general description
Bernhardt-Roth disease (neuropathy of the external cutaneous nerve of the thigh) (G57.1) is damage to the external cutaneous nerve of the thigh due to compression of its fibers under the inguinal ligament in the region of the anterosuperior iliac spine, manifested by paresthesia, pain in the area of the outer surface of the thigh.
The syndrome is more often observed in men 50–60 years old (75%).
Possible causes of the disease: abdominal obesity, use of a corset, tight belt, pregnancy.
Causes
A common cause of the development of Roth's disease is the anatomical features of the human body. Another common cause of Roth's disease is obesity, especially in the abdomen and thighs.
In men, this pathology can be aggravated by wearing a tight trouser belt. The belt puts pressure on the fatty belly area and thereby compresses the nerve. In women, the cause may be constant wearing of corsets.
The most serious reason for the development of pathology is the presence of a large tumor or hematoma in the abdominal area.
There is also "temporary" meralgia. This form occurs in pregnant women. It occurs as a result of tension in the inguinal ligament, which compresses the nerve.
The most rare causes include diabetes mellitus, malaria, herpes zoster, and typhoid fever.
Clinical picture
The disease develops gradually. The lesion is characteristically unilateral. Feelings of numbness, tingling, and burning occur first in certain areas of the thigh. Over time they become permanent. The pain appears over several months.
An objective examination of the patient reveals hypoesthesia/analgesia along the anterior outer surface of the thigh (up to 100%). In 80% of cases, pain is noted on palpation and percussion in the area of the nerve trunk, pain increases with hip hyperextension, and decreases with flexion of the hip joint. The painful point is at the level of the notch under the anterior superior iliac spine.
Treatment
Treatment for Roth's disease depends on the severity and duration of the disease. Treatment includes a set of measures.
The conservative method is aimed at alleviating the patient’s condition (pain relief) and eliminating the cause of nerve compression. Pain syndrome is eliminated by non-steroidal anti-inflammatory drugs, such as Ketorol, Diclofenac. If their use is ineffective, anticonvulsants are prescribed.
For obesity, a diet aimed at losing weight, as well as physical exercise, is recommended. Decongestant therapy with diuretics (Furosemide, Lasix) is also carried out.
Vascular medications are prescribed to improve microcirculation and nutrition in the affected area. Anticholinesterase drugs are indicated to restore nerve impulse transmission.
Physiotherapy has proven itself well in the treatment of Roth's disease: shock wave therapy, electrophoresis, acupuncture.
If all of the above treatment methods are ineffective and in severe cases, surgical treatment may be indicated. Surgery is aimed at freeing the damaged nerve and preventing further compression.
Shock wave therapy treatment
Shock wave therapy is a method of treating musculoskeletal diseases using the properties of sound. This method of physiotherapy is relatively new, but is already showing good results. Shock wave therapy acts as an auxiliary drug treatment, as well as in the postoperative period.
A person cannot hear these shock waves, because their frequency is quite low (16-25 Hertz). They are characterized by short pulse duration and high pressure amplitude. The effect of this treatment method is based on the difference between the acoustic impedance of soft and dense tissues. Sound waves easily penetrate the skin, fat layer and blood vessels. But bones, muscles and tendons are an obstacle for them, due to this an effect similar to a massage occurs. What happens in these places:
- strengthening and improving blood circulation;
- reduction of excessive muscle tone;
- anesthesia;
- destruction of pathological formations (growths on bones, calcified deposits, etc.).
Physiotherapists use various sources of sound waves:
- Pneumatic.
- Electromagnetic.
- Electrohydraulic.
- Piezoelectric.
The effectiveness of shock wave therapy for Roth's disease:
- Tissue swelling is reduced.
- Blood circulation in the affected area improves.
- Pain is reduced.
- Feeling better after exercise.
- Unpleasant sensations in the affected area (tingling, burning, numbness) are reduced.
- Rehabilitation after treatment is accelerated.
Improvement is often felt after the first or second session.
Benefits of shock wave therapy treatment:
- Gentle effect on the body.
- A small number of contraindications.
- High efficiency of treatment.
- Sometimes acts as an alternative to surgery.
- Combines with other treatment methods.
- Non-invasive procedure and ease of use.
The course of treatment usually ranges from 5 to 10 procedures. Intervals between procedures can range from 3 to 5 days. Many patients return to work after a course of treatment in a short time.
Contraindications to this method of physiotherapy:
- Pregnancy.
- Malignant formations.
- Systemic blood diseases and thrombophlebitis.
- Acute inflammatory processes, infections.
- Presence of a pacemaker.
Treatment of Bernhardt-Roth disease
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist. Vitamin therapy, analgesics, massage, physiotherapy, therapeutic physical training, novocaine and hydrocortisone blockades, and surgery in the inguinal ligament are indicated. Measures such as normalizing body weight, eliminating external pressure factors and treating somatic diseases are important.
Essential drugs
There are contraindications. Specialist consultation is required.
- Voltaren (non-steroidal anti-inflammatory drug). Dosage regimen: IM at a dose of 75 mg (contents of 1 ampoule) 1 time/day.
- Ketoprofen (non-steroidal anti-inflammatory drug). Dosage regimen: IM - 100 mg 1-2 times a day; after pain relief, it is prescribed orally in a daily dose of 300 mg in 2-3 doses, a maintenance dose of 150-200 mg/day.
- Tramadol (analgesic). Dosage regimen: IV, IM, SC in a single dose of 50-100 mg, possible repeated administration of the drug after 4-6 hours. The maximum daily dose is 400 mg.
- Thiamine bromide (vitamin B1). Dosage regimen: IM, 2 ml of 6% solution 1 time/day. There are 25 injections per course.
- Cyanocobalamin (vitamin B12). Dosage regimen: IM, 200 mcg 1 time/day. There are 20 injections per course.
Causes of Roth-Bernhardt syndrome and methods of its treatment
Roth Bernhardt's disease was first described by the Russian scientist Roth and the German Bernhardt at the end of the 19th century. Another name is myalgia paresthetica. The disease is a compression of the lateral nerve of the skin of the thigh. The external nerve is a conductor of impulses from the outer and posterior zones of the thigh, ending near the knee. The nerve may have anatomical pathology. The disease itself is caused by abnormal structural features of the hip; it can be unilateral and in 20% of cases bilateral.
Factors leading to illness
Factors influencing congenital disorders:
- Manifestation of the disease in the area of attachment of the inguinal ligament to the bone due to poor blood circulation.
- The appearance of a canal when the groin ligament bifurcates, where the nerve is pinched.
- Congenital sharp fracture of the nerve.
- Nerve close to the ilium, etc.
In addition to congenital, the disease can be acquired and manifests itself with age. This is facilitated by:
- Pressure on the lateral nerve caused by wearing tight clothing or a belt;
- Pregnancy, as the forward curve of the spine increases and the inguinal ligament becomes tense;
- Excess body weight, where the most problem areas are the stomach and thighs;
- Hernias in the groin;
- Neoplasms in the abdominal area;
- Pathological fluid in the abdominal cavity;
- Hematomas in the retroperitoneal region;
- Swelling and increased tissue size associated with surgical procedures or inflammation;
- Diabetes, lack of microelements, typhoid fever and other diseases in acute and chronic forms;
- Rachiocampsis
. _
Signs of Roth Bernhardt's disease
Signs of the disease become obvious from the first moments of compression of the external nerve. Patients complain of:
- Burning;
- Numbness;
- Decreased sensitivity;
- Cold;
- The appearance of ulcers;
- Acute painful sensations;
- Skin inflammation;
- Intermittent claudication that occurs with physical activity and disappears when the person is immobile.
Ways to determine the disease
It is not difficult to identify a disease, but you need to find its root cause, on which treatment will depend. First, data is collected about the patient’s well-being and his complaints, then a visual and palpation examination is carried out. In order to make an accurate diagnosis, the following methods are used:
- Electroneuromyography is used to assess muscle activity in response to a stimulus.
- Ultrasound helps determine the area where the nerve is torn and other abnormalities.
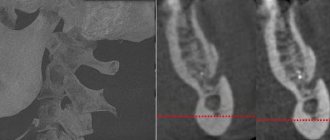
- MRI is prescribed to obtain a three-dimensional image of the area in any projection. Most often it is performed when there is a suspicion of the presence of neoplasms and internal hematomas.
- CT also provides reliable information, but with the use of X-rays.
- X-ray of the spine.
- Autoimmune and biochemical blood tests.
If, after eliminating the obvious cause of the disease, the patient continues to complain of malaise, additional examinations are prescribed.
How is Roth-Bernhardt disease treated?
To cure the disease, a set of therapeutic and preventive measures are used to improve well-being and eliminate pressure on the nerve.
Medicines are prescribed for:
- Relieving inflammation. For this, non-steroidal anti-inflammatory drugs like Diclofenac, Indomethacin, etc. are used.
- Pain relief in the form of ointments, tablets or injections.
- Improves blood circulation.
- Obtaining the necessary elements. For this purpose, vitamin complexes are prescribed, especially those containing B12 and B1 and the minerals Mg, Ka, Cal, necessary for the heart.
- Vasodilation using Nicotinic acid, Trental, etc.
- For severe acute pain, hormonal drugs such as Prednisolone, Dexamitozone, etc. are recommended.
Physiotherapeutic treatment is prescribed in the form of:
- Hydrogen sulfide baths;
- Wraps;
- Mud treatment;
- Water massage;
- Magnetic laser procedures;
- UHF;
- Acupuncture.
The measures taken inhibit the inflammatory process, relieve pain, and improve blood flow to tissues and cells.
Gymnastic exercises have a positive effect on recovery. The most productive block is carried out daily for 15 minutes, including the following exercises:
- The patient sits with his legs bent. Using sliding movements along the flooring, you need to straighten your lower limbs. Perform five times in two approaches.
- The patient's position is to lie on his stomach. The hands are placed on the lumbar region. Raises the shoulders along with the head, lifting them off the floor at a slow pace three times. Do it twice.
- The patient stands with his hands on his belt. Spreads his legs at a slow pace, sliding and leaving his feet on the floor. Performs four times, taking a 15-second pause between approaches.
- The patient lies on his stomach and performs arm movements six times as with the breaststroke technique.
- The patient lies on the side opposite the patient. The head is placed on the arm bent at the elbow. Raises the straight leg to a painless maximum about eight times.
During treatment, the patient is advised to:
- Refrain from uncomfortable clothes, replacing them with loose-fitting models, avoiding belts.
- Eat foods rich in microelements and vitamins, adhere to a proper sleep schedule.
- Monitor your weight, if it exceeds the norm, adjust your diet and increase physical activity.
For tumors and large-scale hematomas, operations to remove them are indicated, where a positive outcome predetermines the timely surgical manipulation.
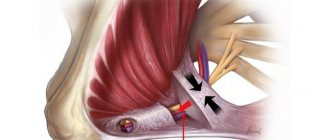
To reach the nerve, a shallow incision is made in the skin under local anesthesia. If the operation is delayed, the growing death of nerve cells will interfere with recovery. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 0 | 0 | 0 | 3 | 6 | 0 | 0 | 0 | 0 | 0 | 1 | 2.8 |
What causes upper extremity neuropathy to develop?
The main cause of upper extremity neuropathy is nerve compression. This can happen in places where the nerve lies shallow under the skin or passes through a narrow bone canal (for example, the ulnar canal); in some cases, the nerve can be compressed “in the depths” of the arm. The main causes of nerve compression are:
- An uncomfortable position in which the arm is in an inverted state for a long time (during sleep, while intoxicated or under anesthesia)
- Injuries to the extremities: both direct injury to the nerve (bruise, tear, rupture), and injury to bone or muscle tissue, in which the nerve is compressed by bone fragments or swelling, hematoma
- Consequences of injury or surgery: 1) the nerve can be involved in the forming scar tissue and become trapped in it; 2) lack of blood circulation and, as a consequence, deterioration of muscle nutrition; 3) compressive edema
- Deformation of joints due to professional activities (athletes, musicians, chefs, dentists, working with vibrating instruments)
- Cervical osteochondrosis
- Frequent hypothermia
- Any swelling and inflammation in the muscles caused by infection (flu, herpes, tuberculosis, diphtheria, malaria, HIV) or endocrine diseases (diabetes mellitus)
- Mechanical compression of the nerve by a tumor (in oncology and benign tumor diseases)
- Lack of vitamins (usually vitamin B) or minerals in the body
Symptoms of upper limb neuropathy
A nerve is a channel through which information about its (organ/limb) position in space, temperature, pressure, etc. is received from an organ to the brain, and action commands to the organ/limb are received from the brain. In case of nerve damage, this connection is disrupted or broken, i.e. the brain “does not know” about the existence of the limb, or incorrectly interprets the information (partially not reaching it), or the signal from the brain does not reach the limb. Therefore, with neuropathy of the upper extremities, the most common symptoms are:
- weakness of arm muscles, difficulty moving, difficulty raising arms up (especially from the sides)
- because of this, a lack of coordination of movements develops
- changes in the sensitivity of the hands: decreased temperature sensitivity, sensation of “pins and needles” (paresthesia)
- muscle atrophy of the upper limbs
- spastic syndrome: involuntary muscle contractions, cramps and spasms
- swelling of the limbs
Causes and types of neuropathy
In 30% of cases, neuropathy is considered idiopathic (that is, arising from unknown causes).
Otherwise, the causes of the disease can be divided into internal and external.
Causes associated with various internal pathologies:
- endocrine diseases, of which diabetes mellitus accounts for about a third of all neuropathies;
- vitamin deficiency, especially deficiency of B vitamins;
- autoimmune diseases;
- multiple sclerosis;
- rheumatoid arthritis, etc.
External factors that provoke the development of neuropathy include:
- alcoholism (a common consequence is neuropathy of the lower extremities);
- injuries;
- intoxication;
- infections.
Often the cause of nerve damage is a hereditary factor. In such cases, the disease can develop independently, without any additional harmful effects.
Neuropathy is a very serious illness that requires qualified diagnosis and adequate treatment. If you are concerned about any of the symptoms listed below, consult a neurologist immediately!
Depending on the location of the disease, neuropathies of the upper, lower extremities and cranial nerves are distinguished, for example:
Facial nerve neuropathy
It can develop as a result of a traumatic brain injury, a viral infection, hypothermia, unsuccessful dental surgery, depression, pregnancy and childbirth, as well as due to a neoplasm. Signs of the disease are: weakening of the muscles on the side of the affected nerve, salivation and lacrimation, inability to completely close the eyelids.
Trigeminal neuropathy
Caused by various reasons (maxillofacial surgery, dentures, difficult childbirth, heredity) damage to the nerve endings of the gums, upper and lower lips, and chin. Patients complain of severe facial pain from the affected nerve, radiating to the upper and lower jaws, not relieved by analgesics. There is also discharge from one nostril, lacrimation and redness of the eye.
Radial nerve neuropathy
It often occurs against the background of so-called “sleep paralysis,” i.e. compression of the nerve due to incorrect position of the hand. Occurs in people who use drugs or alcohol. It also progresses with wrist fractures, bursitis or arthritis. It manifests itself as a violation of the dorsiflexion of the hand (the hand hangs), numbness of the thumb and index fingers, pain can occur on the outer surface of the forearm.
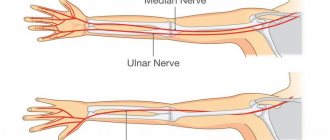
Median nerve neuropathy
Damage to this area of the upper limb can occur due to sprains, fractures, diabetes mellitus, rheumatism, gout, neoplasms, as well as in the event of nerve compression. It manifests itself as severe pain (as well as numbness and burning) in the forearm, shoulder, hand, thumb, index and middle fingers.
Ulnar nerve neuropathy
The cause of this disease may be traumatic (sprain, tear and rupture) or other damage to the ulnar nerve (for example, caused by bursitis, arthritis). It manifests itself as numbness of the first and half of the fourth fingers, a decrease in the volume of the hand, and a decrease in the range of movement.
Sciatic nerve neuropathy
It usually results from a serious injury or illness (knife or gunshot wound, fracture of the hip or pelvic bones, intervertebral hernia, oncology). It manifests itself as pain along the back of the thigh, lower leg, buttock from the side of the nerve lesion.
Neuropathy of the lower extremities
It can develop due to excessive physical overload, tumors in the pelvic area, hypothermia, and also due to the use of certain drugs. Symptoms: inability to bend forward, pain in the back of the thigh, numbness in the lower leg.
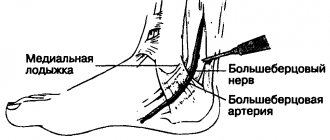
Peroneal nerve neuropathy
It occurs due to bruises, dislocations and other injuries, as well as due to curvature of the spine, carpal tunnel syndrome, and wearing narrow, uncomfortable shoes. Manifestations: inability to dorsiflex the foot, cock-like gait (the patient cannot bend the foot towards himself).
1 Massage
2 Massage
3 Acupuncture