Author: Sozinova A.V., obstetrician-gynecologist, has been in continuous practice since 2001.
Hydrops of the fetus is a pathological condition in which fluid accumulates in all cavities of the body and generalized edema is present (edema of the whole body - anasarca).
In most cases, hydrops fetalis is observed during Rh-conflict pregnancy and hemolytic disease of the newborn. The prevalence of this condition is 1 case per 1000-14000 births. There are immune and non-immune hydrops fetalis.
Causes
The main cause of the development of immune fetal hydrops is hemolytic disease.
The reason that led to the development of non-immune hydrops fetalis often remains unrecognized, but the following factors are identified:
- chromosomal pathology of the fetus (Down syndrome, mosaicism, trisomy, Shereshevsky-Turner syndrome and others);
- gene diseases: deficiency of glucose-6-phosphate dehydrogenase, A-thalassemia, Noonan syndrome, achondrogenesis, thanatophoric dwarfism, Pen-Shockey syndrome, multiple pterygium syndrome, achondroplasia;
- malformations of the chest cavity (thoracic dysplasia, diaphragmatic hernia, cystic adenomatous lung defect);
- malformations of the urinary system (congenital nephrotic syndrome, urethral and kidney defects);
- cardiovascular pathology (cardiomyopathy, congenital heart defects, anatomical defects, arterial-venous shunts)
- chorioangioma of the placenta;
- in case of multiple pregnancy (feto-fetal transfusion, acardial twins);
- infectious diseases of the mother during pregnancy (cytomegalovirus infection, syphilis, parvovirus infection, toxoplasmosis, Coxsackie viral pancarditis);
- pregnancy complications (preeclampsia, severe anemia, uncorrected diabetes mellitus, hypoproteinemia);
- congenital metabolic disorders (mucopolysaccharidosis type 4, Gaucher disease, neuraminidase deficiency, Morquio disease);
- congenital tumors of the brain and spinal cord, urinary system and digestive tract, liver, sacrococcygeal teratoma, neuroblastoma.
Clinical case of non-immune fetal hydrops with congenital syphilis in a premature newborn
- Kharlamova Natalya Valerievna
- Mezhinsky Semyon Sergeevich
- Ananyeva Maria Alexandrovna
- Chasha Tatyana Valentinovna
- Andreev Artem Vladimirovich
- Shilova Natalia Alexandrovna
Summary We describe a case of non-immune hydrops in a premature baby caused by Treponema pallidum, with clinical manifestations in the form of congenital pneumonia, pleurisy, meningitis, hepatosplenomegaly, thrombocytopenia.
Key words: premature newborn, congenital syphilis, non-immune hydrops fetalis, hepato-splenomegaly, thrombocytopenia
Neonatology: news, opinions, training. 2021. T. 7. No. 1. P. 77-82. DOI: 10.24411/2308-2402-2018-00010
Non-immune hydrops fetalis (NHF) is a heterogeneous pathology, which is usually the final stage in the development of some intrauterine diseases of the fetus and is clinically characterized by signs of severe general hydration caused by extracellular accumulation of fluid in tissues and serous cavities in the absence of signs of immune sensitization [1, 2] .
NVP currently remains a pathology characterized by a fairly high mortality rate, reaching, according to some data, 80-90% [1-3]. The prevalence of NVP varies from 1:1500 to 1:4000 [4].
NVP can occur at different stages of fetal development [1]. In the early stages of pregnancy, the most common causes of NVP are chromosomal aberrations and gene diseases (glucose-6-phosphate dehydrogenase deficiency, homozygous α-thalassemia, Pena-Chockey syndrome, Noonan syndrome, multiple pterygium syndrome, achondrogenesis, achondroplasia, thanatophoric dwarfism, etc.) [5 , 6], congenital malformations (heart defects, diaphragmatic hernia, cystic adenomatous lung defect, malformations of the lymphatic system) [1, 2]. In later stages of pregnancy, the etiological factor of NVP in most cases is infections [1, 2, 7-11]. Up to 20% of cases of NVP are associated with the development of parvovirus B19 infection [12]. In addition, causative microorganisms in relation to NVP are also herpes simplex virus [13], cytomegalovirus [14], as well as the causative agent of syphilis, Treponema pallidum [10, 15-17]. The clinical picture of congenital syphilis can vary from asymptomatic to severe clinical manifestations of the disease, including NVP, severe anemia, hepatosplenomegaly, thrombocytopenia, syphilitic rhinitis, inflammation of internal organs, skeletal lesions and neurosyphilis [10, 15-18].
We present a clinical case of NVP with early congenital syphilis in a premature baby.
Child
M., male, from a 30-year-old mother, a resident of Uzbekistan, was born in the birth block of the obstetric clinic of the Federal State Budgetary Institution “Ivanovo Research Institute named after. V.N. Gorodkov" of the Ministry of Health of Russia at a gestation period of 35 weeks. The woman is currently pregnant for the second time. The woman registered with the antenatal clinic for this pregnancy at 27 weeks (at her place of residence in Uzbekistan). From the anamnesis: chronic diseases include chronic rhinitis, chronic bronchitis. The course of this pregnancy was complicated by an acute respiratory infection at 14 weeks with catarrhal symptoms without fever, and grade I anemia. At 28 weeks, the woman had a positive blood reaction to syphilis (Wassermann reaction ++) without accompanying clinical signs; the woman did not receive treatment. From 32 weeks, the patient was observed at the antenatal clinic in the Ivanovo region, and treatment for syphilis was started at the same time. At 33 weeks, polyhydramnios was diagnosed; ultrasound revealed signs of acute placentitis and intrauterine fetal hydrops. From 34 weeks, increasing polyhydramnios and intrauterine fetal suffering were noted; at 35 weeks, amniotic fluid leaked. Due to prenatal rupture of amniotic fluid and intrauterine suffering of the fetus, a caesarean section was performed at 35 weeks, and a boy weighing 3500 g, length 48 cm, head circumference 32 cm, chest circumference 36 cm was removed. Apgar score was 3/5/6 points.
At birth, the child's condition was assessed as extremely severe in terms of the severity of respiratory failure, edema syndrome, and depression of the central nervous system. Primary resuscitation measures were carried out: radiant heat, sanitation of the upper respiratory tract, tracheal intubation in the 2nd minute of life, artificial pulmonary ventilation (ALV) was started in the controlled forced ventilation mode. The child was transferred to the neonatal intensive care unit (NICU) under conditions of mechanical ventilation and hardware monitoring. Assessment of the child’s physical development using the centile method showed large body weight (body weight exceeded the 90th percentile on the Intergrows scale). Height and head circumference were within normal values.
Upon transfer to the NICU, the condition was assessed as extremely severe, due to severe respiratory failure and hemodynamic instability. The edema syndrome is sharply expressed to the degree of anasarca. Severe indurative edema of subcutaneous fat and subcutaneous small focal hemorrhages in the abdomen and lower extremities are noted. The child’s general reaction to the examination is minimal, muscle tone is significantly reduced, and motor activity is minimal. ADsr. 30 mmHg Palpation of the large fontanel is difficult. Eyes closed. Breathing during mechanical ventilation is sharply weakened in both halves of the chest, and practically cannot be heard on auscultation. Heart sounds are dull, rhythmic, with a tendency to bradycardia (90-120 per minute). The abdomen is sharply increased in volume and tense. Palpation of the liver and spleen is difficult (Fig. 1).
In the NICU, starting from day 1, initial antibacterial therapy was prescribed, taking into account the recommendations of a dermatovenerologist: ceftriaxone + netromycin. Dopamine was prescribed for cardiotonic purposes. After consultation with a pediatric surgeon, under analgesia (fentanyl), puncture and drainage of the abdominal cavity were performed, and a dark yellow content was obtained in a volume of 250 ml. During puncture of the pleural cavities, a small amount of content was obtained (Fig. 2, A, B).
The finding during neurosonography was the detection of an intracerebral hematoma in the left frontal lobe.
After a clinical and instrumental examination, a clinical diagnosis was made: intrauterine infection. Congenital syphilis (?). Non-immune hydrops fetalis (hydrothorax, ascites, edema syndrome). Perinatal damage to the central nervous system (CNS) of mixed etiology. Cerebral ischemia stage III. Intracerebral hematoma in the left frontal lobe. Congenital pneumonia, severe, stage III respiratory failure, pleurisy. Functioning ductus arteriosus (1.5 mm), variable discharge. Open oval window. Hepatosplenomegaly. Prematurity 35 weeks.
General clinical blood tests were performed in the NICU (Tables 1, 2). Features of the first days of life were severe anemia, leukocytosis and thrombocytopenia. The neutrophil index in the first 2 days of life varied from 0.2 to 0.3. The platelet count did not exceed 50 g/l.
On the 2nd day of life, the child’s condition remained the same, still unstable. Mechanical ventilation was performed with the same parameters. Indicators of pH and blood gas composition are compensated. Cardiotonic dopamine support was continued. Given the decrease in blood plasma concentration parameters (Hb 79 g/l), red blood cell transfusion was performed. According to a biochemical blood test, an increase in the levels of transaminases, urea and creatinine, bilirubin and its direct fraction was observed (see Table 2). Due to increasing hyperbilirubinemia, phototherapy was prescribed. A general urine analysis revealed no pathological changes. On the 3rd day of life, the child’s condition was stabilized. Due to persistent severe hypoproteinemia (hypoalbuminemia), an infusion of albumin solution was performed. Given the progressive thrombocytopenia, transfusion of platelet concentrate was prescribed. Subsequently, the condition tended to stabilize; on the 7th day of life, the boy was transferred to an auxiliary mode of mechanical ventilation. On the 10th day of life, due to the appearance of independent adequate breathing in the child, he was extubated and transferred to spontaneous breathing under oxygen therapy through an oxygen mask.
For diagnostic purposes, a magnetic resonance imaging study of the brain was performed (Fig. 3), an intracerebral hematoma was confirmed in the left frontal lobe and the deep substance of the left hemisphere of the brain with a small intrathecal hemorrhage in the left frontal region (probably a hemorrhage with the formation of a hematoma in the area of ischemic damage ). A neurosurgeon was consulted - there are no indications for surgical intervention.
Examination of the cerebrospinal fluid (lumbar puncture) showed the presence of antibodies to
Treponema pallidum
(positive result), signs of inflammatory changes (cytosis 7.2; protein 1.2 g/l). Based on the data obtained, a diagnosis was made: meningitis. PCR diagnostics (DNA) of the cerebrospinal fluid was carried out: HSV I and II - the result is negative, CMV - the result is negative; PCR diagnostics of urine: HSV I and II - negative result, CMV - negative result. The conclusion of a serological blood test using ELISA was obtained: hepatitis HBsAg - negative result, anti-HCV - negative result. The child was consulted by a venereologist and diagnosed with early congenital syphilis with symptoms. A routine X-ray examination of the tubular bones of the lower extremities was performed: no bone-pathological changes were detected.
Further management of the newborn in the NICU was accompanied by a weakening of mechanical ventilation regimens, a change in the course of antibacterial therapy, and an increase in the volume of enteral nutrition.
At the age of 1 month of life, a boy in a serious stable condition weighing 2960 g was transferred to the Department of Pathology of Newborns and Premature Infants (OPNND) of the Federal State Budgetary Institution Ivanovo Research Institute named after. V.N. Gorodkov" of the Russian Ministry of Health with a diagnosis of intrauterine infection. Early congenital syphilis with symptoms (visceral). Nonimmune hydrops fetalis. Polyserositis: bilateral effusion pleurisy, effusion into the abdominal cavity. Condition after laparocentesis, drainage of the abdominal cavity, puncture of the pleural cavities. Congenital pneumonia of unknown etiology, severe course. Respiratory failure stage III. Hepatosplenomegaly. Neonatal cholestasis. Severe anemia of mixed etiology. Thrombocytopenia. Cerebral ischemia stage III. Intracerebral hematoma in the left frontal lobe and deep substance of the left hemisphere of the brain. Inguinal hernia on the right. Prematurity 35 weeks.
In the department of pathology of newborns and premature infants, treatment was continued, including the use of eubiotics (Linex), antihemorrhagic drugs (Vikasol 1%), hepatoprotectors with choleretic effects (Galstena, Ursofalk), and immune drugs (Viferon 1). Despite the treatment, the boy's condition remained stable and serious. Motor activity is moderately reduced. The cry is loud, irritated. There are no meningeal symptoms. Large fontanelle 3x3 cm, not tense. Muscular hypotonia, hyporeflexia. He was fed from a nipple, the sucking was sluggish, he did not get enough nutrition, so he was fed through a tube and absorbed the prescribed amount of food. The skin was pale pink with an earthy tint, jaundice decreased over time, and cyanosis of the nasolabial triangle remained. Oxygen independent. Breathing with the participation of auxiliary muscles, auscultation is better, wheezing in a small amount. Heart sounds are muffled, rhythmic, systolic murmur. The abdomen is enlarged, soft, painless. Liver +5 cm, spleen +7.5 cm. Inguinal hernia on the right, without signs of strangulation. The chair is yellow. Urine is straw-yellow.
The child was kept in the OPNND until he was 45 days old, after which, due to the planned closure of the institute’s clinic, he was transferred for further treatment to the Ivanovo Regional Children’s Clinical Hospital. At the age of 2 months, the child was operated on for a strangulated inguinal hernia; the operation went without complications.
Currently, the boy is being monitored on an outpatient basis at a children's clinic at his place of temporary residence (Ivanovo region). The dynamics of the child's condition are positive.
Thus, the clinical picture of congenital syphilis in the classical description is quite rare. The symptoms of this infection in newborns are varied and often nonspecific; they can also occur with other diseases. When a child is born with NVP, it is first necessary to suspect chromosomal or gene diseases, congenital malformations, as well as intrauterine infections, among the most significant pathogens of which are parvovirus B19, cytomegalovirus, herpes simplex virus, and treponema pallidum. Much attention must be paid to the prevention of intrauterine infections, timely detection and treatment of infected pregnant women, since the clinical manifestations of intrauterine infection in a newborn, especially NVP, can determine the unfavorable outcome of the disease.
LITERATURE
1. Kurtser M.A., Gnetetskaya V.A., Malmberg O.L., Belkovskaya M.E. and others. Non-immune fetal hydrops: diagnosis and tactics // Obstetrics. and gin. 2009. No. 2. P. 37-40.
2. Kuznetsov P.A., Kozlov P.V., Dzhokhadze L.S., Konstantinova K.I. Non-immune hydrops of one fetus from twins (clinical observation) // Vestn. Ross. state honey. un-ta. 2014. No. 4. P. 42-44.
3. Vorobyova O.V., Levchenko L.A., Markosyan K.A., Podolyaka V.L. and others. Non-immune hydrops fetalis (clinical case) // Ukrainian Medical Almanac. 2011. T. 14, No. 1. P. 49-51.
4. Henrich W., Heeger J., Schmider A. et al. CompLete spontaneous resolution of severe nonimmunoLogicaL hydrops fetaLis with unknown etioLogy in the second trimester - a case report // J. Perinat. Med. 2005. VoL. 30, N 6. P. 522-527.
5. Sohan K., CarroLL SG, De La Fuente S., SoothiLL P. et al. AnaLysis of outcome in hydrops fetaLis in reLation to gestationL age at diagnosis, cause and treatment // Acta Obstet. GynecoL. Scand. 2001. VoL. 80. P. 726-730.
6. Crow Y., Hayward B., Parmar R. et al. Mutations in the gene encoding the 3′-5′ DNA exonucLease TREX1 cause Aicardi-Goutieres syndrome at the AGS1 Locus // Nat. Genet. 2006. VoL. 38, N 8. P. 917-920.
7. Kolobov A.V., Karev V.E., Vorobtsova I.N., Orel V.I. Non-immune fetal edema during intrauterine infection // Journal. infectology. 2013. T. 5, No. 2. P. 109-112.
8. Syridou G., Skevaki C., Kafetzis DA Intrauterine infection with parvovirus B19 and CMV: implications in earLy and Late gestation fetaL demise // Expert Rev. Anti Infect. Ther. 2005. VoL. 3, N 4. P. 651-661.
9. KuhL PG, ULmer HE, Schmidt W., WiLLe L. Non-immunoLogic hydrops fetaLis report of 14 cases and Literature review // KLin. Padiatr. 1985. VoL. 197, N 4. P. 282-287.
10. McCauLey M., van den Broek N. ELiminating congenitaL syphiLis-Lessons Learnt in the United Kingdom shouLd inform gLobaL strategy // BJOG. 2021. VoL. 124, N 1. P. 78.
11. Syrneva T.A., Malishevskaya N.P., Makarenko A.V. Clinical and epidemiological aspects of congenital syphilis in Russia // Ros. magazine leather and veins bol. 2015. T. 18, No. 2. P. 57-60.
12. Essary LR et aL. Frequency of parvovirus B19 infection in nonimmune hydrops fetaLis and utiLity of three diagnostic methods // Hum. PathoL. 1998. VoL. 29, N 7. P. 696-701.
13. Dubois-Lebbe C., HouffLin-Debarge V., DewiLde A., Devisme L. et al. Nonimmune hydrops fetaLis due to herpes simpLex virus type 1 // Prenat. Diagn. 2007. VoL. 27. P. 188-189.
14. Matyskina N.V., Taranushenko T.E., Prokhorenkov V.I. Early congenital syphilis: clinical and laboratory features in the neonatal period // Children's infections. 2015. T. 14, No. 1. P. 43-46.
15. Askhakov M. S. Congenital syphilis // Vestn. young scientist. 2021. T. 15, No. 4. P. 46-52.
16. Malinnikova E.Yu., Amon E.P., Rakova N.G. Problems of diagnosing intrauterine and congenital infections from the position of clinicians and doctors of clinical diagnostic laboratories // Med. alphabet. 2021. T. 2, No. 13. P. 53-57.
17. Okeke TC, Egbugara MN, Ezenyeaku CC, Ikeako LC Non-immunehydropsfetaLis // Niger. J. Med. 2013. VoL. 22, N 4. P. 266-273.
Diagnostics
Diagnosis of fetal hydrops is aimed at establishing the cause that caused it. First of all, the blood type and Rh factor are determined to confirm/exclude Rh conflict and immune fetal hydrops.
An analysis is carried out of the life history (infectious diseases in the past, operations, chronic pathology), obstetric and gynecological history (the presence of gynecological pathologies, the course and outcomes of previous pregnancies), the course of the current pregnancy, its complications, general weight gain, etc. is analyzed.
The main diagnostic method is fetal ultrasound. Ultrasound signs include:
- swelling of the placenta (“thick placenta”);
- excess amniotic fluid (polyhydramnios);
- the size of the fetus is larger than normal due to edema (in particular, increased size of the abdomen due to ascites compared to the size of the head);
- accumulation of fluid in all cavities of the fruiting body (hydropericardium, ascites, hydrothorax)
- swelling of the subcutaneous fat layer in the form of a double contour;
- swelling of the scalp, arms and legs;
- cardiomegaly (increase in heart size);
- thickening of the intestine (swelling of the walls);
- enlargement of the liver and spleen (hepatosplenomegaly)
- “Buddha pose” - a swollen abdomen with the limbs and spine removed from it;
- low motor activity in combination with other signs.
After an ultrasound, amnio- or cordocentesis is prescribed to determine the fetal karyotype, obtain fetal blood (assessment of hemoglobin, protein) and possible intrauterine treatment. In order to exclude intrauterine infection, PCR testing for suspected infections is prescribed.
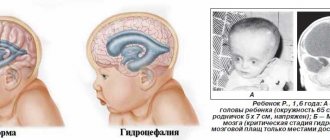
Can hydrocephalus be cured?
Modern methods make it possible to normalize the outflow of cerebrospinal fluid from a congested brain or spinal cord by installing shunts - tubes that drain cerebrospinal fluid. Sometimes, with a mild form of the disease, this is enough to preserve the child’s intelligence. However, such a child will have to be home schooled, because... a minor head injury, which he easily receives at school, can be fatal. Such children also do not attend preschool institutions.
But in severe forms of the disease, manifested by a significant increase in head size, especially when combined with other developmental defects, the child’s physical and mental development inevitably suffers.
The growth of the head progresses after birth and it becomes very large with protruding external saphenous veins. Such children often have profound disabilities and cannot even care for themselves.
The most dangerous situation is when, already in utero, the child receives severe brain damage caused by increased intracerebral division. Children often suffer from visual impairment, hearing impairment, cerebral palsy, convulsive seizures, epilepsy, and attacks of uncontrollable headaches accompanied by vomiting. Most children, except those suffering from a mild form of hydrocephalus and receiving timely treatment, die before the age of 10 years.
Of course, the question of whether or not to leave a child with hydrocephalus depends on the degree of manifestation of the pathology, so the doctor, during an ultrasound of the fetus, will tell you what problems may arise and whether there is a chance for treatment and rehabilitation.
In the future, everything depends on the principles and financial capabilities of the family, because the treatment and recovery of such a child is expensive and not always promising. If the doctor insists on terminating the pregnancy, it is better to agree with him.
It is not uncommon for the birth of such a child to destroy a family. As a result, by the age of 6-10, the sick child still died, but at the same time other children suffered, deprived of the care and attention of parents who were fully occupied with caring for a child with a high degree of disability.
Treatment of hydrops fetalis
If congenital malformations of the fetus are detected that are incompatible with life (1-2 trimester of pregnancy), the woman is offered termination of pregnancy. If termination is refused, the course of pregnancy and the development of the disease continue to be monitored until the time period allows for prenatal (prenatal) therapy.
Treatment of fetal hydrops consists of cordocentesis and blood transfusion into the umbilical cord (in case of severe anemia and a decrease in hematocrit to 30 or below). If necessary, replacement blood transfusion is repeated after 2-3 weeks.
If feto-fetal transfusion of twins is detected, laser coagulation of the vessels connecting the fetuses is performed. If it is not possible to carry out prenatal treatment, the degree of risk of premature birth in relation to antenatal fetal death is assessed and delivery is carried out ahead of schedule with the preliminary prescription of drugs to accelerate the maturation of the fetal lungs. In some cases, maternal administration of cardiac glycosides is indicated to normalize fetal cardiac activity.
Before delivery (it usually occurs as planned), preparations are made for the birth of a child with dropsy. The delivery room must be equipped with equipment for cardiopulmonary resuscitation; a resuscitation team of 2-3 resuscitators and 2-3 neonatologists is formed (after the birth of the child, the child is immediately intubated and artificial ventilation is carried out with 100% oxygen).
Immediately after birth and resuscitation measures, pericardiocentesis (removal of accumulated fluid by puncture of the pericardial sac), pleural puncture (removal of fluid from the pleural cavity) and laparocentesis (suction of fluid from the abdominal cavity) are performed. A catheter is inserted into the umbilical artery for subsequent infusions of red blood cells or blood.
How often should you have an ultrasound during pregnancy?
The standard number of procedures is 2-3, but in some cases the patient has to visit the diagnostic room several times a month. These are women who are at risk due to the high likelihood of developing abnormalities in the fetus. People in this category include:
- over 35 years old;
- having children with congenital pathologies;
- with a family history;
- exposed to radiation, in contact with toxic substances;
- having a history of premature birth, cases of stillbirth or fetal death in the womb, miscarriages.
Do not be alarmed if the doctor prescribes an additional ultrasound - careful monitoring of the condition of the fetus allows you to avoid congenital pathologies and notice deviations from the norm in the early stages.
Forecasts
The prognosis for non-immune fetal hydrops is unfavorable and the percentage of surviving children is 20-33%. When dropsy develops in the first trimester, pregnancy usually ends in spontaneous abortion; in the second and third trimesters, the risk of antenatal fetal death is high.
With immune dropsy, the prognosis is more comforting; the effect of prenatal and postnatal treatment reaches 80-90%.
Some studies during pregnancy
- Smears during pregnancy
- Pregnancy tests by trimester
- Ultrasound during pregnancy
- General urine test during pregnancy
- Coagulogram
- Installation of a pessary
- Glucose tolerance test
- Homocysteine during pregnancy
- Amniocentesis
- Anesthesia during childbirth
- Fetal CTG (cardiotocography)
- Cordocentesis
- Epidural anesthesia during childbirth
Causes of congenital fetal pathology
What factors can adversely affect the fetus? The causes of various pathologies are:
- burdened heredity;
- Mom's age is over 35 years, dad's age is over 40;
- unfavorable environmental conditions;
- working with toxic substances;
- bad habits - alcohol abuse, smoking, drug use;
- viral and bacterial diseases, especially in the first trimester - influenza, rubella, toxoplasmosis, hepatitis B, sexually transmitted diseases;
- taking certain medications;
- excessive psycho-emotional stress.
The more factors are present, the greater the likelihood of fetal pathologies. That is why you need to start planning for the birth of a child in advance, at least six months before conception. This time is enough to undergo a comprehensive examination, identify and cure diseases, and prepare for the conception of a healthy baby. To highlight the impact of bad habits on the fetus, we present some numbers.
With maternal alcoholism, toxicosis is observed in 26% of cases, antenatal death and asphyxia in 12%, miscarriages in 22%, premature birth in 34%, birth injuries in 8%, and intrauterine growth retardation in 19%.