum, buttocks, anus and rectum);
- proctalgia (pain spreads mainly along the rectum).