Dizziness
It happens that there are no physiological reasons for dizziness. The body, at first glance, is healthy and works great, but the head still feels dizzy again and again. If something similar has happened to you, think about how you felt before the dizziness. Perhaps severe fear or anxiety? Panic? In this case, it is quite possible that your dizziness was psychogenic.
Psychogenic dizziness is dizziness caused by a person's psychological or emotional state. Sometimes it is called imaginary because, unlike true dizziness, it is not associated with a disruption of the vestibular apparatus. [1] Actually, this is why the sensations during attacks of vestibular and psychogenic dizziness are so different: vestibular dizziness is similar to movement, rotation, and psychogenic dizziness is similar to fog in the head, instability, fear of falling, lightheadedness, etc. [2][3]
Despite the fact that psychogenic dizziness occurs due to emotional problems, its symptoms can be very real. For example, shortness of breath, sweating, tinnitus, headache, rapid heartbeat, etc. [1]
How to understand that dizziness is psychogenic?
Only a specialist can find out. During diagnosis, he must, first of all, exclude all other possible causes of dizziness. To do this, he needs to find out from you as much as possible about the conditions under which attacks occur, how long they last and what they look like, whether they are accompanied by other symptoms, etc. In some cases, additional examination by several specialists (otoneurologist, cardiologist, hematologist, etc.), laboratory and radiation diagnostics, as well as additional studies (for example, a study of balance or the condition of the inner ear, ECG, etc.) may be necessary. [2][3]
After the doctor is convinced that you have psychogenic dizziness, you need to understand what kind of disorder caused it. Most often these are [1]:
Anxiety or anxiety-depressive disorders (they are felt as anxiety, constant fears for loved ones, sudden mood swings, worry about little things, tension, stiffness, loss of sleep, decreased performance, increased fatigue, muscle and other pain, etc.) [ 4]
Panic disorder (characterized by recurrent panic attacks and anxiety in anticipation of a new attack). [5] Panic attacks include fear, shortness of breath, palpitations, nausea, weakness, lightheadedness, lightheadedness, fear of falling, and loss of balance. Panic attack is one of the most common anxiety disorders, which approximately 3% of the population has experienced at least once in their lives. [6]
Phobic postural vertigo can be described as a feeling of instability in the form of attacks. Simply put, it feels like a momentary loss of balance. It can occur spontaneously, but is more often associated with specific stimuli or situations that cause fear (i.e., phobias). [4][7]
Symptoms of a panic attack
- hyperhidrosis (excessive sweating);
- muscle tremors, chills;
- tachycardia;
- dystonic or physiological tremor;
- hot flashes (instant sensations of heat);
- asphyxia (suffocation);
- dyspnea (difficulty breathing, shortness of breath, feeling of lack of air);
- irradiation of pain to the left side of the chest;
- nausea, urge to vomit;
- abdominal pain syndrome (stomach pain);
- sensation of a foreign body, coma in the throat;
- paresthesia (tingling in the limbs, feeling of numbness);
- lightheadedness, dizziness;
- stool disorders (constipation, diarrhea);
- dysbasia (gait disturbance);
- high blood pressure;
- impairment of vision and/or hearing;
- frequent urination.
- derealization (feeling of unreality, alienation, indistinctness of the surrounding reality);
- fear of schizophrenia, obsessive fear of going crazy, losing control over one’s actions;
- disorientation, confusion;
- depersonalization (the patient perceives his actions as if from the outside and feels that he cannot control them);
- interrupted sleep, insomnia (insomnia), nightmares;
- Thanatophobia (fear of death).
- more frequent repetition of attacks with the appearance of new symptoms;
- isolated attacks;
- the addition of depressive symptoms (sleep disturbances, loss of appetite, persistently depressed mood);
- constant fear for your health;
- refusal to perform habitual life rituals (patients stop traveling in public transport, going outside, and their performance sharply decreases).
What does a person experience during a panic attack?
- feeling of fear of varying strength;
- feeling of impending danger;
- fear of death;
- stiffness reaching the point of stupor (in some people);
- motor activity (in others);
- fear of committing an uncontrollable act;
- fear of going crazy;
- confusion of thoughts;
- unreality of what is happening;
- loss of orientation in personality, space and time.
Physical symptoms of a panic attack
The main reason for their appearance is the release of biologically active substances (norepinephrine and adrenaline) into the blood in large quantities. Mediators have a stimulating effect on the nervous, respiratory systems, heart and blood vessels.
- Rapid breathing and heart rate.
- Shortness of breath, lack of air.
- Chills.
- Dry mouth.
- Increased sweating.
- Weakness, body numbness, dizziness.
- Diarrhea.
- Involuntary urination.
- Vomit.
The most pronounced physical symptoms are in anxiety, which develops due to pathology of organs and systems.
Treatment of psychogenic dizziness
Many doctors deal with the problem of dizziness, but when treating psychogenic dizziness, consultations with a neurologist and psychotherapist are especially important.
Typically, complex therapy is used to treat psychogenic dizziness, which includes both medicinal (including antidepressants) and non-medicinal treatment methods. [5] Of great importance are:
• vestibular gymnastics, which is aimed at training and reducing the excitability of the vestibular apparatus; [7]
• breathing exercises, which help reduce hyperventilation (its manifestations include lack of air, dissatisfaction with inhalation, inability to take a full breath, etc.);
• psychotherapy.
It has long been proven that a person’s psychological health is as important as physiological health. [4] Keep this in mind and be sure to consult a specialist if you feel dizzy.
Diagnostics
Diagnosis begins, first of all, with a consultation with a doctor. The doctor may be primarily interested in answers to the following questions:
- Is the dizziness continuous or sporadic?
- If the dizziness occurs in episodes, how long did the episode last?
- How often do episodes of dizziness occur?
- What triggers episodes of dizziness?
- Does the sensation of spinning, moving around, or spinning your body itself make you dizzy?
- Is dizziness accompanied by a feeling of weakness?
- Does dizziness cause imbalance?
- Is dizziness accompanied by ringing, a feeling of fullness in the ears, or hearing loss?
- Are there any visual impairments?
- Does dizziness get worse when you change your head position?
- What medications, vitamins, or nutritional supplements is the patient taking?
The doctor thus narrows down the range of conditions that may be causing dizziness. A neurological examination helps identify the presence of neurological symptoms. After a physical examination, your doctor may prescribe additional tests.
- Eyeball movement test. The doctor may observe the movement of the patient's eyeballs while tracking a moving object. In addition, a test may be performed where cold or warm water is poured into the ear and eye movements are observed.
- Posturography. This method allows you to determine which parts of the balancing system are out of order.
- Vestibular testing also allows you to determine the degree of stability of the vestibular apparatus.
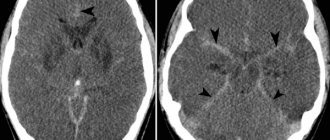
In some cases, magnetic resonance imaging (MRI) may be needed. An MRI may be done to rule out acoustic neuroma or other problems in the brain that may be causing the dizziness.
Laboratory research methods are necessary in cases where there is suspicion of somatic diseases (for example, anemia).
Bibliography:
1. Filatova E. G. Diagnosis and treatment of psychogenic dizziness // Attending physician. –2009. - No. 5/9. — https://www.lvrach.ru/2009/05/9155798/ (Access date: 07/18/2016).
2. Drapkina O.M., Chaparkina S.M., Ivashkin V.T. Dizziness in the practice of an internist // Cardiovascular therapy and prevention. – 2007. – No. 6 (4). – pp. 107-114.
3. Zamergrad M.V. Vestibular vertigo // Neurology, neuropsychiatry, psychosomatics. – 2009. – No. 1. – P. 14-18.
4. Sitdikova A.I. et al. Psychogenic dizziness: clinical features and diagnostic principles // Bulletin of modern clinical medicine. – 2015. – T.8. — No. 6. – pp. 76-79.
5. Filatova E. G. Anxiety in neurological practice // Lech. nervous bol. – 2005. – No. 1. – P. 7–14.
6. Melnikov A. N., Stanko E. P. Panic attacks in children and adolescents // Journal of the Grodno State Medical University. – 2005. – No. 3 (11). – pp. 33-35.
7. Golubev V.L., Vein A.M. Neurological syndromes. – M.: Eidos Media, 2002. – 832 p. – pp. 695–704.
Therapeutic exercise to improve the functioning of the cardiovascular system.
Dizziness
G
dizziness is one of the symptoms most often encountered in medical practice. Among the reasons for visiting doctors of all specialties, it accounts for 2–5% [12].
The cause of dizziness is an imbalance of sensory information coming from the main afferent systems that provide spatial orientation - vestibular, visual and proprioceptive. Disturbances in central information processing and the efferent part of the motor act are also of great importance. In addition, pathology of the musculoskeletal system plays a certain role [2,4,8, 9,11,12,16,14].
In most cases, dizziness is caused by one of the following conditions:
: peripheral vestibular disorders, multiple sensory deficits, psychogenic causes, circulatory disorders in the brain stem, other diseases of the central nervous system, cardiovascular diseases. A combination of several reasons is possible [12,14].
Patients can describe a wide variety of sensations as “dizziness,” so the primary diagnostic task is to clarify the nature of the patient’s complaints. Typically, they can be classified into one of four clinical types of dizziness [1,2,4,9,11,12,14,16].
Systemic or vestibular vertigo
– a feeling of rotating, falling, tilting or swaying of one’s own body or surrounding objects. Often accompanied by nausea, vomiting, hyperhidrosis, impaired hearing and balance, as well as oscillopsia (the illusion of rapid small-amplitude vibrations of surrounding objects). Systemic vertigo is characteristic of damage to the vestibular system - both its peripheral and central parts.
Presyncope
. Patients note a feeling of lightheadedness, impending loss of consciousness, and “lightness” in the head. Often combined with pallor of the skin, palpitations, a feeling of fear, darkening of the eyes, nausea, and increased sweating. The most common causes are heart disease and orthostatic hypotension.
In some cases, by “dizziness”, patients mean imbalance
. There is instability, unsteadiness when walking, and a “drunk” gait. It is characterized by a combination with paresis, sensitivity disorders, incoordination and oscillopsia. Symptoms caused by imbalance are observed during standing and walking and are absent in sitting and lying positions [1,4,12,16,14].
For psychogenic dizziness
, observed, in particular, within the framework of anxiety, conversion disorders or depression, is characterized by difficult-to-describe sensations that do not correspond to the previous types of dizziness [1,12]. Patients may complain of “fog,” “heaviness” in the head, a feeling of intoxication, and lightheadedness. It should be noted that similar vague symptoms can occur in the early stages or during the atypical course of organic diseases [12].
Along with the clinical type of dizziness, its course, the presence of provoking factors and accompanying symptoms are of diagnostic importance [4,11]. A single episode of systemic vertigo is most often caused by a brainstem or cerebellar stroke. Repeated attacks of dizziness can develop either for no apparent reason or due to certain provoking factors. Spontaneous attacks of dizziness, not provoked by sudden movements of the head, usually serve as a manifestation of arrhythmias, transient ischemic attacks (TIA) in the vertebrobasilar region, Meniere's disease or epileptic seizures. Recurrent attacks of dizziness, in which provoking factors are identified (changes in body position, turning the head), are most often caused by benign paroxysmal positional vertigo (BPPV) or fainting, in particular orthostatic.
Systemic dizziness
The most common cause of systemic dizziness is BPPV [4,8,12,14]. The disease usually develops after middle ear infections, traumatic brain injury, or otological surgery. Characteristic are short-term (no more than 1 minute) attacks of systemic dizziness that occur when changing body position. In the pathogenesis of BPPV, the leading role is played by cupulolithiasis - the formation of a clot of calcium carbonate crystals in the cavity of the semicircular tubule, which leads to an increase in the sensitivity of the receptors of the semicircular tubules. To detect positional vertigo, the Nilen-Barany
. From a sitting position, the patient quickly lies on his back, with his head tilted back 45° and turned to the side 45°. The position is maintained for 30–40 seconds. The test is repeated with the head positioned along the midline and when turned in the opposite direction. The development of positional vertigo and nystagmus confirms the diagnosis. Isolated positional nystagmus also speaks in favor of BPPV - when the eyeballs are fixed in the middle position, the nystagmus is vertical-rotatory, with a fast phase directed upward and towards the underlying ear. When looking towards the underlying ear, the fast phase of nystagmus is directed in the same direction, horizontal-rotatory nystagmus, when looking in the opposite direction - vertical, beating upward. There is a characteristic latent period (30–40 seconds) between the start of the test and the onset of nystagmus. The nystagmus fades when the test is repeated. Positional nystagmus is observed inconsistently, more often during an exacerbation [10]. BPPV must be differentiated from central positional vertigo and nystagmus, the most common causes of which include spinocerebellar degenerations, brainstem tumors, Arnold-Chiari malformation, and multiple sclerosis. Central positional nystagmus has no latent period, its duration exceeds 1 minute, the direction of nystagmus can vary, often vertical nystagmus does not fade with repeated examination. To treat BPPV, exercises are used to move calcium carbonate crystals from the semicircular tubule into the cavity of the elliptical sac. Repeated provocation of dizziness is also effective, which leads to its gradual regression due to central compensation.
The combination of systemic dizziness with focal neurological symptoms is characteristic of circulatory disorders in the vertebrobasilar system, as well as tumors of the cerebellopontine angle and posterior cranial fossa [4, 5, 12, 14]. With vertebrobasilar insufficiency, dizziness, as a rule, develops suddenly and persists for several minutes, often accompanied by nausea and vomiting. As a rule, it is combined with other symptoms of ischemia in the vertebrobasilar region [10]. Early stages of vertebrobasilar insufficiency can manifest as episodes of isolated systemic dizziness [15]. Longer episodes of isolated systemic vertigo suggest other diseases, particularly peripheral vestibular disorders. Along with systemic dizziness, TIAs and strokes in the vertebrobasilar region can also manifest as imbalance.
Systemic dizziness, nausea and vomiting are the earliest symptoms of ischemia in the anterior inferior cerebellar artery.
, leading to the development of infarction of the caudal parts of the tegmentum of the pons (lateral inferior pontine syndrome, Gasperini syndrome). Similar symptoms are observed with cerebellar infarction [19,23]. Such symptoms require a differential diagnosis with peripheral vestibular disorders. With damage to the cerebellum, in contrast to damage to the labyrinth, the fast component of nystagmus is directed towards the lesion. Its direction changes depending on the direction of gaze, but nystagmus is most pronounced when looking in the direction of the lesion. Fixing the gaze on any object does not affect nystagmus and dizziness. In addition, there is discoordination in the limbs, which is absent when the labyrinth is affected [6,9,14].
Acute systemic dizziness, both isolated and in combination with suddenly developed deafness, is characteristic of labyrinthine infarction
. Deafness caused by labyrinthine infarction is usually irreversible, while the severity of vestibular disorders gradually decreases. A combination of labyrinth and brainstem infarction is possible [6,19,23].
Systemic dizziness is a cardinal symptom of peripheral vestibular disorders
. The most important sign that makes it possible to differentiate peripheral vestibular disorders from central ones is nystagmus - most often horizontal, directed in the direction opposite to the lesion and intensifying when looking in the same direction. In contrast to central lesions, gaze fixation reduces nystagmus and vertigo [4–6,9,12,24,16,14].
Acute development of systemic dizziness in combination with nausea and vomiting is characteristic of viral neurolabyrinthitis
(vestibular neuronitis, vestibular neuritis). Symptoms usually regress within a few days, in severe cases - after 1-2 weeks. Typically, symptoms develop 1–2 weeks after a respiratory infection [4,5,12,14].
Meniere's disease
manifests itself as repeated episodes of severe systemic dizziness, accompanied by decreased hearing, a feeling of fullness and noise in the ear, nausea and vomiting. Within a few minutes, the dizziness reaches its maximum and gradually, over the course of several hours, goes away. Hearing impairment in the early stages of the disease regresses completely and then becomes irreversible. Balance problems may occur for several days after an attack of Meniere's disease. The first attacks of the disease may manifest as isolated systemic dizziness. To confirm the diagnosis, audiometry is performed. A hearing loss of more than 10 dB at two different frequencies is typical. The cause of Meniere's disease is recurrent swelling of the labyrinth, which develops as a result of rupture of the membrane separating the endolymph from the perilymph [1,4,14].
Treatment
Treatment of systemic dizziness is largely determined by its cause; in addition, symptomatic therapy plays an important role. Specific treatment for systemic vertigo is known only for a limited range of diseases. Dizziness as part of vertebrobasilar insufficiency requires the prescription of antiplatelet agents
(acetylsalicylic acid 75–330 mg/day, ticlopidine 500 mg/day), and if symptoms increase,
anticoagulants
[6]. For viral neurolabyrinthitis, symptomatic therapy is carried out. The effectiveness of antiviral drugs and glucocorticoids has not been proven [4,5,8,12,14].
Treatment of attacks of Meniere's disease is symptomatic. Betahistine is the most effective
[1,3]. For prevention, a low-salt diet and diuretics are prescribed [4,8].
For the symptomatic treatment of systemic dizziness, vestibulolytic agents are used that act on vestibular receptors or on central vestibular structures, mainly the vestibular nuclei. The first include antihistamines
: meclozine is prescribed 12.5–25 mg orally 4 times a day, promethazine – 25–50 mg orally, intramuscularly or rectally 4–6 times a day.
Benzodiazepines
have a central vestibulolytic effect : oxazepam - 10-15 mg orally 4 times a day, diazepam - 5-10 mg orally, IM or IV 4-6 times a day. Also used is the histamine receptor stimulator betahistine - 8-16 mg orally 2-3 times a day, calcium antagonists (cinnarizine 25-50 mg orally or intramuscularly 4 times a day, flunarizine 10 mg per day in the afternoon) [3, 8,13,18].
An effective treatment for dizziness is the combination drug Phezam
, containing 400 mg of piracetam and 25 mg of cinnarizine. The effect of the drug is complex, including vasoactive and metabolic effects [7,20]. The combination of two components in the drug leads to an increase in their therapeutic effect without increasing toxicity. In addition, Phezam was noted to be more effective and tolerable compared to separate administration of its components [17,19].
A number of double-blind, placebo-controlled studies have shown the high effectiveness of Phezam in systemic vertigo caused by both central and peripheral vestibular disorders [17,19]. The drug also reduced the severity of dizziness during the presyncope state. Fezam is effective in patients with chronic cerebrovascular insufficiency, who showed significant improvement in cognitive functions during treatment. The drug is prescribed 2 capsules 3 times a day for 3–6 weeks.
To relieve nausea and vomiting
Prescribe prochlorperazine 5-10 mg orally or intramuscularly 4 times a day, 25 mg rectally once a day or metoclopramide - 5-50 mg orally, intramuscularly or intravenously 4-6 times a day. Thiethylperazine has a central vestibulolytic and antiemetic effect. Prescribe 6.5 mg orally, rectally, subcutaneously, intramuscularly or intravenously 1–3 times a day [5,6,12,16,18]. A combination of antihistamines and benzodiazepines is effective. To reduce the sedative effect of vestibulolytic drugs, it is recommended to prescribe methylphenidate hydrochloride 5 mg orally 2 times a day (in the first half of the day) [12]. Vestibulolytic agents should be prescribed only for acute systemic dizziness. Their use should be as short as possible, since long-term use slows down the process of central compensation of the defect [6,12,16,18].
The main principle of rehabilitation for peripheral vestibular disorders is the stimulation of central compensation
by repeated stimulation of vestibular receptors. It is necessary to start rehabilitation as early as possible. With damage to the central vestibular structures, rehabilitation is much less effective [5,6,8,16].
Balance imbalance
One of the causes of imbalance is chronic vestibular dysfunction. Characteristically, symptoms intensify in the dark, when it is impossible to compensate for the defect with the help of vision. Oscillopsia is often observed, possibly combined with hearing impairment. The most common cause of chronic bilateral labyrinthine lesions is the use of ototoxic drugs. Worsening imbalance in the dark is also characteristic of deep sensitivity disorders. The most pronounced imbalances develop in cerebellar disorders. Visual control does not affect the severity of symptoms. With damage to the flocculonodular parts of the cerebellum, oscillopsia is often observed, as well as nystagmus, depending on the direction of gaze. One of the mechanisms of imbalance is also disorders of cervical proprioception. The causes of imbalance caused by changes in the efferent part of the motor act include multiple subcortical infarctions, normal pressure hydrocephalus, Parkinson's disease, chronic subdural hematoma, tumors of the frontal lobes, as well as a number of medications - anticonvulsants (difenin, phenobarbital, finlepsin), benzodiazepines, antipsychotics ( phenothiazines, haloperidol), lithium preparations. Impaired balance is a characteristic symptom of tumors of the cerebellopontine angle, temporal bone and posterior cranial fossa. Systemic dizziness is observed much less frequently with this pathology. In the vast majority of cases, concomitant neurological symptoms are detected. In addition, one of the causes of imbalance, observed mainly in the elderly, is multiple sensory insufficiency - a combination of moderate disorders of several sensory functions. Disturbances in the central integration of sensory information play a certain role in its development [4,8,9,11,12,16,14].
Psychogenic dizziness
Psychogenic dizziness most often occurs as part of agoraphobia, depression and panic attacks, and also, usually in the form of a presyncope, serves as a manifestation of hyperventilation syndrome [4,12,14]. With dizziness of an organic nature, it is also possible to develop restrictive behavior, in particular, secondary agoraphobia or reactive depression. In some cases, there is a combination of episodes of organic and psychogenic dizziness, as well as the development of dizziness of mixed origin [14]. Treatment is determined by the nature of the underlying disorder. Psychotherapy is of great importance. It is necessary to explain to the patient the essence of his existing disorders, since often an additional psychotraumatic factor is the belief that he has a life-threatening disease [4,8,12,16].
The list of references can be found on the website https://www.rmj.ru
Piracetam + Cinnarizine –
Fezam (trade name)
(Balkanpharma)
Literature:
1. Weiss G. Dizziness // Neurology Edited by M Samuels - M, Practice, 1997–P 94–120.
2. Lavrov A.Yu., Shtulman D.R., Yakhno N.N. Dizziness in the elderly // Neurological journal – 2000 – T 5, N 5 – P 39–47.
3 Lavrov A.Yu. Application of betaserc in neurological practice // Ibid –2001 –T6.N2–C35–38.
4. Baloh RW Dizziness in older people//J Am Genatr Soc–1992–Vol 40, N 7 –P 713–721.
5. Baloh RW Dizziness and verigo // Office of practice of neurology Eds MA Samuels, S Feske – New York, 1996 – P 83–91.
6. Baloh RW Vertigo //Lancet –1998 –Vol 3 52 –P 1841–1846..
7. Ban T. Psychopharmacology fot the aged – Basel, Karger, 1980.
8. Brandt T. Vertigo // Neurological disorders Course and treatment Eds T Brandt, LP Caplani, J Dichgans et al – San Diago, 1996 – P 117–134.
9. Daroff R.V., Martin JB Dizziness and vertigo // Harrison's principles of internal medicine Eds Fauci AS, Braunwald E., Isselbacher KJ et al – 14th ed – New York, 1998 – P 104–107.
10. Davies RA Disorders of balance // Handbook of vestibular rehabilitation Eds LM Luxon, RA Davies – London, 1997 – P 31–40.
11. Derebery MJ The diagnosis and treatment of dizziness // Med Clin North Am –1999–Vol 83,N 1–P 163–176.
12. Drachman DA A 69–year–old man with chronic dizziness // JAMA –1998 –Vol 290, N 24–Р21П–2118.
13. Fraysse V., Bebear JP, Dubreuil S. et al Betahistine dihydrochloride versus flunarizine A double–blind study on recurrent vertigo with or without cochlear syndrome typical of Memere's disease // Acta Otolaryngol (Stockh) – 1991 – Suppi 490 – P 1 -10.
14 Furman JM, Jacob RG Psychiatric dizziness // Neurology–1997–Vol 48, N 5–P 1161–1166.
15 Gomez S.R. , Cruz-Flores S., Malkoff MD et al. Isolated vertigo as a manifestation ofvertebrobasilar ischemia // Neurology –1996 –Vol 47 –P 94–97.
16. Hollander J. Dizziness//Semin Neurol–1987–Vol 7, N 4–P 317–334.
17. Konstantinov K., Yordanov Y. Clinical and experimental–psychological studies in cerebral atherosclerosis //MBI–1988–Vol 6–P 12–17.
18. Luxon LM. Modes of treatment of vestibular symptomatology // Handbook of ves–tibular rehabilitation Eds LM Luxon, RA Davies – London, 1997 – P 53–63.
19.Popov G., Ivanov V., Dimova G. et al Phezam - clinical and psychoogical study // MBI-1986-Vol 4-P3-6.
20. Temkov I. Yordanov Y., Konstantinov K. et al. Clinical and experimental–psuchological studies of the Bulgarian drug pyramem // Savr Med–1980–Vol 31, N9–P 467–474.
21. Troost T.V. Dizziness and vertigo // Neurology in clinical practice Eds WG Bradley, R.V. Daroff, G.M. Fenichel, S.D. Marsden 2nd ed – Boston, 1996 – P 219–232.
Mechanisms of maintaining balance
The mechanisms for maintaining balance in humans include: the vestibular, visual systems, deep and superficial sensitivity. All information is integrated in the central nervous system (CNS) and is modulated by the activity of the reticular formation, the extrapyramidal system of the brain, and the frontotemporal lobes of the cerebral hemispheres. The primary role is played by the vestibular receptors; they determine the forces of gravity and translate information into impulses that are deciphered by the brain (Luxon, 1984). As a result of this, a person is aware of the position of the head and body in space, information is available to him that controls postural movements. The activity of the vestibular nuclei (superior, lateral, medial and inferior) is modulated and integrated by multiple afferent inputs (Brodal, 1974). It is known that the vestibular nuclei are connected with five physiological systems: the oculomotor nuclei through the longitudinal medial fasciculus by multisynaptic connections with the reticular formation; the motor part of the spinal cord through the reticulospinal tract and partly the medial longitudinal fasciculus; cerebellum; the autonomic nervous system, so a “floor” in this branched system in any department can lead to a feeling of dizziness and loss of balance.
Treatment
Conservative therapy
Mild dizziness caused by physiological factors is eliminated by normalizing nutrition, daily routine, reducing stress levels, and ensuring sufficient ventilation in the premises. To normalize the condition of women during menopause, hormone replacement therapy is carried out and antidepressants are prescribed.
In case of dizziness caused by taking medications, the dose is adjusted, the drug is discontinued or replaced. Therapeutic tactics for other pathologies are determined by the nature of the disease:
- VSD
. The most important role is played by non-drug measures: correction of the work and rest regime, elimination of physical inactivity and unnecessary emotional influences, psychotherapy, physiotherapy. If the effectiveness is insufficient, tranquilizers, antidepressants, nootropics, and sedatives are used. - Cerebral atherosclerosis
. A special diet, regular exercise, and avoidance of smoking and alcohol consumption are required. Drug correction of hyperlipidemia is carried out. Antiplatelet agents, vascular agents, B vitamins, and nootropics are used. - Arterial hypotension
. Treatment of the underlying disease is required. Therapeutic and recreational activities include massage, hydrotherapy, acupuncture, aromatherapy, exercise therapy. Herbal adaptogens, cerebroprotectors, antioxidants, and antidepressants are effective. - Cervical osteochondrosis
. During periods of exacerbation, wearing a Shants collar is recommended. As part of drug therapy, NSAIDs, muscle relaxants, and painkillers are used. - Endocrine diseases
. For patients with diabetes mellitus, mild dizziness requires adjustment of diet, insulin therapy regimen, or treatment with hypoglycemic drugs. Hypothyroidism requires replacement therapy with levothyroxine.
For iron deficiency anemia, a nutritious diet with a high content of heme iron and taking iron supplements are recommended. Patients with neurotic disorders are given psychotherapy and prescribed antidepressants and tranquilizers.