Today, pudendal neuropathies (neuropathy of the pudendal nerve) are encountered quite often in the clinical practice of a urologist. They manifest themselves in the form of a syndrome with a general name - chronic pelvic pain.
Both women and men face this problem throughout their lives. So let's figure out what pudendal neuropathy is, why it occurs, how to diagnose it and how to treat it.
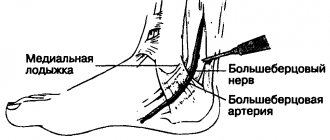
Let's start with the fact that complaints of pain in a sitting position, discomfort, numbness, burning in the pelvis can be explained by the anatomy of the pudendal nerve. This nerve leaves the spine at the level of 1-3 lumbar vertebrae and goes to the pelvis, passing between the muscles and ligaments. More precisely, between the piriformis muscle and the sacrospinous ligament. Note in Figure 1 where the pudendal nerve is labeled as. N.pudendus.
According to scientific research, most often the pudendal nerve is “pinched” either between two ligaments (sacrospinous and sacrotuberous), or between the piriformis muscle and the sacrospinous ligament. If this compression occurs, swelling will form around the nerve. This area begins to hurt, and the pain increases in a sitting position, actually due to the location of the area of nerve compression. After the nerve has passed these “dangerous zones”, it enters an equally dangerous canal - Alcock’s canal (the area of the ischial spine), however, based on literature data and our experience, compression in this canal occurs much less frequently.
Why is this happening?
There is evidence that risk factors for compression of the pudendal nerve are:
- Chronic microtraumas (non-systematic exercise according to the principle: “it’s better rarely, but wear it out.” This includes cycling, exercise in the gym, team sports).
- Hormonal disorders (diabetes mellitus, hypothyroidism, etc.)
- Systemic connective tissue diseases (collagenosis, etc.)
- Chronic intoxication (alcohol)
- Genetic predisposition
- Congenital anatomical features of the pelvis
About the causes and symptoms of functional disorders
For the etiology of damage, the proximity to the ischium, which the nerve goes around entering the pelvic cavity, as well as the relatively shallow depth of the terminal branches under the surface of the skin and mucous membranes of the pelvic organs, are important. Therefore, dysfunction can occur as a result of:
- injuries to the perineal area;
Perineal trauma can lead to more serious consequences - hypothermia of the perineal area;
- pressing against the ischium by the piriformis muscle due to the presence of a volumetric process in the small pelvis, or due to compression between the pelvic ligaments, or due to another reason;
- damage to the formations that make up the sacral plexus or the sacrum itself.
Provoking factors may be:
- horse riding or cycling (frequently or professionally);
- prolonged labor;
- fracture of the pelvic bones (from a fall from a height, in a car or plane accident).
To understand that something is wrong with the genitofemoral nerve is made possible by dysfunctions of the organs located in the pelvis. These may be sensitivity disorders or autonomic disorders.
The first category includes both varying degrees of decrease in sensitivity (up to its complete loss) and an increase in pain to unbearable limits.
Deviations in autonomics are expressed by disturbances in the functioning of glands and other structures containing smooth muscle fibers, in particular, disorders of the mechanism of blood supply to the cavernous bodies of the penis or clitoris.
Trophic disorders of the skin of the perineum, scrotum and peri-anal area can also be a sign of disorders.
In addition to physical factors, the cause of pathology can also be general somatic diseases:
- tuberculosis;
- collagenoses;
- blood supply disorders due to endocrine disorders and vascular accidents or for any other reason.
Diagnosis of pudendal nerve neuropathy
Today, there are clinical criteria that suggest pudendal neuropathy. We are talking about the Nantes criteria. Answer yourself the question whether you have these clinical symptoms.
- Pain in the area of innervation of the pudendal nerve: from the anus to the clitoris/head of the penis.
- The pain is felt worse when sitting.
- The pain does not cause awakenings at night.
- The pain is not accompanied by a decrease in tactile sensitivity.
Additional criteria:
- The pain is burning, shooting, stabbing, and may be accompanied by slight numbness.
- The pain worsens during the day and subsides after sleep.
- Mostly the pain appears on one side.
- Pain may be triggered by defecation.
If you notice that you have these symptoms, you should immediately consult a doctor.
Already at the initial appointment, the doctor will be able to conduct additional special manual tests.
Only a urologist specializing in the treatment of pelvic dysfunction should perform a manual examination (both in a gynecological chair and on a couch). This is due to the need to thoroughly and carefully examine the areas most susceptible to compression. An insufficiently complete examination is fraught with the loss of valuable diagnostic information, incorrect interpretation of symptoms and low effectiveness of treatment.
The next step is to conduct electrophysiological studies,
for example, assessing the bulbocavernosus reflex using electromyography.
All possible diagnostic methods are carried out at the Expert Urogynecology Clinic by highly qualified specialists in the field of pelvic floor pathology. Differential diagnosis is carried out with lesions of other pelvic nerves, as well as with myofascial syndrome. The latter is characterized by painful sensations when pressing on various trigger points in the muscles.
| anonymously to the doctor, through the feedback form, we will try to help you. | Ask a Question |
Clinical manifestations of root compression in osteochondrosis
| Spine | Spread of pain/area of sensory loss | Atrophied muscles | Decreased/active reflexes |
| L4 | Along the inner anterior thighs to the knee and sometimes below | Quadriceps femoris | Knee |
| L5 | From the lower back to the buttock >> along the outer edge of the thigh >> along the anterior outer surface of the lower leg to the 1-3 toes | Tibialis anterior muscle | — |
| S1 | From the lower back to the buttock >> along the outer back edge of the thigh >> along the outer edge of the lower leg to the 4–5 toes and heel | Triceps surae muscle | Achilles |
*The table shows the most commonly affected roots that can cause pelvic pain (the L5, S1 roots are most often affected).
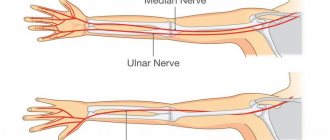
In conclusion, one cannot help but mention such a pathological condition as COMPRESSION NEUROPATHY - damage to the peripheral nerves, in this case the pelvic nerves, when they are compressed, as the cause of pelvic pain.
Such compression may occur as a result of narrowing of the musculofascial and/or musculoskeletal canals in which the nerves pass. This occurs due to local proliferation of connective tissue, with prolonged monotonous overstrain of the musculo-ligamentous apparatus in athletes and/or as a result of professional activity, with soft tissue injuries and/or dislocations.
Compression syndromes are also called tunnel syndromes, when due to compression of the nerve trunk and the vessels feeding it, certain changes occur in it.
In our article we will look at damage (neuropathy) of the pudendal nerve, obturator nerve, “causalgia syndrome of the inguinal-genital zone”, lateral cutaneous nerve of the thigh and damage to the lumbosacral plexus.
Symptoms of sciatic nerve compression are discussed in piriformis syndrome (see above).
Treatment of pudendal nerve neuropathies
Therapeutic and diagnostic blockades
Conservative treatment is aimed primarily at removing tension (decompression) of the nerve in “critical zones” and restoring normal trophism.
The first stage is recommended to carry out therapeutic and diagnostic blockades of these very problem areas, which we talked about at the very beginning (areas of ligaments and muscles).
The most common are blockades with local anesthetic (lidocaine, bupivacaine) and glucocorticoid (betamethasone).
Transvertebral magnetic neuromodulation
Within the walls of our center, a unique method of treating neuropathic pain has been developed and adapted. It is highly effective for true pudendal nerve neuropathy and is used in parallel with blockades. The deep impact of a directed magnetic pulse with a certain frequency on the area where the pudendal nerve exits the spine (level S2-S3) allows you to “reset” the innervation and break the vicious circle of pain. The course of treatment with magnetic neuromodulation ranges from 10 to 15 sessions, depending on the severity of the disease.
Botulinum therapy.
Indicated in the presence of muscular-tonic syndrome, when the muscle needs to be relaxed. Botulinum toxin type A is successfully used specifically to target this pathological component.
When used correctly (according to indications and with good navigation via ultrasound), the risks of complications are minimal.
Transcranial magnetic neuromodulation
The newest method of influencing brain structures.
In Russia, we are leaders in the use of neuromodulation of the central and peripheral nervous system for the treatment of pelvic floor dysfunction and chronic pelvic pain syndrome. This technique is aimed at eliminating central sensitization - a condition that develops during a long course of the disease, when the patient did not receive adequate treatment in time.
Remember, even with a prolonged course of the disease there is a way out!
Manual therapy.
The main goal of treatment by an osteopathic neurologist is to eliminate biomechanical disorders and pathological changes in soft tissue structures.
When a person has a sore muscle, he tries to reflexively “save” it by changing his position, sitting or walking. This leads to the fact that these structures, which bear an additional “volume of work,” begin to experience additional stress and get sick. And this only strengthens the vicious circle of disease development. With the help of manual techniques, it is possible to return to its place what has been displaced and is involved in the pathological process.
Pudendal nerve neuropathy: a patient’s history of recovery
Diagnosis and treatment
In order to correctly carry out diagnostic measures, the patient must tell the doctor about all the existing symptoms. For example, in the presence of pathology, pain decreases if the patient is in a supine position and increases if he is sitting. When applying cold, the patient may also experience temporary relief - this indicates the presence of neuropathy. The doctor can also examine the patient by palpation to find areas characteristic of a pinched nerve.
The following diagnostic measures are prescribed:
- ultrasound examination - to determine whether there are disturbances in blood flow through the pudendal artery;
- Dopplerography - performed for the same purpose as ultrasound;
- novocaine blockade of the nerve tract - check whether discomfort disappears after the procedure.
Only after a diagnosis has been established, the patient is prescribed therapy, the main purpose of which is to restore nerves, as well as relieve unpleasant symptoms in the perineum and pelvis.
In this regard, the patient is recommended the following medications:
- Muscle relaxants are needed to relax the muscles of the genitofemoral nerve.
- Anticonvulsants - These relieve pain; Gabapentin is a popular one.
- Sedatives are also prescribed to reduce pain.
- Solutions of hormones, as well as anesthetics - for blocking the pudendal nerve - drugs of the Neuromultivitis class. When used, urination and bowel movements should normalize, and discomfort should go away.
- Rectal or vaginal suppositories with an active ingredient such as Diazepam.
- The use of vitamins C and group B to normalize the general condition.
- Physiotherapeutic techniques - phonophoresis, electrophoresis. They are used against the background of chronic pathology.
- Physiotherapy exercises are selected individually for each patient and are needed to massage the perineal muscles.
If all of the above methods are ineffective, then the patient is prescribed surgical decompression.
What functions does it perform?
- Innervates the muscle that elevates the anus and sphincter.
- Innervates the sphincter of the urinary canal.
- Innervates the female clitoris and the cavernous bodies in men.
- Makes the skin of the anus and external genitalia sensitive.
From the above list it is clear that the pudendal nerve plays a very important role both in the intimate life of a person and during bowel movements and urination. This nerve includes a large number of autonomic fibers that ensure the correct functioning of the sphincters without the use of conscious tension. After all, people never think, do not try to control and do not consciously squeeze their muscles so as not to urinate or defecate completely accidentally at the wrong moment. These functions are performed by the autonomic fibers that enter the pudendal nerve.
Pinching: reasons
Trouble may occur due to the piriformis muscle located in the pelvic cavity or due to compression between a pair of ligaments.
In addition, the pudendal nerve can be damaged after unforeseen situations, which include a car accident or a fall from a height. In such situations, a fracture of the pelvic bones may occur. Very often, the cause of chronic pain is damage to the nerve during childbirth or its involvement in the growth of a malignant tumor.
Preventive measures
Pinched pudendal nerve is a recurrent disease. If the patient does not follow certain rules after completing the therapeutic course, a re-exacerbation is possible. It is characterized by increased symptoms, which are difficult to treat with medication. You can avoid relapse by strictly following the following recommendations:
- It is necessary to protect the groin area from injuries, direct blows, and prolonged exposure to cold.
- Professional equestrians and cyclists should take frequent breaks from exercise.
- In case of a hip fracture, traction should be carried out using a perineal fixator, the support area of which is no more than 9 cm (a softening pad should be placed under it).
- If you plan to intramuscularly administer a solution of magnesium sulfate, this must be done extremely carefully to prevent the formation of ischemic necrosis of the gluteal muscles.
If the triad characteristic of a pinched pudendal nerve reappears, it is important to immediately seek medical help.
Results
Thus, it was discussed what the pudendal nerve is, symptoms and treatment for its pinching, and diagnosis. In order to avoid this disease, it is recommended to be careful and avoid injury, as well as to lead an active lifestyle, exercise and have an active sex life. Well, if trouble does happen, then you must strictly follow the doctors’ recommendations.
Damage to the pudendal (genital) nerve often causes chronic pain in adults, localized in the pelvic area. In men, this pathology occurs three times less often than in women. The anatomy of the pudendal nerve can explain this phenomenon.
Therapy methods
Treatment of genitofemoral nerve neuropathy in women and men begins with drug therapy. Patients are prescribed:
- regular blockades with injections of glucocorticoids with local anesthetics;
- enhancement of neuromuscular transmission by antiepileptic rectal drugs that contain diazepam;
- decreased tone of the piriformis muscle with muscle relaxants;
- nutrition of nervous tissue with vitamins B and C: they can be taken separately in the form of tablets or used as a component of a solution for blockade;
- physiological effects to restore impaired functions: phonophoresis, electrophoresis.
Experts have found that the development of neuropathy contributes to increased anxiety, and in especially severe cases it becomes the cause of deep depression.
In such cases, correctional therapy is used, antidepressants are prescribed, and work is carried out with a psychologist. Many people are helped by physical exercises, the meaning of which is to gradually compress and relax the muscles of the perineum. Full recovery takes time. The indicated course is long - stretches for six months. If conservative therapy does not cure the neuropathy, surgery is prescribed to eliminate the cause of the pinched pudendal nerve. Radical measures are always effective, but any surgical intervention has a long recovery period.
Ignoring the problem can lead to unwanted complications. The disease can become chronic, in which case it will be extremely difficult to eliminate the main symptoms with medication.
Clinical practice knows of cases where patients with the described diagnosis became impotent and completely lost control over bowel movements and urination.
Structural features
The described element is small in size.
The pudendal nerve originates from the sacral plexus, exits through the infrapiriform foramen along with the internal pudendal artery, bends around the sciatic spine from behind and enters the ischiorectal fossa through the lesser sciatic foramen. There it lies on the surface of the obturator muscle and passes through the Alcock canal (it is formed by the split fascia of the obturator internus muscle). Then they diverge into three branches: They innervate the muscle that lifts and holds the anus, the anal sphincter, the urethral sphincter, the muscles of the perineum, the genital organs - the cavernous bodies of the penis in men and the clitoris in women. The branches provide sensitivity to the skin of the external genitalia and anus. Any damage to the nerve can provoke disruption of sexual life, bowel movements and bladder processes.
SYNDROME OF "CAUSALGIA OF THE INGUINAL-GENITAL AREA"
This syndrome develops with damage to the iliohypogastric (n. iliohypogastricus), ilioinguinal (n. ilioinguinalis), and genitofemoral (n. genitofemoralis) nerves.
The function of all three of these nerves is to provide sensitivity to the skin in the groin area.
Neuropathy of each nerve can occur separately, but the similarity of their anatomy and clinical manifestations makes it possible to combine their damage into a single syndrome - the “causalgia of the inguinal-genital zone” syndrome.
The main complaint is burning pain in the groin area, spreading along the front surface of the thigh and along the abdominal wall. The pain intensifies when the muscles of the anterior abdominal wall are tense - when straining, when walking with long steps, when hyperextending the lumbar spine.
Sometimes a gentle gait is observed: a person moves in small steps with a lean forward, which reduces abdominal tension and, accordingly, pain.
An additional diagnostic test is to apply pressure to a point located slightly to the center of the anterior superior iliac spine. In this case, the pain characteristic of this syndrome is reproduced.
Other procedures
Often, treatment of a pinched pudendal nerve requires the support of a good psychologist who performs correctional therapy and prescribes antidepressants. You may need to prescribe vaginal or rectal suppositories that contain diazepam. The patient may be prescribed special physical exercises, the meaning of which is to slowly compress and relax the muscles located in the perineum.
In situations where conservative treatment methods do not have a positive effect, decompressive surgeries are performed. They are performed in special centers for the treatment of chronic pelvic pain.
NEUROPATHY OF THE OPTURATIVE NERVE (n. obturatorius)
The first signs of compression of the obturator nerve are usually pain that occurs in the groin area and along the inner surface of the thigh, in the hip joint.
Usually the pain intensifies with coughing, tension of the abdominal muscles, that is, with any conditions that increase intra-abdominal pressure. In addition, hip extension, abduction, and inward rotation contribute to increased pain.
There may be a feeling of numbness and “crawling” in the middle and lower part of the inner thigh. Later, a zone of reduced sensitivity (hypesthesia) appears in these same areas.
Motor disorders are manifested by weakness of the adductor muscles of the thigh: weakness when bringing the hips together, difficulty in fulfilling the request to put one leg on the other.
NEUROPATHY OF THE EXTERNAL CUTANEOUS NERVE OF THE FEMOR (n. cutaneus femoris lateralis)
This is a sensory nerve; it is responsible for sensitivity in the area of the outer (lateral) thighs.
Neuropathy is manifested by burning persistent pain in the area of the outer surface of the thigh and a feeling of numbness, “crawling”, tingling in the same area.
These phenomena intensify when standing up and walking.
People suffering from neuropathy of the external cutaneous nerve of the thigh describe pain when standing up as a flashing, “ball of fire” in the lateral thigh area and spreading down the thigh, before reaching the knee.
The pain point for this type of neuropathy is detected under the anterosuperior iliac spine.
Since there is no limit to indignation, or about neuropathy
In addition to neuralgia, the pudendal nerve can also become the scene of an inflammatory process, then they talk about neuropathy (neuropathy), or neuritis of the pudendal nerve (a term rarely used today).
Neuropathy differs from neuralgia in the presence of structural changes in the pudendal nerve, as well as movement disorders and the possibility of loss of sensitivity, which serves as a reason for indignation and upset of the patient, because we are talking about neither more nor less than the genitals.
The cause of the pathology (also called pudendoneuropathy) is the implementation of two mechanisms:
The first is illustrated by the consequences of long-term or unsuccessful horse riding or cycling (compression by a hard saddle), and the second by the consequences of surgical intervention - for example, when traction of the hip with the use of a perineal fixator, tension occurs on the nerve pressed to the pubic region.