Facial nerve neuropathy is the most acute form of mononeuropathy and is a disease of the nervous system in which, due to the influence of certain factors, damage to the seventh cranial nerve occurs. This nerve controls the movement of the facial muscles and any damage to the nerve results in loss of movement of the facial muscles on the affected side. Damage to the nerve can also affect hearing and taste, since this nerve is also involved in the functioning of the senses. The effectiveness of treatment depends on the severity and cause of the disease.
Causes
There are many reasons, it is often impossible to clearly differentiate a specific factor, which is when we talk about idiopathic Bell's palsy. Often the cause is an infectious-allergic lesion. It develops in the second or third week after an acute viral infection. Hypothermia may also be an additional cause. Neuritis often develops as a result of traumatic lesions, sometimes during plastic surgery, surgery on the salivary glands, and surgery for sinusitis. In this case there is a clear connection with trauma; Treatment usually does not give good results.
Why does nerve damage occur?
The primary manifestation of the disease is usually associated with a recent viral infection or a previous cold. The recurrent course of the disease is caused by various factors, such as:
- multiple sclerosis;
- injuries of various origins;
- cerebral aneurysm;
- tumor processes;
- parotitis;
- diabetes;
- acute otitis;
- Hunt's syndrome (damage to nerve fibers by herpesvirus);
- ischemia, or local disturbance of blood supply;
- suffered stress;
- pregnancy.
The cause of the pathological process can also be a rare neurological disorder - Melkerson-Rosenthal syndrome, which is presumably inherited.
Symptoms
The symptoms are quite numerous. Depending on the degree of damage, localization of the main lesion, phase of the disease:
- Weakness of the facial and chewing muscles on one side, manifested in facial asymmetry and sagging cheeks.
- Leakage of food from the mouth.
- Lagophthalmos is the inability to completely close the eye, leaving a small strip of white.
- Impaired sensitivity of the tongue.
- Watery eyes or, conversely, dry eyes.
- Numbness of the cheek, soft palate and tongue.
- Impaired facial skin sensitivity.
- Pain in the parotid region is especially common with infectious-allergic lesions.
Long-term untreated neuritis can lead to persistent pathological manifestations. The clinic in this case will be as follows:
- Persistent paresis of the facial muscles.
- Facial sensitivity disorders.
- Pathological twitching - synkinesis - in the cheek, eyebrows, etc. Often accompanied by severe unpleasant or even painful sensations.
What are the possible complications?
A consequence of facial nerve neuropathy can be contracture, or contraction of the facial muscles, which is associated with their incomplete recovery. The patient complains of spasms and involuntary twitching on the affected side, facial asymmetry remains significantly pronounced. The following factors indicate an unfavorable prognosis:
- the duration of the disease is more than 3 weeks;
- age from 60 years;
- diabetes mellitus;
- complete paralysis of facial muscles;
- detection of severe degeneration of the facial nerve.
The prognosis is considered favorable for most patients, with complete recovery occurring in approximately 75% of cases.
Diagnostics
Diagnosis is usually not difficult for neurologists. The diagnosis is established based on medical history and neurological manifestations. In case of an old process, it makes sense to conduct ENMG of the facial nerve, which reveals a decrease in the excitability of nerve fibers and a decrease in the speed of impulse conduction.
Information about the disease
The facial nerve is responsible for ensuring the movements of facial muscles, the lacrimal gland, the tensor tympani muscle, and also innervates the anterior two-thirds of the tongue. It leaves the skull in a narrow canal located deep in the temporal bone. The slightest swelling in this area leads to compression of the fibers and the development of corresponding symptoms.
The pathology most often occurs in middle-aged people, who often neglect preventive measures due to the high pace of life. The peak incidence occurs in the cold season, since low temperatures are one of the provoking factors.
Make an appointment
Treatment
Treatment of neuritis of the facial nerve, especially with acutely developed manifestations, should begin immediately. Therapy includes drug treatment, physiotherapy techniques, exercise therapy, taping therapy (adhesive plaster traction).
- Drug treatment necessarily includes the prescription of neuroprotective drugs (primarily B vitamins), vascular therapy (Trental as the drug of choice), antioxidant treatment (Mexidol, vitamin E can be used), and hormonal treatment. Prednisolone for neuritis of the facial nerve is prescribed in the case of an infectious-allergic nature of the lesion and only in case of early treatment by the patient (on the first to fourth day after the onset of the disease). The hormone is prescribed in a decreasing pattern. Typically, on the first day, 50-70 mg is prescribed (10-14 tablets, in two or three doses), the dose is accumulated for the first three days, then there is a gradual (5 mg per day) reduction in the dosage until it is completely discontinued.
- Various techniques are used in physiotherapy. Electrophoresis with proserine and magnetic fields are often used. Prescription of procedures occurs only after consultation with a physiotherapist, identification of contraindications and the best method of treatment. In the recovery phase, as well as in case of long-term consequences, massage can be prescribed. Facial massage is done very carefully, using an activating technique on the affected side. Massage is an excellent procedure for preventing the development of synkinesis.
- The exercise therapy complex consists of exercises that allow for early muscle activation. When performing exercises, the healthy side is usually supported by the hand. This is necessary so that further redistribution of tone in favor of healthy muscles is not aggravated.
- Taping therapy involves applying adhesive tape to the weak muscles of the affected area. Sometimes it is during taping therapy that it is advisable to engage in physical therapy exercises. Depending on the number of muscles affected, a different number of adhesive tapes are applied. The time for one procedure is 1-2 hours.
Clinical picture
The symptoms are so characteristic that in a typical case the diagnosis is not difficult. The disease begins acutely, most often with pain behind the ear. Gradually the pain spreads across the face and to the back of the head. On the affected side, tears begin to flow from the eye, but sometimes dryness appears. Some patients notice that ordinary sounds have become extremely unpleasant. Over the course of 1-2 days, the symptoms increase, and paresis (weakness) or paralysis of the facial muscles occurs.
Manifestations of damage are:
- on the affected side of the face all skin folds are smoothed, this is especially visible on the nasolabial fold;
- when pronouncing consonants or at the moment of exhalation, swelling of the cheek is visible (symptom of “sail”);
- when you try to close your eyes, the eyelid on the affected side does not close, and the eyeball itself turns outward and upward - this characteristic symptom is called “hare’s eye” or lagophthalmos;
- When eating, solid food is between the gum and cheek, and liquid flows out of the corner of the mouth.
Intercostal neuralgia
Intercostal neuralgia is compression or irritation of the intercostal nerves. The disease is also called thoracalgia.
Intercostal neuralgia causes severe pain in the chest. Most often it occurs in middle-aged and elderly people.
How does intercostal neuralgia occur?
There are 12 pairs of ribs in the human skeleton. There is a nerve in each intercostal space. Because of their location, they are called intercostal nerves. When they are irritated or pinched, thoracic neuralgia occurs.
Most often, the disease appears after an acute muscle spasm. It occurs when a person turns poorly, sleeps in an uncomfortable position, stays in a draft for a long time or in the same position, or physically overexerts himself.
Causes of intercostal neuralgia
The disease is caused by the following reasons:
- Osteochondrosis, intervertebral hernia in the thoracic region;
- Rachiocampsis
- Diseases of the nervous system: multiple sclerosis, polyradiculoneuritis
- Infections: flu, tuberculosis, herpes
- Cardiovascular diseases: hypertension, atherosclerosis, anemia
- Inflammation in joints and ligaments, salt deposition in the spine
- Diabetes
- Vertebral compression fracture as a result of trauma, metastases, osteoporosis
- Lung diseases
Symptoms of intercostal neuralgia
- Severe burning pain throughout the chest or one side
- Painful sensations intensify with movement, coughing, changing body position, taking a deep breath
- Pain can radiate to the heart, shoulder blade, neck, arm, lower back
- Attacks of neuralgia may be accompanied by sweating, redness of the skin or muscle twitching
- Loss of sensitivity, goosebumps, numbness of the skin over the affected nerve
- Burning, tingling in the affected area
Signs of the disease in women more often appear in the heart area. In men, the pain is localized on the lower ribs on the left side.
Treatment
Drug treatment
The first step is pain management.
This is done with the help of non-steroidal anti-inflammatory drugs, muscle relaxants, and steroidal anti-inflammatory drugs in the form of therapeutic drug blockades.
Physiotherapeutic treatment
Magnetic therapy and laser therapy are used in the ELIGOMED digital computer to relieve the inflammatory process and relieve pain.
Acupuncture
An effective method of pain relief and muscle relaxation.
The ELIGOMED CVM uses its own reflexology techniques, developed and patented, which have been proving their effectiveness for over 20 years.
Facial nerve neuropathy: modern approaches to diagnosis and treatment
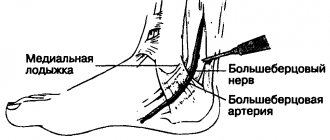
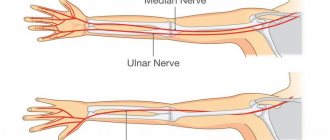
Facial nerve neuropathy is an extremely relevant pathology of the peripheral nervous system today. The number of people suffering from this disease is constantly growing. The frequency of facial nerve neuropathies is, for example, in European countries 20 cases, in Japan 30 cases per 100 thousand population. According to WHO, the most common type is mononeuropathy of the facial nerve, which ranks 2nd in frequency among diseases of the peripheral nervous system. The incidence ranges from 8 to 240 cases per 100 thousand population in different countries of the world [1, 2]. The relatively high incidence of damage to the facial nerve is due to its topographic and anatomical features [1, 3]. The facial nerve unites two nerves: the facial nerve itself, formed by motor nerve fibers, and the intermediate nerve, which is sensitive taste and autonomic (parasympathetic) nerve fibers. In the fallopian canal of the temporal bone, three branches arise from the facial nerve: the greater petrosal nerve, the chorda tympani, and the stapedius nerve. After leaving the stylomastoid foramen, many motor branches depart from the facial nerve to the facial muscles. The intermediate nerve contains afferent fibers (taste sensitivity) going to its sensory nucleus, and efferent fibers (secretory, parasympathetic) coming from its autonomic nucleus [4, 5]. According to I.Ya. Sendulsky distinguishes between the labyrinthine (intracrural), tympanic (intratympanic), tympanomastoid (intermediate) and mastoid sections of the bony canal of the facial nerve. The labyrinthine section, 3 mm long, runs from the internal auditory opening to the geniculate canal of the facial nerve. It begins in the medial part of the superior fossa of the bottom of the internal auditory canal, then goes under the anterosuperior surface of the pyramid. Here the canal passes between the transition point of the main curl of the cochlea into the second and the ampulla of the superior semicircular canal. This part of the channel has a horizontal direction, perpendicular to the axis of the pyramid. The intrarocky part of the canal is located near the labyrinth, which creates the danger of nerve damage in labyrinthine pathologies. The tympanic section occupies the space from the knee of the facial nerve canal to the pyramidal protrusion. Its length is 8–11 mm. It does not run parallel to the axis of the pyramid, but goes from the front and top - back and down. Its beginning is covered by a spoon-shaped process. The main part of this section passes between the eminence of the external semicircular canal and the oval window. At this point, the horizontal part of the facial nerve canal passes at an angle (second knee) into the descending part (according to Schwartz). Passing from the labyrinthine wall of the tympanic cavity to its posterior wall, the facial nerve canal forms the inferomedial side of the aditus (threshold). Trauma to the facial nerve during radical ear surgery, during removal of granulations of the tympanic cavity, usually occurs in this place. The tympanomastoid section is part of the facial nerve canal, located in the posterior wall of the tympanic cavity within the pyramidal eminence. This part of the canal is closely connected with both the tympanic cavity and the mastoid process. On the back wall the canal is covered with a pyramidal elevation. The mastoid portion of the facial nerve canal occupies the space from the pyramidal protuberance to the stylomastoid foramen. Its length is about 12.0–13.5 mm. This section corresponds to the descending part of the facial nerve canal according to Schwartz. There are 3 types of channel passage: 1st type - normal vertical, 2nd type - flat, 3rd - medium oblique. The steeper the facial nerve canal descends, the deeper it lies in the bone, and vice versa. The facial nerve canal may be 1–10 mm distant from the posterior wall of the bony external auditory canal. But still, in the majority of cases, the direction of the canal is vertical and the distance from it to the posterior wall of the external auditory canal, as a rule, does not exceed 2–4 mm. The distal mastoid portion of the facial nerve canal is at risk of injury during resection of the mastoid apex and surgery on the jugular bulb [4, 6]. Anomalies in the position of the facial nerve canal are rare, but have very important surgical significance. Kettel, using material from 125 operations on the facial nerve, described three variants of deviations of the facial nerve from its normal location. The blood supply to the facial nerve is carried out by the stylomastoid artery passing through the fallopian canal. Poor circulation plays a major role in nerve pathology [6]. There are many causes of facial nerve damage. The first place among them is occupied by the inflammatory factor: neuritis, otogenic damage. The second place is occupied by iatrogenic causes, which is due, on the one hand, to the complexity of the topographic anatomy of the facial nerve, on the other hand, to the need for frequent interventions, and the peculiarity of the growth of tumors of the ear and base of the skull. The incidence of facial nerve damage during otological operations ranges from 0.2 to 10%. In some cases, its function is persistently impaired after surgery, despite the preservation of anatomical integrity. The presence of facial muscle paresis before surgery, as well as tumor sizes greater than 3 cm, are poor prognostic signs regarding the preservation of facial nerve function. The use of microsurgical techniques to remove tumors of the cerebellopontine angle currently allows the majority of patients to preserve the anatomical integrity of the facial nerve, but its function is preserved or restored only in no more than 50% of patients. The facial nerve is also often damaged during surgical interventions on the neck, maxillofacial operations and during operations on the parotid salivary gland, since it is located in the thickness of its tissue, where it forms the so-called parotid plexus [7]. Post-traumatic injuries of the facial nerve take 3rd place. Facial nerve injury occurs in approximately 15% of patients with traumatic brain injury and basal skull fracture. Traumatic injuries to the facial nerve account for 5–7% of all its lesions. Transverse fractures of the temporal bone pyramid are complicated by damage to the facial nerve in 30–50% of cases, longitudinal fractures in 10–25%, but 70–90% of facial nerve paresis recover on their own. The facial nerve can also be damaged by wounds and closed injuries to the face and neck. The frequency of injuries to the maxillofacial area among head injuries is 16.5%. Considering the high level of general traumatism and its tendency to increase, the problem of traumatic injuries of the facial nerve is undoubtedly relevant and socially significant [8]. Of all lesions of the facial nerve, 6.5% are based on single causes, among them rare infectious diseases, diseases of the central nervous system, and metastatic lesions [6, 8]. It should be noted that there are several anatomical prerequisites for such frequent damage to the facial nerve: phylogenetically, the nerve is one of the youngest cranial nerves, has a long and tortuous course in a narrow bone canal, a feature of the blood supply to the nerve is that the main vessels in a narrow bone bed behave similarly to the terminal ones [2, 7]. So, etiologically, the following types of lesions of the facial nerve can be distinguished: - idiopathic neuropathy, or Bell's palsy (the most common form - up to 75% of cases), when the exact etiological causes cannot be established. This form is characterized by seasonality, the development of the disease after cooling and during common colds; – otogenic neuritis (up to 15% of cases), in which the trunk of the facial nerve is often damaged during operations on the middle ear (general cavity operations, operations on the mastoid process for purulent mastoiditis); – infectious neuritis, which occurs much less frequently: with Herpes zoster (Hunt syndrome), polio, influenza, mumps, etc. Considering the large number of lesions of the facial nerve of otogenic origin, this problem should be considered relevant not only for neurologists, but also for otolaryngologists. Knowledge of the anatomy, topography and blood supply of the facial nerve helps in correct topical diagnosis and in prescribing correct and timely treatment, which helps reduce the number of complications. To assess the degree of damage to the facial nerve, the House–Braakman scale is used (Table 1).
Paralysis of the facial muscles leads not only to cosmetic defects and painful experiences for the patient, but also to impaired swallowing and chewing functions, as well as to phonation. Neuroparalytic keratitis, which is caused by lagophthalmos and impaired tear production in patients with damage to the facial nerve, leads to scarring of the cornea, reduction and loss of vision. Thus, damage to the facial nerve significantly reduces the quality of life of patients. Topical diagnosis of nerve lesions at different levels is based on the identification of peripheral paralysis and other symptoms. When the nucleus of the facial nerve is damaged, peripheral paralysis of the facial muscles on the side of the lesion can be combined with spastic hemiparesis on the opposite side. If the pathological focus spreads to the inner knee of the facial nerve, then the function of the nucleus of the abducens nerve is also disrupted. In this case, alternating Foville syndrome develops: on the side of the lesion there is peripheral paralysis of the facial muscles and the external rectus muscle of the eye, and on the opposite side there is spastic hemiplegia. When the root of the facial nerve in the cerebellopontine triangle is damaged, paralysis of the facial muscles is accompanied by symptoms of dysfunction of the trigeminal, abducens and vestibulocochlear nerves. When the facial nerve is damaged in the internal auditory canal, paralysis of the facial muscles is combined with a taste disturbance in the anterior two-thirds of the tongue, dry eyes and deafness in this ear. Damage to the facial nerve in the bony canal before the origin of the greater petrosal nerve is manifested by prosoplegia, taste disturbance in the anterior two-thirds of the tongue, dry eye and hyperacusis. Damage to the facial nerve in the facial canal above the level of the origin of the stapedius muscle is accompanied by lacrimation, hyperacusis and taste disturbance. When the facial nerve is damaged at the level of exit through the stylomastoid foramen, the clinical picture consists only of paralysis of the facial muscles and lacrimation. In some cases, the pathological process extends not only to the facial nerve, but also to the branches of the trigeminal nerve. In such cases, peripheral paralysis of the facial muscles is accompanied by excruciating pain in the lateral area of the face. When the corticonuclear fibers are damaged on one side, paralysis of only the lower facial muscles on the opposite side develops [3, 7]. When treating facial nerve injuries, it is advisable to consider both surgical and conservative approaches. In the treatment of persistent dysfunction of the facial nerve, surgical methods are most effective [1, 7]. Surgical aids for neuropathies of the facial nerve can be divided into two groups: interventions on the facial nerve in order to restore its conductivity and voluntary motor function of the facial muscles, plastic surgery (static and dynamic) on the skin, muscles and tendons of the face in order to reduce cosmetic defects and replace function paralyzed muscles [1, 9]. The facial nerve is the first nerve on which neuroplasty was performed, which consists of suturing the peripheral segment of the facial nerve with the central segment of another, specially transected motor nerve. For the first time, reinnervation of the facial nerve by the accessory nerve was performed by Drobnik in 1879, and by the hypoglossal nerve by Korte in 1902. Soon these operations began to be used more often. In addition to the accessory and hypoglossal nerves, the glossopharyngeal nerve, phrenic nerve, and descending branch of the hypoglossal nerve were used as donor nerves for reinnervation of the facial nerve; 2nd and 3rd cervical nerves, the muscular branch of the accessory nerve to the sternocleidomastoid muscle. To date, considerable experience has been accumulated in operations of extracranial reinnervation of the facial nerve. Reinnervation of the facial nerve by the accessory nerve.
The main effect of the operation is to prevent muscle atrophy and restore their tone.
Hypoglossal nerve reinnervation of the facial nerve is the most commonly used technique for extracranial facial nerve reinnervation. Many authors, preferring this technique, emphasize that there are functional relationships between the motor areas of the face and tongue in the central nervous system [1, 6, 9]. Cross-face anastomose
, cross-face nerve grafting
was first described in the works of L. Scaramella (1971), JW Smith (1971), H. Andrel (1972). The essence of the operation is the reinnervation of the affected facial nerve or its branches with individual branches of the healthy facial nerve through autografts, which makes it possible to create connections between the corresponding branches of the facial nerves. Typically, 3 autografts are used (for the muscles of the eye, cheek and mouth circumference). The operation can be performed in 1 or 2 stages, as early as possible, and surgical technique is of great importance for a positive outcome. To improve results, facial plastic surgery is also used, which can be divided into static and dynamic. The purpose of static operations is to reduce facial asymmetry; for this purpose, tarsorrhaphy is performed to reduce lagophthalmos, and tightening of the facial skin [1, 9]. Multidirectional suspension techniques have been proposed to correct brow drooping, lagophthalmos, and cheek and corner of the mouth drooping. For this purpose, fascial tapes cut from the fascia lata of the thigh are used. There are even cases of implantation of a metal spring into the upper eyelid. However, as the authors themselves note, in such cases a rejection reaction is possible. If there is no good fixation, the spring can be pushed out, even perforating the skin. A similar complication occurs when magnets are implanted into the eyelids (rejection reaction in 15% of cases) [1, 6]. The goal of dynamic surgery
is to replace the function of paralyzed muscles.
In 1971, a free muscle-tendon autograft was transplanted for the first time. Transplantation of free muscle-tendon autografts has been performed by many surgeons. The authors note that transplanted muscles often undergo cicatricial degeneration. With the development of microsurgical technology, muscle transplantation with microvascular and neural anastomosis and the transfer of muscle flaps from the temporal or subcutaneous muscles of the neck began to be used more widely [6, 7]. Contraindications to plastic surgery are the presence of purulent inflammatory foci on the scalp, neck, ear, tonsils and paranasal cavities; inflammatory processes of the parotid and submandibular glands, lymph nodes and neck area, mastoid process. Plastic surgery should not be performed when initial signs of restoration of facial nerve function appear [7]. In addition to surgical treatment methods, conservative therapy, including drug therapy and physiotherapeutic methods, is of great importance. Exercise therapy during surgical treatment of facial nerve injuries can be divided into 3 periods: preoperative, early postoperative, late postoperative [10]. In the preoperative period, the main task is to actively prevent asymmetry of the healthy and diseased sides of the face. The sharp asymmetry of the face that was created on the first day after the main operation requires immediate and strictly targeted correction. Such a correction is achieved by two methodological techniques: the desired position is given using adhesive tape tension and special gymnastics for the muscles of the healthy half of the face. Treatment by tension.
Adhesive plaster tension is carried out as follows: the adhesive plaster is applied to the active points of the healthy side of the face - the area of the quadratus muscle of the upper lip, the orbicularis oris muscle (on the healthy side) - and with a sufficiently strong tension directed towards the sore side, it is attached to a special helmet-mask or to side straps of the postoperative dressing. The tension is left for a period of 2 to 6 hours a day with a gradual increase in time from day to day. Such a bandage is especially necessary during active facial actions - while eating, talking, in emotional situations, since weakening the asymmetric traction of the muscles of the healthy side of the face improves the general functional state of the paralyzed muscles, which plays a huge role in the postoperative period, especially after germination of the stitched nerve. Treatment with tension in the area of the orbicularis oculi muscle on the affected side is considered separately. In this case, an adhesive plaster is applied like a “crow’s foot” to the middle of the upper and lower eyelids and pulled outward and slightly upward. At the same time, the palpebral fissure narrows significantly, which ensures almost complete closure of the upper and lower eyelids when blinking, normalizes tear production, and protects the cornea from drying out and ulceration. During sleep, the main adhesive plaster tension is removed and left in the eye area. Special gymnastics in this period is also mainly aimed at working the muscles of the healthy side - training is carried out on active muscle relaxation, dosed and, of course, differentiated tension of the main facial muscle groups - the zygomatic, orbicularis oris and eye muscles, triangular muscles. Such exercises with the muscles of the healthy half of the face reduce facial asymmetry, prepare these muscles for such a dosed tension, which in the future will be the most adequate, functionally beneficial for slowly recovering paretic muscles. The second period, early postoperative, is from the moment of plastic surgery to the first signs of nerve sprouting. At this time, basically the same rehabilitation measures continue as in the first period: tension treatment and special gymnastics, aimed primarily at dosed training of the muscles of the healthy side of the face. A necessary addition to these exercises are reflex exercises - static tension of the tongue muscles and forced swallowing training. Tension of the tongue is achieved as follows: the patient rests the tip of the tongue against the line of closed teeth for 2-3 seconds, then relaxes the tongue muscle and again rests against the gum - now above the teeth. After relaxation, emphasis should be placed on the gums below the teeth. Similar series of tensions (emphasis in the middle, up, down) are done 3-4 times a day, 5-8 times during each series. Swallowing training is also carried out in series of 3-4 sips in a row. You can combine normal swallowing with drinking fluids, especially if the patient experiences dry mouth. Combined movements are also possible - static tension of the tongue and, at the same time, swallowing. Combined exercises require a longer rest (3–4 minutes) than after individual exercises. During this period, various types of restorative treatment can be recommended: vitamin therapy, massage of the collar area, etc. Massage of the face, especially the affected side, is considered inappropriate during this period. The third, late postoperative period begins from the moment of the first clinical manifestations of nerve sprouting. Movements of the laughter muscles and one of the portions of the zygomatic muscle appear earlier than others. During this period, the main emphasis is on therapeutic exercises. Static exercises for the muscles of the tongue and swallowing movements continue with a significant increase in the number of classes to 5-6 times a day and the duration of these classes. Before and after exercises, it is recommended to massage the affected half of the face. Particularly valuable is massage from the inside of the mouth, when a physiotherapy instructor massages individual muscle groups with a hand in a surgical glove - the quadratus muscle of the upper lip, the zygomatic muscle, the orbicularis oris muscle, the buccal muscle. As the amplitude of voluntary movements increases, exercises are added with symmetrical tension on both sides - healthy and affected. Here, an important methodological principle is to equate the strength and amplitude of contraction of the muscles of the healthy side with the currently limited capabilities of the muscles of the affected side, but not vice versa, since paretic muscles, even with maximum contraction, do not reach the capabilities of healthy muscles - compliance with this rule ensures facial symmetry. Only equating healthy muscles with paretic ones eliminates asymmetry and thus increases the overall effect of surgical treatment. Movements of the orbicularis oculi muscle appear much later and are initially the result of synergy of contractions of the muscles of the lower and middle parts of the face. This synergy will be achieved within 2–3 months. should be strengthened in every possible way (by joint contractions of all muscles of the affected side), and after achieving a sufficient amplitude of contraction of the orbicularis oculi muscle, it is necessary to achieve differentiated contractions of all muscles. With proper sequential training, the skill of separate contraction of the muscles of the healthy side (see the first period) should transfer to the affected side. During the same period, it is recommended to carry out tension treatment according to the method outlined above, reducing the time to 2–3 hours, every other day [1, 5, 6]. Drug therapy methods include: analgesics, decongestants, anti-inflammatory drugs, vitamins, antiplatelet agents [10]. Neurobion contains a combination of B vitamins: pyridoxine (B6), thiamine (B1) and cyanocobalamin (B12). These vitamins act as coenzymes in intermediate metabolism in the central and peripheral nervous system. It should be noted that the combined use of vitamins B1, B6 and B12 is advisable due to their special role in the metabolic processes of the nervous system [11–13]. This combination of coenzymes accelerates the regeneration of damaged nerve fibers, since it has been proven that the effectiveness of the combination of drugs is superior to the effectiveness of individual components. The therapeutic use of B vitamins is aimed, on the one hand, at compensating for existing deficiency, and on the other hand, at stimulating natural mechanisms for restoring the function of nerve tissue. The analgesic effect of the B vitamin complex has also been proven, which has a beneficial effect on the quality of life of patients [14, 15]. The main indication for use of the drug Neurobion is neuropathy of the facial nerve. Contraindications include hypersensitivity to the components of the drug, childhood, pregnancy and breastfeeding [11]. Among the side effects of the drug Neurobion, in some cases with parenteral administration of vitamin B1, sweating, tachycardia and allergic reactions in the form of skin itching and rash were noted. In rare cases, a hypersensitivity reaction may occur - exanthema, difficulty breathing, anaphylactic shock (after parenteral administration of vitamin B1), acne, eczema and urticaria were observed with the administration of vitamin B12 (mainly through intravenous infusions). When used simultaneously with levodopa, vitamin B6 reduces the antiparkinsonian effect of levodopa. An increased need for vitamin B6 may occur with simultaneous administration of D-penicillamine and cycloserine. Vitamin B1 is destroyed when interacting with solutions containing sulfites [11, 14, 16]. Vitamins B1, B6 and B12 have a wide therapeutic range. Overdose symptoms are not observed when the drug is used in recommended doses and regimen. When high doses of vitamins are administered intravenously for a long time (>2 months), symptoms of intoxication may occur. Neurobion is available in solution for intramuscular administration and in tablet form. In cases of severe pain, it is recommended to begin treatment with intramuscular administration of 3 ml/day until acute symptoms subside. After the symptoms have weakened or in cases of moderate severity, switch to administration of 3 ml 2-3 times a week for 2-3 weeks. For maintenance therapy, to prevent relapse or continue the course of treatment, the drug Neurobion in tablet form is recommended. The drug Neurobion should be taken 1 tablet 3 times a day. The duration of treatment is determined by the doctor and averages 1–1.5 months. Currently, the results of a number of clinical studies of the drug Neurobion are known. A randomized, double-blind study, “Neurobion versus placebo in the prevention of relapse of spinal pain syndrome with B vitamins,” conducted by G. Schwieger, showed a lower rate of relapse of neuropathy - 32% - compared to the placebo group, where the relapse rate reached 60% [11 , 16]. Thus, treatment of diseases of the facial nerve should be comprehensive and include both surgical and medicinal methods. Moreover, systemic drug therapy should occupy a leading place, prescribed individually and depending on the phase of rehabilitation and the concomitant use of surgical aids or physiotherapeutic techniques.