Forecast
The prognosis depends on many factors: timeliness of assistance provided, general health, quality of treatment. In addition, the consequences of a stroke depend on the type of stroke, namely the area of the brain affected.
Let's look at the main types of stroke by area and their health consequences.
Major stroke
The outcome for the elderly is unfavorable, since the patient does not fully recover. The result is disability.
Unilateral stroke
The prognosis is influenced by the extent of the lesion and the timeliness of medical care. Often the outcome is death or paralysis. Only in isolated cases does the patient recover completely.
Brainstem stroke
The most dangerous species, often leading to death. The survivors remain disabled.
Cerebellar stroke
The prognosis depends on the extent of the lesion. If treatment is started in a timely manner and the patient is properly cared for during the rehabilitation period, he can fully or partially recover. However, most stroke survivors suffer from impaired mobility, which causes them to walk with support.
Spinal stroke
The prognosis is generally favorable and the mortality rate is low. If treatment is not started in time, the patient can be paralyzed. Problems in the functioning of the pelvic organs cannot be ruled out.
If you are over 80 years old
For people over 80 years of age, the prognosis is rarely good, regardless of the type of stroke. The fact is that at such a respectable age the condition is complicated by existing chronic diseases and weakened immunity, which reduces the chances of recovery.
Elderly people at this age most often fall into a coma, during which they do not breathe on their own. Their blood pressure decreases, which leads to impaired blood circulation. Fever may occur. Lives in a coma for an average of 7 days, after which he dies.
In less severe cases (with a unilateral stroke), the patient remains disabled due to paralysis of the side of the body opposite to the lesion and other disorders.
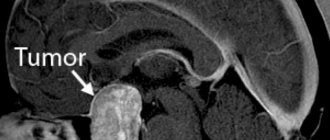
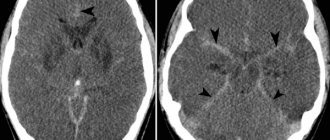
According to the European Stroke Organization (ESO) Guidelines, 2008
- All patients with suspected TIA or stroke are recommended to undergo CT or MRI examination.
- In patients with TIA, minor stroke and spontaneous regression of symptoms, urgent vascular imaging methods (ultrasound, CT or MR angiography) are recommended.
- In patients with acute stroke and TIA, early clinical evaluation is recommended, including assessment of physiological parameters, as well as routine blood tests.
- A 12-lead ECG is recommended for all patients with TIA and acute stroke.
- For patients with stroke and TIA, Holter ECG monitoring is recommended after the acute period of the disease in the presence of arrhythmia and an unknown type of stroke.
- Echocardiography is recommended only in certain patients
Ischemic stroke of unknown etiology (cryptogenic) requires additional laboratory testing:
- Proteins C and S;
- C-reactive protein;
- Homocysteine;
- Antiphospholipid antibodies.
Confirmation of the diagnosis of stroke and its nature, the choice of treatment tactics is possible only with the availability of neuroimaging methods!
- All patients with suspected transient ischemic attack (TIA) and stroke should be hospitalized.
- Emergency hospitalization should be carried out in a specialized department for acute cerebrovascular accidents in a multidisciplinary hospital (“stroke units”) with specialized multidisciplinary care, neuro- and angiosurgical capabilities, including the provision of high-tech care, which reduces mortality and improves the outcome of the disease.
Consequences of a stroke
Unfortunately, as a result of brain damage, important functions are impaired, which are not always amenable to recovery. Let's look at the main ones.
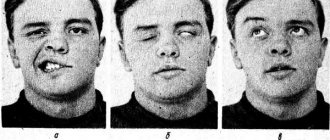
Paralysis
It involves damage to the nerve endings that control muscle function, resulting in loss of motor function. Paralysis can be of the whole body or part of it. The most common form is one-sided. May affect facial muscles.
Speech dysfunction
A common consequence of a stroke that occurs due to damage to the areas of the brain responsible for speech. Expressed in complete/partial loss of the ability to speak and perceive the words of others. With a partial form, the conversation is unclear; with a complete form, there is an inability to utter at least a word.
Deterioration of the visual organs
A stroke can damage the parts of the brain responsible for visual function. As a result, there is deterioration in vision, loss of individual parts from the field of view (up to ½), and strabismus (difficult to treat).
Impaired motor coordination
Most often occurs with a brainstem stroke. Manifests itself in the form of dizziness and staggering when moving. Depending on the form of the pathology and severity, it may manifest itself during the first days after the attack or over a longer period.
Swallowing dysfunction
It occurs due to a disruption of the reflex process or paralysis of facial muscles. It is also a consequence of brainstem infarction.
May manifest:
- Difficulty chewing food.
- Difficulty swallowing food.
- Pain while eating.
- The entry of food particles from the oral cavity into the respiratory organs, in particular the nose.
Formation of bedsores
It is observed in paralyzed patients due to prolonged stay in one position. In this case, less nutrients reach the tissues. The result is their starvation and further death. The areas most affected are areas closely pressed to the bed.
Pneumonia
As a result of paralysis, the patient cannot cough up the mucus that accumulates in the bronchi and enters the lungs. Next, inflammation begins.
Depressive state
The most common consequence that minimizes the effectiveness of treatment and rehabilitation. You need the help of a qualified psychologist and a course of antidepressants.
Coma
One of the dangerous consequences, considered a transitional state to death. During this period it is noted:
- slowing down metabolism;
- decrease in body temperature;
- change in breathing pattern;
- falling into unconsciousness;
- lack of response to external stimuli.
The prognosis for coma is predominantly unfavorable.
Special methods for the treatment of acute stroke. Reperfusion therapy
Basic reperfusion methods:
- restoration and maintenance of systemic hemodynamics (maintaining blood pressure at a sufficient perfusion level, which is reflected in Basic therapy);
- Thrombolysis;
- hemangiocorrection (anticoagulants and antiplatelet agents).
Reperfusion should be active and short-term with a reperfusion period of no more than 3-6 hours.
Thrombolytic therapy (TLT)
- the only method with a high degree of evidence leading to recanalization, provides complete physical independence in 1 out of 10 treated patients.
Types of TLT:
- 1. Drug TLT: systemic intravenous thrombolysis (IV TLT);
- selective (intraarterial) thrombolysis (V/A TLT);
- combined thrombolysis (V/A + mechanical);
- staged thrombolysis (V/V+V/A or mechanical) – rt-PA bridging.
- Ultrasound destruction of thrombus
When a patient is admitted with a stroke clinic during the “therapeutic window” period, it is necessary to immediately resolve the issue of indications and contraindications for intravenous thrombolysis.
In any case, it is better to treat than not to treat!
IA TLT is indicated for patients with occlusion of the proximal segments of intracerebral arteries. Its use requires the patient to remain in a high-level stroke center with 24-hour access to cerebral angiography. IA TLT is the method of choice in patients with severe ischemic stroke lasting up to 6 hours, for stroke in the VBB - up to 12 hours. During endovascular intervention, it is possible to administer a thrombolytic intravenously (only on the basis of an accepted and approved internal protocol due to the lack of an authorization document for the use of thrombolysis outside the 4.5 hour “therapeutic window” and the use of mechanical recanalization methods.
It is important that the possibility of endovascular (I/A) intervention should not be a reason for refusing IV TLT in accordance with the indications.
The following patients may be candidates for endovascular technologies:
- 1. IV TLT beyond the time frame (up to 6 hours in patients with cerebral infarction in the carotid system);
- 2. With an unknown time - “night” stroke (up to 8 hours) with occlusion of the main artery, because inaction is fatal!
- 3. With occlusion of the distal parts of the ICA, with T-occlusion, with occlusion of the M1 and M2 segments of the MCA, with basilar occlusion, after ineffective IV TLT. At the same time, verification of recanalization is not required for transfer to the angiosurgical operating room. Endovascular interventions are performed under multicomponent drug anesthesia in the department of X-ray surgical methods of diagnosis and treatment (complete head immobility during manipulations).
According to the European Stroke Organization Guidelines (2009)
Intravenous administration of rt-PA is recommended in the first 3 hours from the onset of the first signs of cerebral infarction at a rate of 0.9 mg/kg administered as a 10% bolus followed by infusion over 60 minutes. IV TLT has also been shown to be successful when administered between 3-4.5 hours after the first symptoms of stroke appear.
Before TLT, it is recommended to correct blood pressure if it increases to 185/100 mmHg or higher.
IA TLT is recommended as an additional treatment for acute MCA occlusion within a 6-hour “therapeutic window.”
IA TLT is performed for acute basilar occlusion in selected patients. IV TLT in case of basilar artery occlusion is a valid alternative even after 3 hours.
IV TLT for ischemic stroke should be carried out in an intensive care ward (unit) of a multidisciplinary hospital with the mandatory availability of round-the-clock neuroimaging services and clinical laboratory diagnostics. Potential risks and benefits should be discussed with the patient and family.
When deciding to conduct TLT, it is necessary to monitor blood pressure, heart rate, respiratory rate, body temperature, oxygen saturation, and control of biochemical blood parameters for at least 48 hours. Blood pressure levels and biochemical blood parameters cannot be an absolute obstacle to TLT; provided they are corrected during the permissible “therapeutic window,” thrombolysis is possible.
As a thrombolytic, today (based on evidence) it is possible to use a single drug: recombinant tissue plasminogen activator (rt-PA) - ALTEPLASE, ACTILYSE.
Based on the results of an analysis of foreign experience (more than 10 years of use of IV rt-PA, for example, 10 years ago in a regular vascular center in Germany or Spain an average of 15 TLTs were performed per year, now - 70-80) it became obvious that using a “one size fits all” approach is ineffective. The use of IV TLT is not successful in all cases of acute stroke, since not all strokes are the same. For small lesions, TLT is not justified economically, because A small stroke recovers well with conventional treatment. On the other hand, large strokes caused by occlusion of medium and large vessels are a difficult aspect of intravenous thrombolysis, in which the rate of achieving a therapeutic effect is low. In case of tandem occlusions of the ICA and MCA, the use of IV TLT is usually ineffective. However, the use of IV TLT remains the standard treatment for all patients with large artery occlusion when there are no contraindications.
Acute MCA occlusion is the most common type of occlusion in stroke patients and is often caused by cardiogenic embolism or large artery disease. The natural course of the disease in untreated acute occlusion of the MCA has an unfavorable prognosis, including such outcomes as persistent disability (more than 70%) and death (20%). It has been established that IV TLT is effective only in 1/3 of cases when complete recovery occurs. However, it is not just recanalization that is important. Only timely, rapid recanalization achieved within the “therapeutic window” is effective, i.e. before the development of irreversible changes in the brain. Late recanalization, not accompanied by clinically significant improvement, is ineffective. However, it is better than no therapy.