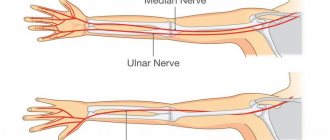
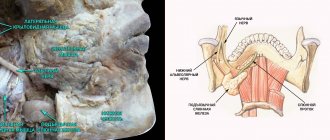
The peroneal nerve arises from the sciatic nerve at the level of the popliteal fossa. It runs in the outer part of the lower leg, foot, carries both sensory and motor fibers, that is, it is mixed in function. Its branches:
- External cutaneous nerve of the calf - provides sensitivity to the skin of the lower leg in the posterior outer region.
- Superficial peroneal – provides flexion and abduction of the foot, sensitivity of the skin on the dorsum of the foot.
- Deep peroneal – provides extension of the foot and toes, sensitivity of the skin of the foot.
With neuritis, these functions are disrupted.
Our expert in this field:
Lashch Natalia Yurievna
Neurologist of the highest category, candidate of medical sciences, associate professor. Laureate of the Moscow City Prize in the field of medicine.
Call the doctor Reviews about the doctor
Why does peroneal nerve neuritis occur?
The main reasons for the development of the disease:
- Poisoning with various substances.
- injuries .
- Diabetes mellitus - one of the complications of the disease is damage to small vessels, impaired circulation in various nerves, including the peroneal nerve.
- Vasculitis is an inflammatory process in the wall of blood vessels.
- Poor circulation due to prolonged compression. This often occurs in people who like to sit with their legs crossed.
- Dysproteinemia is a condition in which there is an imbalance in the ratio of different types of proteins in the blood.
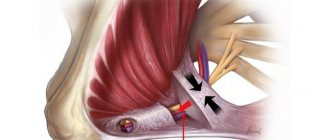
- Tunnel syndrome - neuritis occurs as a result of compression of the nerve trunk between the bone and ligaments. The “tunnel” where the peroneal nerve is most often compressed is where it passes near the head of the fibula.
Have you noticed numbness or impaired movement in your leg? Visit a neurologist – the effectiveness of treatment may depend on how early you see a doctor.
Enduring pain is dangerous!
Message sent!
expect a call, we will contact you shortly
Causes
Neuritis (neuralgia) of the tibial nerve can be provoked by:
- injuries (fractures, bruises, sprains, dislocations, etc.);
- foot deformities (for example, flat feet);
- acute and chronic infectious diseases;
- compression when staying in an uncomfortable position for a long time, walking in tight shoes with heels;
- compression by joints and/or ligaments deformed due to overload or general diseases (rheumatoid arthritis, gout, arthrosis);
- compression by swollen muscles, overload of which was caused by poor posture, pathological changes in the spine, etc.;
- metabolic disorders (diabetes, hypothyroidism, etc.);
- intoxication with heavy metals, alcohol, etc.;
- vascular pathologies;
- tumor formations, etc.
Neuritis of the tibial nerve, caused by its pinching by the walls of the tarsal canal, is often provoked by prolonged running or walking. This condition is called tarsal tunnel syndrome.
Treatment of peroneal nerve neuritis
The principles of treating the disease are the same as for inflammatory processes in other nerves:
- B vitamins help improve the functioning of the nervous system.
- Drugs that improve blood circulation in small vessels.
- Drugs that improve metabolic processes in nervous tissue and the transmission of nerve impulses.
- Physiotherapy.
- Massage.
- Physiotherapy.
If the neuritis occurs as a result of tunnel syndrome, then solutions of anesthetics and adrenal hormones (glucocorticoids) that suppress inflammation are injected into the place where it is compressed. In severe cases, the doctor may recommend surgery to relieve compression of the nerve trunk.
If the inflammatory process occurs after an injury, and treatment for 1-2 months does not bring any effect, the neurologist prescribes an additional examination and raises the question of surgical treatment.
The effectiveness of treatment for neuritis depends on how early it is started. Don't delay your visit to the doctor. An experienced neurologist is ready to see you at the Medical Center International Clinic Medica24.
We will call you back
Message sent!
expect a call, we will contact you shortly
The peroneal nerve has a mixed structure (it includes both sensory and motor fibers); together with the tibial nerve, it provides muscle movement and sensitivity to the skin of the lower leg. When an inflammatory process occurs—neuritis—these functions are disrupted. The following characteristic symptoms occur:
Movement disorders. It is impossible to straighten the foot and toes, or turn the foot outward. The foot constantly hangs down and is slightly turned inward. This picture is designated by a special Latin term - pes equinovarus. A “cock’s gait” (steppage) occurs: when taking a step, a person raises his foot high so as not to touch the ground with his toe. It is impossible to raise your toes and stand or walk on your heels.
Sensory disturbances. The sensitivity of the skin to touch and pain on the outer surface of the lower leg and the back of the foot is reduced.
If you are bothered by similar symptoms, do not hesitate, consult a doctor. The effectiveness of treatment is highest if it is started in a timely manner.
Symptoms
Damage to the nerve at the beginning of its branch from the sciatic nerve impairs the flexion functions of the fingers and toes. The patient cannot walk on his toes and is therefore forced to walk on his heels. The muscles in the back of the lower leg atrophy, and in the same area and the sole the sensitivity of the skin is impaired. The Achilles reflex gradually fades away.
Neuritis of the tibial nerve is accompanied by severe pain (neuralgia) in the back of the leg and in the calf muscle, and autonomic-trophic disorders.
With tarsal tunnel syndrome, plantar pain is burning in nature and spreads to the calf muscle. At the same time, the sensitivity of the edges of the feet is impaired, the foot itself is flattened, and the toes take on a claw-like position.
What diagnostic methods are used for neuritis of the peroneal nerve?
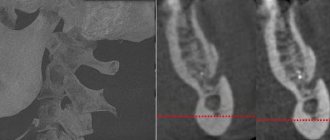
After an examination and identification of characteristic symptoms, the doctor may prescribe you an electroneuromyography - a study during which, using special electrodes connected to a device, you can evaluate the nature and strength of nerve impulses and check how the lower leg muscles respond to them. This helps confirm damage to the peroneal nerve and identify at what level the neuritis occurred.
You may also be prescribed a biochemical blood test and other laboratory tests if the doctor suspects that the symptoms of peroneal nerve neuritis are caused by diabetes mellitus or infections.
In some doubtful cases, they resort to radiography, CT, MRI and other studies.
The international clinic Medica24 employs professional doctors and has installed new modern diagnostic equipment. Here they will accurately identify the cause of your symptoms, establish a reliable diagnosis, and prescribe the correct treatment. Contact us at any time of the day by phone.
The material was prepared by Natalya Yurievna, a neurologist at the international clinic Medica24, Candidate of Medical Sciences Lasch.
Treatment
At the First Medical Clinic, treatment of neuritis (neuralgia) of the tibial nerve is successfully carried out using non-surgical methods.
First of all, pain is eliminated. From this point of view, therapeutic blockades - injections of anesthetic drugs into the area of nerve damage - are especially effective.
In order to relieve inflammation, tissue swelling and reflex muscle spasm, local injection therapy - antibacterial, anti-inflammatory, analgesic, muscle relaxant, vitamin and other drugs are injected into the pathology site.
is used to suppress pathological processes and activate tissue self-healing . This method is based on the isolation of plasma from the patient’s venous blood using a special technology. Such plasma contains a large number of platelets - sources of growth factors, anti-inflammatory cytokines and other bioactive substances. As a result of treatment with autoplasma, inflammation, swelling and pain go away, and the patient returns to normal activity.
Depending on the underlying cause of neuritis (neuralgia) of the tibial nerve, the course of treatment may include methods such as:
- transcutaneous electromyoneurostimulation - delivering weak current pulses to stimulate muscle activity;
- manual therapy and osteopathy;
- massotherapy;
- shock wave therapy;
- reflexology , etc.
The required amount of therapeutic assistance can only be determined by a specialist after diagnostic procedures. If symptoms of neuritis (neuralgia) of the tibial nerve appear, we recommend that you contact the First Medical Clinic in a timely manner.
You can make an appointment for a consultation and appointment by phone
Clinical relevance
Damage to the sural nerve can occur due to direct trauma and fracture of the heel bone, as well as during surgery in this area. Damage to the sural nerve is accompanied by impaired sensitivity in the area of its innervation and does not lead to significant functional deficit or disability, since its function is compensated by other nerves. For this reason, it is often used for biopsies (for example, to diagnose neuropathies), and also as a donor when nerve transplants are needed. However, there is evidence of a higher complication rate than with peroneal nerve biopsy, particularly persistent postoperative pain, dysesthesia, and paresthesia.
The nerve path includes passage under the dense fibrous arcade (arch) or fibrous formation of the Achilles tendon (here chronic frictional irritation may occur), then (in the distal third of the leg) it passes superficially. Symptoms associated with irritation of the sural nerve include chronic (since the diagnosis is usually delayed) pain in the posterolateral part of the leg, aggravated by physical activity. Radiating pain/tingling in the foot may also occur.
How to diagnose the disease?
Tunnel neuropathy of the peroneal nerve can be suspected based on typical complaints (weakness of the lower leg muscles, numbness of the outer surface of the lower leg and dorsum of the foot, burning shooting pain in the leg below the knee level). The diagnosis can be confirmed using stimulation electroneuromyography (ENMG).
This study allows using an electric current to “ring” the sciatic, tibial and peroneal nerves along their entire length and identify the local area of damage. In the place where the nerve is subjected to mechanical compression, its myelin sheath is damaged, which leads to a decrease in the speed of propagation of the nerve impulse along this segment of the nerve trunk.
It is this parameter during ENMG that is the most informative for establishing the diagnosis of tunnel neuropathy.
Trigeminal neuralgia - symptoms and treatment
There are two types of pain due to trigeminal neuralgia:
- constant, dull, periodically intensifying pain without wide irradiation, arising in the area of distribution of one or another branch of the nerve and not accompanied by pronounced autonomic reactions;
- pain of a paroxysmal nature, lasting from several minutes to several hours.[4][5]
The intensity of the attacks varies: from mild but frequent, lasting a few seconds, to strong and unbearable, lasting for minutes and causing severe suffering.
Attacks often occur spontaneously, without any irritants, or as a result of hard and cold food getting into the mouth, touching, drafts, hypothermia under air conditioning, jaw movements, etc.
The attack usually begins with pain in one branch of the nerve - the site of the primary lesion, then the pain spreads to other branches, often radiating to the back of the head, to the ear nerves, to the neck and even to the area of the thoracic nerves.
Severe attacks are usually accompanied by autonomic reflex reactions: redness of the face, lacrimation, runny nose, drooling, sometimes swelling of the cheeks, eyelids, and slight swelling of half the nose.
The patient's suffering is manifested by general anxiety, rubbing the painful area with his hand, putting pressure on this area, and smacking his lips. This layering of new stimuli obviously accelerates the moment of the onset of an inhibitory state in the center of pain perception, which usually gives way to an attack.
As motor manifestations in connection with a painful attack, tic-like muscle twitching or spasmodic contractions occur. The maximum twitching or contraction of the muscles corresponds mainly to the zones from which the pain begins, i.e., to the sites of primary damage.
With long-term disease, graying of the scalp hair on the affected side is sometimes observed.
Sometimes paroxysmal neuralgia is accompanied by a rash of herpes zoster (herpes zoster), located according to the primary lesions of certain branches, sometimes affecting the corneal mucosa.
Periods of exacerbations may alternate with periods of remission, which last for months, sometimes years.
Outside of an attack, usually no disorders are observed: no pain points, no objective sensitivity disorders. Sometimes you can notice a decrease in pain sensitivity, mainly in the area of the branch that was the site of the primary lesion. Less commonly, decreased sensitivity is found in the area of all branches of the trigeminal nerve. In some cases, outside of attacks, patients experience mild dull pain. Pain occurs at any time, but more often during sleep.[6][7]