What is lumbodynia
Pain with lumbodynia can be chronic or acute/subacute, but in any case it is caused by spinal pathology. Lumbodynia syndrome is considered a sign of osteochondrosis of the lumbar spine, although often with this diagnosis there may be no pain at all. The severity of pain can vary and depends on the individual and a combination of a number of factors. It occurs mainly in people of working age (25-45 years).
Lumbar pain can be localized only on one side or on both (right-sided, left-sided, symmetrical). It most often worries in the lower lumbar region and can radiate to the gluteal region (one or both buttocks).
Kinds
Vertebrogenic lumbodynia is the main manifestation of the chronic form of osteochondrosis (lumbar zone) and is more often characteristic of men. Can have any duration (last from several weeks/months to several years). If the cause of pain is diseases of the intervertebral disc (herniation, protrusion), then lumbodynia is called discogenic.
In addition to the above, “classic” one, there are other types. It can be combined with nagging pain in one or both legs (sciatica), in which case it is called lumboischialgia. (left-handed or right-handed). Depending on the distribution (on one or both limbs). Accompanies the non-radicular phase of lumbar osteochondrosis.
When the pain is intensified not only by movements, but even by the slightest activity, such as talking, sneezing, bending over, then this type is called lumbodynia with muscular-tonic syndrome. Often, there is a moderate curvature of the spine, causing pronounced reflex tension in the lower back muscles (bilateral or unilateral), which provokes pain.
Lumbodynia can turn into radiculitis (radiculopathy)
After some time, lumbodynia, if no measures are taken, may give way to the next, radicular stage of spinal osteochondrosis - radiculitis (radiculopathy). As a rule, radiculitis is caused by compression of the nerve root by an enlarged herniated intervertebral disc. In Latin, the spine is radicula (radicula).
Severe, persistent lumbodynia on the right or lumbodynia on the left occurs, depending on which side the nerve root is compressed. Radiculopathy is more difficult to treat and takes longer. The help of a neurosurgeon is often required.
Causes of lumbodynia
Low back pain (lumbodynia), both chronic and acute, is most often caused by pathological processes (degenerative-dystrophic) in the spine, especially in the lumbar region. In addition to osteochondrosis, lumbodynia is caused by its complications, such as protrusion, spondylolisthesis, intervertebral hernia, spondyloarthrosis, spondylosis.
The mechanism of lumbodynia is based on irritation of the nerves (especially sinuvertebral). Pain is especially pronounced with cracks in the fibrous ring. Also the cause is abnormalities in the development of the lumbar spine.
Pain can occur after a single physical overload, lower back injuries, hypothermia, stress, sudden turns of the body, hypothermia, exposure to drafts, prolonged exposure to an uncomfortable or monotonous position. Moreover, lumbodynia can manifest itself not only after a few days or weeks, but even several months after the provoking factor.
The risk group also includes those who are overweight, have certain chronic diseases, have infectious diseases, workers in hazardous industries, those who experience increased stress, lead an adynamic lifestyle, or are in an uncomfortable or the same body position for a long time.
How does chronic vertebrogenic lumbodynia occur?
Low back pain with osteochondrosis is characterized by periods of remissions and exacerbations. Sometimes remissions are quite long, several years. It may seem that recovery has arrived. However, real recovery is not always observed. If the spine continues to work incorrectly, with overload in the lumbar region, then the overloaded intervertebral disc continues to collapse. And if there were no protrusions and hernias, then they may well appear. And if they already existed, then their size may increase. And lower back pain in such situations tends to get worse.
Causes of exacerbation of vertebrogenic lumbodynia
Intensification or recurrence of pain occurs under the influence of various mechanical and traumatic factors, hypothermia, and stress. The proportion of hypothermia as a factor provoking exacerbation of lumbodynia is significantly greater than the causes of the primary occurrence.
Pathological processes occurring outside the spine can affect both the reactivity of the body in general and the course of lumbar osteochondrosis in particular. Chronic somatic diseases and foci of local infection aggravate the manifestations of both lumbodynia and other clinical syndromes of lumbar osteochondrosis.
With the development of osteochondrosis, the formation of protrusions and herniations of spinal discs, endocrine pathology plays an important role. These are diseases of the thyroid and parathyroid glands, adrenal glands and progressive diabetes mellitus.
Symptoms
With vertebral osteochondrosis, lumbodynia is aching in nature and is more pronounced in the morning. May have different durations, decrease or increase during the day. There are provoking factors that increase or decrease the intensity of lumbodynia. For some it is caused by activity, while for others it is its absence; accordingly, opposite actions ease the pain. A combination of these manifestations may occur in the same person.
Pressure on the vertebrae and paravertebral areas in the lumbar area is usually painful. In addition, bending and many other movements are difficult and most often accompanied by pain. Patients have difficulty bending, especially forward, and the angle of inclination of the torso becomes limited. There may be sharp pain in response to palpation of the exit point of the sciatic nerve on the thigh.
Doctors explain the subsidence of pain in the lying position by reducing the load on the lumbar intervertebral discs. Patients intuitively or consciously find the most comfortable position (in which the pain is least pronounced). Most often, this is a position lying on your side with your legs bent.
At first, there is moderate lumbodynia, gradually the pain intensifies, but does not reach the same degree of severity as with lumbar pain (lumbago), also called acute lumbodynia. Patients can move around and do work, but the quality of life is significantly reduced.
Treatment
This disease should be treated by a neurologist. Medicinal methods of influence should be used in combination with local, manual, physiotherapeutic methods of treatment and physical therapy.
The primary task is to relieve the inflammatory process and reduce pain. To do this, they most often resort to non-steroidal anti-inflammatory drugs (diclofenac, meloxicam, etc.). In the first days, it is preferable to use injectable forms of drugs. Typically, anti-inflammatory therapy lasts 5-15 days; if pain persists, they resort to central anesthesia (use drugs catadolone, tebantine, antiepileptic drugs such as finlepsin, lyrica).
You should also reduce the degree of muscle tension, either with the help of muscle relaxants, or, with mild and moderate manifestations, with local remedies, massage and exercise therapy. Various anti-inflammatory and warming ointments, gels, and patches are used as local remedies. You can also make compresses with liquid dosage forms (for example, compresses with dimexide).
Massage for vertebrogenic lumbodynia should be performed in courses of at least 7-10 procedures. The first three to four sessions may be painful; in subsequent sessions, as well as in cases of severe pain, massage should not be performed. The massage begins with stroking movements, which are then alternated with other massage techniques - such as rubbing, vibration, kneading. Massage is contraindicated in the presence of gynecological pathology, oncopathology (including a history), and skin diseases.
From physical influences, as with other problems with the spine, diadynamic currents should be used, as well as electrophoresis in the acute period, and magnetic fields and laser radiation as a preventive treatment.
Physical therapy exercises for vertebrogenic lumbodynia play a vital role. In addition to relieving and distracting pain during the acute period through stretching exercises, they lead to a number of therapeutic effects. Firstly, this concerns strengthening the muscle corset and thereby reducing the load directly on the vertebrae. Secondly, nutrition of intervertebral structures and microcirculation through the ligamentous apparatus improves. Exercises should be performed regularly, ideally throughout your life.
Diagnosis of lumbodynia
Lumbodynia can be diagnosed in different ways. A neurologist diagnoses this disease. The most common is a clinical examination and questioning of the patient, combined with static and dynamic examination of the spine, as well as manual diagnostics. Additionally, the organs of the pelvic and abdominal cavities are examined to exclude diseases that are a source of referred pain. In addition, MRI, radiography, and ultrasound diagnostics will not be superfluous. During the examination, lumbodynia is differentiated from myositis of the spinal muscles and pathologies of the hip joint.
IMPORTANT! Lumbodynia is a serious symptom that can tell a person about significant problems in the lumbar spine, ranging from inflammatory phenomena to destructive diseases. That is why, if you have lumbodynia, you cannot self-medicate, but you should definitely consult a specialist!
Experienced doctors at the Kuntsevo Medical and Rehabilitation Center will conduct a thorough diagnosis and understand the causes of the symptom. A treatment plan for the patient will then be drawn up. Make an appointment with our doctor and take a step towards getting rid of lumbodynia!
Sign up
Prevention
Prevention of lumbodynia consists of observing the following rules:
- proper organization of the workplace;
- maintaining an active lifestyle, playing sports;
- avoiding hypothermia;
- sleeping on your side with a properly selected pillow;
- regular swimming lessons;
- correct load distribution when lifting and carrying heavy objects;
- refusal of high-heeled shoes;
- balanced diet;
- timely seeking medical help when the first signs of lumbodynia appear.
Treatment of lumbodynia at the CELT Pain Clinic returns freedom of movement to our patients!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Treatment with manual therapy
You can get rid of lumbodynia only by eliminating the causes that caused it. This type of treatment can be considered complete. In other cases, the help will have a temporary effect and after some time, lumbodynia will appear again, and if the treatment was inadequate, it will intensify or recur. It is important to find a good chiropractor, otherwise you may not only not be cured, but even make things worse.
Since the main cause of lumbodynia is considered to be vertebral osteochondrosis, the cause of which, in turn, is improper functioning of the spine, it is not lumbodynia that should be treated, but osteochondrosis. In addition, by getting rid of osteochondrosis, you will protect yourself from the occurrence of its complications, such as hernias and disc protrusions.
Manual therapy is considered one of the most effective ways to eliminate problems in the spine. It is especially effective in combination with the subsequent implementation of a complex of physical therapy (physical therapy). All this not only improves the condition, but also stimulates recovery processes, thanks to which the course of the disease can sometimes not only be stopped, but also reversed.
The number of procedures is prescribed individually, based on the patient’s health characteristics, stage of the process, complications, and concomitant diseases. It is also necessary to perform exercise therapy to consolidate the achieved result and maintain it after treatment.
Mechanisms of pain syndrome formation in the lumbar spine
The anatomical structures that form the spinal motion segment can be involved in the pain syndrome in different ways; pathological processes manifest themselves separately or in combination.
Vertebra
Its most sensitive part is the periosteum. On the other hand, internal bone tissue provides less accurate information about pain, so intraosseous tumors may be asymptomatic or give vague symptoms.
Joints
Intervertebral joint pain occurs only when mechanical stress is transmitted to adjacent structures. Deformations and cracks of the intervertebral disc themselves do not cause pain, because it has no nerve endings, but the vertebrae, the ligamentous apparatus of the vertebral segment, are innervated by branches of the spinal root and any pressure from a deformed or displaced disc will inevitably provoke pain.
A deformed disc (for example, due to osteochondrosis) is less able to absorb mechanical stresses acting on it, increasing the load on the richly innervated facet joints. Thus, pain can be caused by inflammation of mechanical origin - from overload or increased pressure on these joints, or their displacement, misalignment, when the facet joints are no longer parallel. Hyperlordosis, spinal curvature due to spondyloarthritis, and facet joint osteoarthritis cause pain in the same way.
Ligaments
Pressure on the posterior longitudinal ligament produces pain, often due to a herniation or protrusion, usually of the central or centrolateral type, convexing posteriorly.
Nerve roots
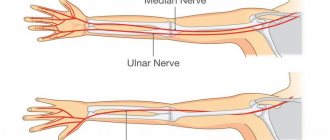
They make up the lumbosacral plexus and the sciatic nerve (L4-L5-S1-S2-S3). Its compression can lead to severe pain - sciatica. The pain “radiates”, passes along the sciatic nerve, through the buttocks and thighs (signs of irritation of the roots), sometimes paresthesia appears. When the compression is significant or persistent, symptoms of neurological deficits, hypo- or areflexia, and paresis occur.
Muscles and fascia
can cause severe dull pain. Pain from the joints of the spine and lumbosacral ligaments causes a reflex spasm of the posterior muscles of the spine, which, in turn, aggravates the condition of the joints.