The phrenic nerve (N. phrenicus) is a mixed innervating trunk that is part of the cervical plexus. Here both the spinal roots and the tissues coming from the cervical nodes located in the lower part come together. If dysfunction occurs in the phrenic nerve for any reason, you need to know how to diagnose it in yourself, which specialist to contact and what treatment methods to use to relieve spasticity or eliminate more severe pathologies.
You can make an appointment with a doctor in the “Doctors and appointments” section.
Anatomy of the phrenic nerves
The phrenic nerve is a mixture of spinal branches as well as cervical ganglion structures. They are all intertwined together and form part of the cervical plexus. If we talk about its localization, then it passes in the neck along the anterior surface, in the chest, and phrenic-abdominal branches are formed in the abdominal cavity.
To understand how the phrenic nerve functions, you need to understand what its anatomy is.
First of all, you need to understand that it is paired and is divided into right and left. But both of them depart from the area where the 3rd, 4th and 5th roots of the cervical spine are localized. Then they go down along the spinal cord. The center of the phrenic nerve is located in the anterior part of the cervical spine.
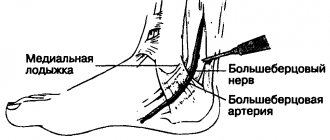
They then pass from the first scalene muscle along the subclavian artery with its further intersection.
When considering the phrenic nerve, it is necessary to take into account its topography in the neck:
- The left process, reaching the chest, crosses the carotid artery, respectively the left subclavian, aorta, and intercostal vein. After this it passes through the pericardium.
- The right one is also located in the chest and runs directly parallel to the brachiocephalic vein. It goes around the right atrium, and before that the superior and inferior vena cava. But, with all this, it should be noted that in some people the position of the right phrenic nerve may be slightly different. In some cases it passes directly through the diaphragmatic opening. In another embodiment, its lateral direction relative to the diaphragm is allowed. It is also worth noting that along the right side of this phrenic nerve the mediastinal pleura runs along its entire length.
Phrenic nerve: symptoms of damage and treatment methods
The phrenic nerve is part of the cervical plexus and consists of sensory and motor branches.
It is responsible for the innervation of the chest and ensures the transmission of impulses to the pericardium, upper abdominal cavity, and pleura.
This nerve is the largest part of the cervical plexus, so its damage causes serious complications. With neuritis, breathing problems and pain of varying degrees of intensity are observed.
Anatomical features
The phrenic nerve begins in the region of the 3-5 roots of the cervical plexus and, moving towards the chest, divides into two large branches. Near its exit, it runs along the anterior scalene muscle and the spinal cord, touching the subclavian artery.
The right branch extends near the lateral surface of the brachiocephalic vein and includes the superior and inferior cava. This part of the phrenic nerve reaches the atrium. The topography of the right branch varies depending on the individual. In some people, the nerve fibers pass through the diaphragm, in others they go around it. But everyone has mediastinal pleura next to them.
The left branch stretches along the subclavian and carotid arteries, the aorta and intercostal vein. This part then reaches the pericardium.
Next to each of these sections is the pericardial-phrenic artery. Only the branches of the phrenic nerve innervate the zone of the same name and influence the respiratory function of a person.
Functions of the phrenic nerve
In addition to innervation of the diaphragm, the nerve is responsible for the following functions:
- transmission of nerve impulses to the skin of the neck and back of the head;
- sensory perception of the muscles located in the area of the collarbone and chest.
The phrenic nerve is part of the cervical plexus, so it affects other branches that:
- innervate the skin of the auricle;
- provide sensitivity to the skin of the outer ear;
- responsible for the motor functions of the muscles of the shoulder, scapula, collarbone;
- innervate the upper part of the abdominal cavity, pericardium, and pleural membrane.
The described anatomical features explain the reasons for the spread of pain beyond the chest with phrenic neuropathy.
Causes of neuropathy
The following pathologies lead to spasm of the diaphragm caused by damage to nerve fibers:
- infectious infection;
- severe intoxication of the body;
- diseases of the spine (spondylosis, osteochondrosis and others);
- neoplasms of various types in the neck and chest;
- heart disease;
- pachymeningitis.
The phrenic nerve is affected mainly due to compression of the chest tissue caused by spasms or injury. Also, the development of a hernia, which compresses neighboring structures, leads to neuritis of the fibers in question.
Often, symptoms of neuropathy are observed in people with a curved spine, or who have been in an incorrect position for a long time: these factors lead to tissue compression in the cervical plexus.
Less commonly, this type of neuritis occurs against the background of:
- autoimmune processes;
- severe stress or neurosis;
- eating spicy food.
It is possible that neuritis may develop after surgery performed on organs located in the chest.
Symptoms
Symptoms of neuritis of the phrenic nerve are manifested mainly by painful sensations. Neuritis does not have a characteristic clinical picture.
Signs of pathology are manifested by the type of coronary disease and other cardiac disorders.
You can differentiate the disease in such situations by taking a nitroglycerin tablet: if relief does not occur, this indicates a disruption in the conduction of signals from the brain.
When the phrenic nerve is damaged, the pain syndrome often radiates to the neck area, which is why, with such damage, an exacerbation of osteochondrosis is often suspected.
The following symptoms indicate neuropathy:
- feeling of lack of air;
- attack of suffocation;
- improper breathing (during inhalation, the chest sinks, when exhaling, it rises);
- rapid breathing;
- hiccups
The intensity of the pain increases with inhalation and swallowing food. At the same time, colic may appear, localized on the liver. In addition, patients with this form of neuropathy experience constipation.
How is it diagnosed?
To identify pinching, the phrenic nerve undergoes a comprehensive examination. To exclude concomitant diseases, the following diagnostic procedures are used:
- radiography;
- Ultrasound and electrocardiogram of the heart;
- MRI;
- CT;
- myelography.
The doctor makes a preliminary diagnosis after an external examination. Diaphragmatic neuropathy is indicated by painful sensations radiating towards the neck, which occur when pressure is applied to the areas where the nerve fibers lie.
Treatment methods
Treatment for damage to the phrenic nerve is aimed at restoring conduction along the damaged fibers. To achieve this result, it is necessary to eliminate the influence of the provoking factor.
The main method of treating phrenic nerve neuritis is drug therapy, which uses:
- Analgesics and non-steroidal anti-inflammatory drugs for pain relief.
- Muscle relaxants to relax muscle fibers and eliminate spasms;
- B vitamins to restore nerve conduction.
Drug treatment is supplemented with physiotherapeutic sessions:
- UHF;
- magnetic therapy;
- electrophoresis;
- phonophoresis.
During the period of remission, doctors recommend performing exercises from a complex of physical therapy, which are selected individually for each patient.
If diagnostic procedures have shown the presence of tumors in the chest or neck (including large hernias), surgical intervention is prescribed, during which such tumors are removed. Surgeries are sometimes resorted to when pinched nerve fibers are caused by injuries.
Source: //bereginerv.ru/patologii-nervov/porazhenie-diafragmalnogo.html
Functions of the phrenic nerves
After it becomes clear what the phrenic nerve is and what its topography is, you should study what functions it performs in the human body:
- Realizes the function of innervation in the occipital region, or more precisely, the epidermis in this area and is partially responsible for the concha.
- It also provides a level of sensitivity in the outer ear along the osteochondral canal.
- Responsible for the area of functioning of the subclavian and supraclavicular parts.
- Controls the level of sensitivity in the area of the shoulder blades.
- In the abdomen and diaphragm, it is responsible for the innervation of the peritoneum and diaphragm, pericardial and pleural tissue.
Phrenic nerve, greater occipital and auricular, anatomy
The cervical plexus is formed by the overlying nerve fibers of the spinal cord. The nerve tissues that make up this plexus innervate:
- cervical skin;
- skin of the back of the head;
- in partial order, the sternocleidomastoid type of muscle fiber (Musculus sternocleidomastoideus);
- trapezius myofibers.
The cervical plexuses make up the following types of nerves:
- lesser occipital;
- large ear;
- supraclavicular;
- phrenic nerve.
Nervus occipitalis
This is a sensitive type of nerve tissue. It innervates the outer skin of the back of the head and partially the concha of the ear.
When this nerve is damaged, the sensitivity of this area, which is innervated by it, is disrupted. Also, when exposed to an irritant, sharp pain will occur. This is the occipital type of neuralgic manifestations. Palpation effect on m. sternocleidomastoideus will reveal its painful areas.
Nervus auricularis magnus
It is also a sensitive type of nervous tissue that innervates the skin of the osteochondral canal belonging to the outer ear, which connects it to the middle ear (external auditory canal, in Latin: meatus acusticus externus).
Another large auricular nerve innervates the area under the lower jaw and, partially, the skin of the ear.
When it is exposed to damaging factors, the sensitivity of these areas with pain in the mandibular region is impaired, and the meatus acusticus externus will still hurt.
Nervi supraclaviculares
These sensory nerve tissues innervate:
- sub- and supraclavicular fossa structures;
- upper scapular zone;
- shoulder.
Impaired sensitivity is manifested by pain, which indicates that the supraclavicular neurofibers are affected.
Nervus phrenicus
Sensory branches with motor types make up the phrenic nerve, which is the largest neurofiber of the cervical plexus.
Diaphragmatic myofibers are innervated by motor nerve branches.
And the sensitive ones are innervated by:
- pleural, pericardial membranes;
- the diaphragmatic region with the peritoneum that is adjacent to it.
When the nervus phrenicus is affected, paralysis develops. Symptoms are expressed by difficulty breathing with the addition of cough.
When this nerve is irritated, the following is observed:
- impaired respiratory function associated with a feeling of lack of air;
- the patient will hiccup and feel the urge to vomit;
- he will feel pain in the chest, cervical area, supraclavicular fossa.
About occipital neuralgia
This pathology is considered a symptom complex, including symptoms of affected nerve fibers that form the cervical plexus.
About the reasons
This type of neuralgic manifestations can develop due to various circumstances. These include:
- infectious pathology;
- intoxication effects;
- disorders of water-salt metabolism in the form of spondylosis, spondyloarthrosis manifestations, spondylitis pathology of a tuberculous nature;
- oncological neoplasms of the cervical and collar zone;
- cardiac and vascular diseases in the form of hypertension, aneurysmal conditions of the vertebral arterial vessels, as well as disturbances of vertebrobasilar blood flow.
About symptoms
The most basic symptomatic manifestation is pain in the area innervated by these nerves. This pain occurs constantly. As a rule, the large, rarely - the small occipital nerve fiber is affected.
The nervus auricularis magnus is also often involved in the clinic. Therefore, a person will feel pain in the area of the concha and external auditory canal.
This soreness will increase when the patient:
- turns his head;
- coughs;
- sneezes.
Painful irradiation spreads to the sub- and supraclavicular areas, sometimes to the facial and scapular areas.
Palpation influence determines impaired sensitivity in the form of hyperesthesia, where the affected nerve tissues pass, pain sensitivity is expressed.
Therapeutic measures are reduced to the use of drugs that eliminate symptoms and treat the underlying pathology.
Clinical picture of phrenic nerve damage
Compression with an ischemic damaging effect on this nerve was observed in five patients with aneurysmal conditions of an atherosclerotic nature of the subclavian arterial vessel, the aortic arch, a pathology described by scientist Takayasu.
The clinical picture was manifested by pain in the left thoracic region (imitation of angina manifestations, “dry pleurisy”), which was not relieved by nitroglycerin and validol drugs. Irradiation of painful sensations manifested itself in the cervical and shoulder areas, aggravated when the patient swallowed, coughed, and breathed deeply.
During fluoroscopy, in order to identify the paresis of the diaphragmatic half, the patient’s weakened lower diaphragmatic breathing will help (the abdomen will not rise during inhalation).
In a patient with a neuroma on the right passing N. phrenicus at the entrance to the chest area, the clinical picture resembled chronic paroxysms of the hepatic type of colic. The patient also hiccupped for a long time.
After surgery, when the nerve fiber was crossed, the symptoms went away, the diaphragmatic part remained paralyzed.
The clinical picture of paroxysms of the diaphragmatic nervous tissue with its damaged sensory fiber structures indicates an intermittent type of ischemic manifestations affecting this nerve.
Also, in three patients who had an aneurysmal condition of the subclavian arterial vessel, the aortic arch, after reconstructive surgical intervention of the vessels was performed, the symptoms of the affected phrenic nerve completely disappeared, since compression phenomena were eliminated.
Source: //NashiNervy.ru/o-nervnoj-sisteme/anatomiya-diafragmalnogo-nerva.html
Symptoms
When, for some reason, an irritant occurs in this part of the body, the phrenic nerve exhibits symptoms such as:
- The pain is similar to angina pectoris due to the fact that it is localized in the left side of the thoracic region.
- Pain may radiate to the neck area. Because of this symptom, this condition is similar to osteochondrosis.
- Most often, discomfort occurs when a person makes sudden breathing movements, sneezes or coughs. This condition can also worsen during sudden bends or turns.
- If neuralgia occurs on the right side, then, most often, the symptoms resemble liver problems, in particular colic. In some cases, a condition of hiccups may occur.
Naturally, how much the phrenic nerve innervates and how severe the pain is depends on what disease or disorder provoked this condition.
Another point that needs to be paid close attention to is the similarity of symptoms with other pathological conditions of the human body. Therefore, before determining why the pain occurs and applying this or that treatment, it is necessary to undergo a comprehensive examination, and the specialist must make a final verdict on what is bothering his patient.
Causes
Irritation of the phrenic nerve can occur for a number of reasons:
- Severe intoxication of the body.
- Various infections.
- Concomitant diseases of the spinal column, including spondyloarthrosis and spondylosis.
- Cardiovascular diseases.
- Hypertension.
- Pachymeningitis.
- Tumors in the cervical or thoracic spine.
But, there is a whole group of reasons that lead to pain and inflammation of the left and/or right phrenic nerve.
Physical exercise
In some cases, when a person places too intense stress on the muscular system, paresis of the phrenic nerve may occur due to intense spasm of the muscle fibers. A kind of pinching occurs, which, with prolonged exposure, can cause inflammation of the nerve fibers.
Hiatal hernia
Due to the development of a hiatal hernia, an increase in these structures is formed. As a result, the phrenic nerve may be affected.
But it is worth noting that this situation occurs quite rarely and is most often associated with birth defects in the development of this part of the human body. The xiphoid process appears on the diaphragm. Although, defects in the structure may be present in the stomach and colon in the anterior or posterior mediastinum. In this case, the phrenic nerve may also be most negatively affected.
With this process of the disease, the patient complains of reflex angina, which occurs due to the fact that the vagus nerve is irritated. Coronary spasm may also occur.
The sufferer may experience a condition where the stomach protrudes above the diaphragm.
Temporary paralysis
When paralysis occurs, the diaphragm is characterized by a high state. At the same time, when you inhale, it does not bulge as it should. And the epigastric region does not descend to the liver. When a person begins to worry or during intense physical work and stress, he or she experiences shortness of breath. During the act of defecation, tension is released. If a person experiences a full stage of paralysis, then the minimal symptoms can become more severe, even leading to fatal asphyxia.
Phrenic nerve irritation
When a state of irritation of these nerve fibers is formed, a person experiences pain of varying intensity, which affects not only the directly affected area, but also radiates to the area of the shoulder girdle, part of the neck and to the area of the shoulder joint. Hiccups may also develop.
Flutter diaphragm
This condition occurs extremely rarely. It is due to the fact that an involuntary contraction occurs in the area of the diaphragm, which is characterized as a spasm or cramp. As a result, there is “pressure” on the adjacent nerve.
Diaphragm spasm and cramps: causes, symptoms, treatment
Diaphragm spasms are involuntary contractions of the muscle that divides the upper abdomen and chest. A spasm of the diaphragm can be felt as contractions, convulsions, and may or may not be painful.
Diaphragm spasms can have a number of causes. In most cases, they do not pose a serious health risk, but they can still cause discomfort.
It is also possible that diaphragm spasm indicates a health problem. This article will discuss the symptoms, causes, and treatment of diaphragm spasms.
What is diaphragm spasm?
A diaphragm spasm is a sudden, involuntary contraction that causes the chest to flutter. It is also common to experience a temporary feeling of heaviness in the chest or difficulty breathing during the spasm.
The diaphragm is a muscle that acts as a divider between the upper abdomen and the chest. The diaphragm plays a crucial role in the respiratory system, helping a person breathe.
The diaphragm contracts when a person inhales, allowing the rib cage to expand so oxygen can enter the lungs. When a person exhales, it relaxes again to help expel carbon dioxide from the lungs.
Other symptoms
Depending on the cause, other symptoms may accompany diaphragm spasm. These may include:
- shortness of breath;
- tightness in the chest;
- hiccups;
- pain in the chest, stomach or back;
- stomach upset;
- nausea;
- vomit;
- difficulty swallowing;
- diaphragmatic paralysis;
- constant cough.
These symptoms can range from mild to severe, depending on the underlying cause.
Causes
There are several potential causes of diaphragm spasm. The most common is a sudden blow to the stomach or chest. Chest injuries are especially common in sports such as boxing, football, etc.
Although the symptoms may be unpleasant, they usually go away within a few minutes.
Let's look at other possible reasons.
Physical exercise
Exercise may cause cramps. This can happen when there is no warm-up before exercise or the load is too heavy.
Hiatal hernia
A surgical hernia is a condition in which part of the stomach rises higher towards the chest. Hiatal hernias occur when age, injury, or recent surgery weakens the muscle tissue of the diaphragm.
When a hiatal hernia occurs, part of the stomach is pushed through an enlarged hole in the diaphragm. This can cause the diaphragm to spasm.
A hernia can be mild or severe, and its severity will determine any additional symptoms. The most severe cases require immediate medical attention as they can damage the stomach, cause bleeding or affect breathing.
Temporary paralysis
A sudden blow to the solar plexus area can temporarily paralyze the diaphragm. This can lead to significant breathing difficulties. A person may panic if they cannot breathe, which can worsen symptoms.
//www.youtube.com/watch?v=2tCUhHaenmI
However, temporary paralysis quickly passes.
Phrenic nerve irritation
The phrenic nerve controls the movement of the diaphragm muscle. Irritation or damage to this nerve or any inflammation can cause spasms in the diaphragm in addition to causing hiccups and difficulty breathing.
A variety of factors can cause phrenic nerve irritation, including:
- breathing and simultaneous consumption of spicy food;
- binge eating;
- physical trauma;
- surgical complications;
- cancer;
- non-cancerous tumors;
- neurological disorders;
- autoimmune diseases;
- infectious diseases.
Flutter diaphragm
Diaphragm flutter is a rare condition that causes frequent spasms or cramps of the diaphragm. Doctors can't say for sure why this happens.
Episodes of spasms can occur suddenly and last for minutes or even hours, significantly affecting a person's quality of life. The pain may be present in the chest, mid-abdomen, or back, making diagnosis difficult. There is no standard treatment for diaphragm flutter, as there is insufficient understanding of the causes of this pathology.
Diagnostics
Symptoms of diaphragm spasm are often similar to symptoms of gastrointestinal or heart problems. In most cases, symptoms disappear within a few minutes without the need for diagnosis by a doctor.
However, if diaphragm spasms occur frequently for no apparent reason, you should seek medical help.
If a doctor suspects that a medical condition is causing the spasms, the following may be used to diagnose:
- X-ray;
- blood tests;
- CT scan;
- MRI;
- endoscopy;
- manometry.
Treatment, how to relieve spasm?
Treatment for diaphragmatic spasms depends on the underlying cause. Diaphragm spasms resulting from a sudden blow may cause discomfort, but symptoms should subside within a few minutes, making treatment unnecessary. It is extremely important to rest and focus on maintaining regular breathing until the symptoms subside.
Let's look at the causes of diaphragm spasms that require treatment.
Forecast
Most diaphragm spasms are temporary and go away within a few minutes. Muscle interventions, medications, and lifestyle changes can help manage persistent symptoms.
If diaphragm spasms occur due to a medical condition that requires medical attention, such as a hiatal hernia, phrenic nerve irritation, or diaphragmatic flutter, your doctor will help you create an individualized treatment plan.
This article uses materials from Medical News Today magazine.
Source: //ChtoiKak.ru/spazm-diafragmy.html
Diagnostics
In order for a specialist to clearly determine whether there is pinching of the phrenic nerve or inflammation, it is necessary to conduct a comprehensive examination. But, before conducting hardware diagnostics, the doctor will perform a complete external examination.
He will palpate the painful areas to see how severe the symptoms are. This is done by ordinary pressure on the muscle parts adjacent to the nerve fibers. And only after he makes a preliminary diagnosis of neuropathy or neuralgia of the phrenic nerve, will he prescribe various types of hardware diagnostics to clarify the condition.
Necessities include:
- X-ray image.
- Carrying out ultrasound examination.
- Carrying out an ECG to make sure that the problem is in the nerve fibers and not in the pathology of the cardiovascular system.
- Magnetic resonance therapy, which allows you to clearly localize where the pathological process is located in the body.
- CT scan.
- Myelography.
Treatment - how to relieve spasm
If the entire complex of examinations has confirmed the presence of such a process in the body, the doctor will prescribe the appropriate treatment.
All manipulations are aimed at restoring the nerve conduction of those fibers that have lost it partially or completely. But before doing this, it is necessary to naturally eliminate the irritating factor. Otherwise, the treatment will not have the desired effect.
In the vast majority of cases, a positive result can be achieved through the use of drug therapy. Moreover, as in the treatment of any disease of the musculoskeletal system, in this case it will be complex. Includes:
- Analgesic painkillers.
- Non-steroidal anti-inflammatory drugs.
- Muscle relaxants that relieve muscle tissue paresis. This allows you to eliminate spasms, which have the most negative effect on the compression of nerve fibers and their further inflammation.
- Preparations with a complex of B vitamins. They allow a comprehensive effect on the central nervous system, supporting its full functioning and at the same time restoring nerve conduction.
Physical exercise
The doctor, in addition to drug treatment, will recommend performing special physical exercises. But it is necessary to remember that such gymnastics should be carried out under the supervision of rehabilitation specialists in order to prevent the deterioration of one’s own condition.
It is also important to remember that any physical activity can be performed only if there is no acute stage of the disease.
Hiatal hernia
When a patient has a hernia, the doctor may recommend the following treatment methods:
- Drug therapy in the form of antacids (allows the binding of hydrochloric acid in gastric juice).
- Drugs that normalize gastrointestinal motility, as well as histamine receptor blockers.
- Physical therapy is also used to strengthen the ligaments. But it must be performed no more than 1 hour before meals.
- It is also very important to follow a special diet, excluding the main provocateurs of the disease, such as overeating and irregular eating. Without this, it is impossible to cure a diaphragmatic hernia. And in the early stages of the development of pathology, this point is predominant.
- But if the initial stages of the disease are missed, or all of the above conservative treatment methods have not helped, then surgical intervention will help to cope with the pathology. This is important to understand, since severe damage to the esophagus will develop in the future. Gastroenterologists insist on surgical intervention.
Phrenic nerve irritation
In a state of irritation, the doctor can recommend a variety of treatment strategies. The final choice depends on the cause that led to the occurrence of the pathology and, of course, on the intensity of the symptoms.
In the mildest cases, the doctor may recommend reducing the amount of food you eat at one time and switching to a smaller diet.
In case of serious processes, drug therapy is used to eliminate spasmodic conditions and reduce the level of discomfort. Physical activity may also be recommended. The main emphasis in this case should be on stretching nearby muscles or, conversely, pressing on them. In any case, it is necessary to select exercises only in consultation with an experienced rehabilitation therapist.
Using these recommendations, you can avoid the pathological development of irritation and inflammation of the phrenic nerve. It is always necessary to take into account that even with minor symptoms, it is necessary to contact an experienced specialist who will help eliminate the problem in the early stages of its development and prevent it from developing into a more severe form.