Osteochondrosis is a chronic degenerative dystrophic disease in which gradual destruction of the cartilage tissue of the intervertebral discs occurs. They lose their elasticity and shock-absorbing ability, and stop protecting the radicular nerves extending from the spinal cord from compression. A decrease in the height of the intervertebral discs leads to instability of the position of the vertebral bodies, their constant displacement, which can cause the development of spinal canal stenosis.
Strain syndrome is excessive tension of the muscle fibers in the area of the affected area of the spinal column. In this way, the body tries to compensate for the decrease in the height of the intervertebral disc and eliminate compression from the radicular nerve. These signs are important in the differential diagnosis of osteochondrosis with other possible pathologies.
Tension syndrome in osteochondrosis helps the neurologist to clarify the degree of damage to the cartilage tissue of the disc and compression of the radicular nerve. There are several symptoms of tension: Lasegue, Neri, Matskevich, Vaserman, Sekar, Bekhterev and Dejerine. We will examine some of them in detail in the proposed material.
If you find at least one of them in yourself, then do not hesitate to contact a neurologist. Such a manifestation indicates that there is serious damage to the nerve fiber. Without timely treatment, this condition can provoke atrophy of the radicular nerve and trigger a cascade process of innervation disruption. In this case, not only the muscles of the back frame can be damaged, but also the lower limbs, vascular bed, and internal organs of the abdominal cavity and pelvis.
If you have symptoms of tension, then in Moscow you can make an appointment with a neurologist at our manual therapy clinic. The initial appointment is free for each patient. During the consultation, an experienced doctor will check whether you really have a positive symptom of tension due to osteochondrosis. Once an accurate diagnosis is made, an individual treatment plan will be developed.
Positive symptoms of tension in neurology
Let's look at some symptoms of tension in neurology. The most common symptom of root tension is Lasegue's syndrome. It indicates an ongoing muscle spasm that accompanies vertebrogenic pain syndrome. The nerve roots are blocked by spasmed muscles. When making sudden movements of the leg or body with a positive Lasegue tension symptom, a nerve fiber may rupture. Therefore, the patient is shown bed rest and complete physical rest until the muscle spasm passes.
Bilateral symptoms of tension in neurology with osteochondrosis appear when large nerves responsible for the innervation of the lower extremities are damaged. For example, bilateral Lassègue's syndrome may be present with sciatica (inflammation of the sciatic nerve). The same sign may indicate piriformis syndrome, plexopathy of the lumbosacral and coccygeal nerve plexuses.
With positive Lasegue syndrome in osteochondrosis, the following clinical signs are present:
- when trying to raise the upper leg on the side of the lesion of the radicular nerves, the patient experiences a severe exacerbation of the pain syndrome;
- when the position of the body in space changes, a sensation of pulsation occurs in the leg, associated with compression of a large nerve;
- there is no possibility to move the leg freely in the lateral direction.
When determining Lasègue tension syndrome, the physician must determine at what angle the patient can lift the leg upward. The condition of the limb in a flexed state is also assessed. If the pain when bending the knee joint decreases, this indicates that the symptom is positive.
Study design
The clinical study lasted 3 months. All patients participating in the study were divided into 2 groups comparable in age, duration of the disease, clinical-neurological status: Group I (20 people)
- patients with clinical manifestations of vertebrogenic lumbar sciatica with neurovascular syndrome who received treatment from the physiotherapeutic device "POLIMAG-01" using external tape inductors for the lumbar region and lower limbs.
Group II (20 people)
— patients with clinical manifestations of vertebrogenic lumboischialgia with neurovascular syndrome who did not receive treatment procedures for the lumbar region and lower extremities (control group).
During the observation period, patients received basic treatment
The procedures were carried out against the background of basic treatment, including therapeutic exercises, swimming in the pool, and iodine-bromine baths. Vascular medications were not used during the study period.
Symptoms of tension in lumbar osteochondrosis
Let's consider other symptoms of tension in lumbar osteochondrosis, one of which is called planting syndrome. It indicates the etiology of pain in the spinal column. It can also be used to assess the condition of the radicular nerves. In order to evaluate the symptoms of tension in osteochondrosis of the lumbar region, it is necessary:
- ask the patient to take off his shoes and sit on the couch so that his back is tilted back and his legs remain straight and parallel to the floor;
- the patient should remain in this reclining state for approximately 20–30 seconds;
- the appearance of complaints of acute pain in the knee joint and falling on the back due to exceeding the pain threshold in the lumbar spine indicates that the landing syndrome is positive.
While the patient is in a reclining position on the couch, it is important to conduct a palpation examination of the area in which pain is detected. Reflex tension in certain areas of the muscular frame of the back and lower back indicates that destruction of individual intervertebral discs has occurred.
In the event that the patient can remain in a reclining position with straightened legs for a long time, the diagnosis of lumboischialgia is not confirmed. You should look for the cause of pain in other parts of the musculoskeletal system. Most often this is deforming osteoarthritis of the iliosacral joints or spondyloarthrosis of the coccygeal-sacral joint. With these pathologies, tension syndromes remain negative.
Back pain, its etiology and treatment is a problem of modern medicine, which has been repeatedly raised in scientific publications, speeches and discussions. However, despite many years of close attention to this therapeutic problem, its unambiguous solution has not been found. It must be recognized that progress in this area is still being observed - works appear [1, 2] describing the mechanisms of occurrence and consolidation of myofascial syndromes, anatomical, physiological and social features leading to an increase in morbidity are being studied, and non-drug methods of pain relief are being actively introduced. Nevertheless, the deeper the understanding of the pathophysiological processes leading to the occurrence of algic disorders becomes, the more questions specialists have. At the moment, there is not even a unity of terminology used to describe this pathological condition. The actively used terms “dorsopathy” and “dorsalgia” are a universal description of any process hidden behind the pain syndrome. At the same time, the variety of factors causing the occurrence of pain undoubtedly requires completely different therapeutic approaches, which leads to misunderstanding and lack of opportunity to streamline and standardize, as necessary, the process of diagnosing and treating back pain [3]. Thus, pain syndromes can occur with myofascial and myotonic disorders caused by a violation of the biomechanics of the motor act. In this case, the greatest attention should be paid to visual optical diagnostics and manual muscle testing, and the role of neuroimaging is secondary and optional [4]. However, often the source of pain impulses can be located in the system of the spinal motion segment and be associated with changes in the spinal column itself and nearby large joints. In this case, the therapeutic strategy should be aimed at identifying these changes and carrying out pharmacological and non-pharmacological correction of these factors [5, 6].
Thus, by now there is a need not only to change the concept of diagnostic and therapeutic methods, but also to develop terminological unity. This will make it possible to create unified methodological approaches to the treatment of pain syndromes in the back, streamline the work of specialists dealing with this problem, and, as the authors hope, will lead, as the authors hope, to a decrease in the percentage of chronicity of the disease.
Developing a treatment plan for back pain is a rather complex therapeutic task, since the disease is accompanied by a number of comorbid and concomitant disorders. One of the most common phenomena accompanying back pain is compression-ischemic neuropathies, which is not accidental - the restructuring of the motor stereotype, leading to the appearance of myotonic reactions in the back, is not an isolated process, but, as a rule, affects all parts of the motor system . Muscle spasm that occurs in the back area contributes to the restructuring of the biomechanics of all muscles involved in the act of movement. In addition, the provoking factors themselves, such as hypothermia, prolonged stay in a non-physiological position, physical inactivity, are often universal triggers leading to spasms and changes in the anatomical and topographic connections of the muscles and neurovascular bundles of the torso and limbs. Thus, it seems relevant to analyze certain types of compression-ischemic neuropathies and methods of their treatment [7, 8].
Compression-ischemic neuropathy of the sciatic nerve, or piriformis syndrome.
This type of neuropathy is caused by pinching of the sciatic nerve by a spasmed piriformis muscle. The high prevalence of the syndrome and the difficulties of its diagnosis are associated with the anatomical features of the structure of the sciatic region: the piriformis muscle has a triangular shape and is attached at one apex to the greater trochanter, then passes through the greater sciatic foramen and is attached in three uniform bundles to the sacrum, between the first and fourth sacral foramina. The capsule of the sacroiliac joint remains above the muscle, and below the muscle is the anterior surface of the sacrotuberous ligament. A bundle of blood vessels and the sciatic nerve pass through the sciatic foramen with the muscle. In this case, there are various topographic options for the location of the sciatic nerve trunk. Most often it is located under the piriformis muscle, but in some cases it can spread over the muscle or pass inside the muscle bundle. The latter option is most often accompanied by pronounced pain syndromes. The piriformis muscle is involved in a large number of movements: external rotation of the hip; bending forward with fixed and motionless lower limbs; stabilization of the hip joint and retention of the femoral head. Spasm leads to shortening and tightening of muscle fibers, which limits the rotational movements of the hip, as a result of which pain spreads to the groin area, along the leg to the knee, and to the lumbar region.
Clinically, piriformis syndrome is manifested by pain sensations both local and along the compressed sciatic nerve. Localization of pain in the gluteal muscle area is often accompanied by pain radiating not only to the leg, but also to the lower back, which forces patients to describe their sensations as back pain and complicates diagnosis. Algic phenomena in this case intensify with movements involving the piriformis muscle; the pain is neuropathic in nature and is accompanied by numbness, paresthesia, and burning in the area innervated by the sciatic nerve or its branches. With a significant degree of compression of the sciatic nerve trunk and involvement of the vascular bundle, manifestations of motor or autonomic-trophic dysfunction are also possible.
When a patient presents with such complaints, in addition to a traditional neurological examination, which allows identifying sensory or reflex disorders in the area of innervation of the sciatic nerve or its branches, it is necessary to palpate the attachment points of the piriformis muscle (the area of the greater trochanter of the femur and the sacroiliac joint), which will sharply painful. Dynamic testing of the condition of the iliosacral and sacrospinous ligaments is also recommended.
However, neuroimaging methods are able to identify only the primary factor in the secondary involvement of the piriformis muscle, and the appointment of an x-ray or magnetic resonance examination only leads to diagnostic inaccuracies, since in most cases it reveals degenerative-dystrophic changes in the spine of varying severity.
To confirm the diagnosis of piriformis muscle syndrome, several diagnostic tests are used, including Bonnet-Bobrovnikova's symptom (palpation of the spasmodic piriformis muscle), Vilenkin's symptom (sharp pain on percussion of the projection area of the piriformis muscle), Grossman's symptom (unilateral or bilateral contraction of the piriformis muscle during percussion lower lumbar or sacral vertebrae).
The concomitant ischemic nature of the lesion can be assumed using the limb elevation test, when the patient, in a supine position, lifts first one and then the other leg. The test can be considered positive if it is possible to reproduce sensory phenomena in the form of the appearance or intensification of numbness, paresthesia, and pallor of the extremities. A patient may complain of similar symptoms when he has to stop while walking due to unpleasant sensations that occur after a short rest.
Compressive neuropathy of the ilioinguinal nerve.
The nerve can be pinched during sudden abdominal tension, for example when lifting or holding heavy objects, due to the displacement of muscle layers that deform the nerve trunk. This type of neuropathy is more common in men in whom the sensory branch of the ilioinguinal nerve reaches the base of the scrotum, exits through the outer ring of the inguinal canal and adjacent parts of the thigh. Much less frequently, this syndrome is observed in women; in this case, the inguinal branch exits in the area of the uterine ligament and ends in the area of the labia majora.
Compression of the ilioinguinal nerve also often occurs after or during operations for inguinal hernias, appendicitis and during nephrectomy, when the nerve trunk is compressed by adhesive scars or gets caught in a suture when suturing the abdominal wall. The most common symptom of neuropathy is pain in the groin area, often radiating to the upper inner thigh. With abdominal tension and hip extension in the hip joint, the pain intensifies, and with flexion and internal rotation of the hip, it decreases or goes away. Here hyperesthesia or hypoesthesia is sometimes detected. Upon palpation and percussion, a limited area of sharp pain is determined, localized medially from the anterior superior iliac spine. This painful area corresponds to the passage of the sensory branch of the ilioinguinal nerve through the external abdominal muscle. In some cases, weakness of the abdominal muscles is detected in the hypogastric region, manifested by protrusion of the latter when the abdominal tension is tense.
Compression-ischemic neuropathy of the femoral nerve.
This nerve is mixed, its muscle branches innervate the iliopsoas muscle and the quadriceps femoris muscle; the area of skin innervation is the anterior and medial surface of the thigh, leg and foot, almost up to the first finger. Thus, symptoms of neuropathy include both sensory and movement disorders. The femoral nerve originates in the lumbar plexus and exits the pelvic cavity under the inguinal ligament between the psoas major and iliacus muscles, being fixed to their fascia. Accordingly, any pathological processes in the area of these muscles can cause damage to the femoral nerve. The most common cause of femoral nerve neuropathy is trauma followed by the formation of a paraneural hematoma or other pathological processes in the hip joint. Rare, but much more unfavorable prognostically, causes of compression of the femoral nerve can be tumors, abscesses and hematomas of the retroperitoneal space. A typical site of compression of the femoral nerve is the area behind the inguinal ligament, where the nerve from the retroperitoneum exits the thigh in close proximity to the hip joint capsule. With compression-ischemic neuropathy, spontaneous pain can sometimes be very intense. Patients with this syndrome can stand and walk freely, but experience severe difficulty going up and down stairs. More often, patients complain of pain under the inguinal ligament with irradiation to the anterior and inner surface of the thigh, the inner surface of the leg and foot. With prolonged disease, hypalgesia occurs in the area of innervation of the femoral nerve. Motor disorders manifest themselves in the inability to straighten the leg at the knee joint and weakened hip flexion. A neurological examination in such cases reveals the absence of a knee reflex, hypoesthesia of the skin of the anterior surface of the thigh and the inner surface of the leg, and with a long course - atrophy of the quadriceps muscle. Characteristic symptoms of tension are Wasserman and Matskevich. Pain is observed when pressing on the nerve in the upper third of the thigh, under the inguinal fold, or when pressing on the muscles of the anterior surface of the thigh. Sensitive vasomotor and trophic disorders and neuropathic pain are detected in the anterior and medial surfaces of the thigh, lower leg and foot to the base of the first toe.
Compressive neuropathy of the external cutaneous nerve of the thigh (Roth disease). In neurological practice, isolated neuritis n. cutanei femoris lateralis
(LII, III), giving the clinical picture described by V.K.
Rotom (1895) under the term “ meralgia paraesthetica”
(from the Greek “
meros
” - thigh). This type of neuropathy is characterized by attacks of pain and paresthesia in the area of the outer surface of the thigh and is one of the most common types of tunnel syndromes due to anatomical and topographical features. The external cutaneous nerve enters the thigh medially from the anterior superior iliac spine, where it penetrates the external bundles of the inguinal ligament. Compression of the nerve trunk in this area can be caused by banal compression by a belt, bandage or corset. Metabolic disorders or excess fat deposition in the lower anterior abdominal wall and thighs, leading to tension on the nerve trunk, increases the incidence of lesions of the external cutaneous nerve of the thigh. The main clinical manifestation of this type of neuropathy is numbness or burning pain along the anterior outer surface of the thigh. In later stages of the disease, analgesia occurs in the innervation zone. The pain in patients increases noticeably when standing and walking, but may be completely absent when lying down. Many patients experience paresthesia in the form of numbness, tingling, and burning. A characteristic symptom found in Roth's disease is increased pain and paresthesia in cases where the patient puts keys or a phone in the pants pocket on the affected side. An objective examination reveals slight hypoesthesia of the skin in the area innervated by this nerve. With a long course, symptoms of trophic skin disorders are possible, but motor disorders in the thigh area are not detected, as is muscle atrophy. Palpation and percussion of the nerve trunk medially from the anterior superior iliac spine causes local pain.
Compressive neuropathy of the saphenous nerve
(
n. saphenus
), which is the terminal branch of the femoral nerve, is most often caused by its compression in the fascial gap as it exits the adductor canal approximately 10 cm above the knee joint on the anterior inner side of the thigh. Clinically, this syndrome is manifested by pain, paresthesia and sensitivity disorder in the area of the medial edge of the knee, the anterior and medial surfaces of the leg and the inner edge of the foot, and a decrease in the secretion of sweat glands is also possible. With percussion and palpation, an area of pain is identified with irradiation of pain into the anterior internal region of the knee joint, the inner surfaces of the lower leg and foot. The pain increases with hip extension and adduction; at the point of exit of the saphenous nerve, the Tinel and Goldberg symptoms are positive. The patient is characterized by a gait disorder: he avoids fully extending the lower leg and walks with his leg slightly bent at the knee joint. There are no motor disorders, the knee reflex is preserved, and there is no muscle atrophy.
Compression-ischemic neuropathy of the common peroneal nerve.
In typical cases, this syndrome develops distal to the head of the fibula, where the nerve trunk or neurovascular bundle is pinched between the fibula and the fibrous edge of the peroneus longus muscle, which starts from the head of the fibula. This pathology was first described by French clinicians in 1934 as “occupational paralysis of tulip bulb diggers,” which is why in some works it bears the author’s name: Guillain-Seza-de Blondin-Walter syndrome. The disease primarily affects workers who squat and kneel, who spend a long time in a “leg-to-leg” position, and who wear a plaster cast. The peroneal nerve is the most vulnerable of all the nerve trunks of the lower extremities. It is very sensitive to injury and relatively easily causes traumatic neuritis, while the adjacent tibial nerve completely retains its function. Even in cases where the injury affects the common trunk of the sciatic nerve above its division into the tibial and peroneal nerves, the peroneal fibers may be affected selectively or predominantly. It is necessary to take into account the possibility of dividing the sciatic nerve into its main branches much above the popliteal fossa. Dislocation in the knee joint and reduction of dislocation in the hip joint can also cause peroneal nerve palsy. This type of neuropathy is clinically characterized by predominantly acute (less often subacute) development of peripheral paresis of the extensors of the foot with gait disturbance, paresthesia and hypoesthesia along the outer surface of the leg and on the dorsum of the foot. Intense pain syndrome with damage to the peroneal nerve is rare, since thin unmyelinated fibers are practically not included in its composition. Quite often this syndrome is bilateral. Peroneal nerve neuropathy causes characteristic foot drop and makes it impossible to straighten the foot and toes. The patient cannot stand on his heel, abduct the foot, or raise its outer edge. The muscles of the anterior surface of the leg atrophy. Hypoesthesia is detected, spreading to the outer surface of the lower leg, the back of the foot, and the inner surfaces of the first and second fingers. Vegetative-trophic disorders are usually minor. Palpation and percussion of the nerve at the level of the head and neck of the fibula are painful and are accompanied by paresthesia in the area of innervation of the nerve. Forced plantar flexion with simultaneous supination of the foot causes or increases pain in the area of the head of the fibula.
Compression-ischemic neuropathy of the tibial nerve (tarsal canal syndrome, Richet canal syndrome). This type of neuropathy is a consequence of compression of the distal part of the tibial nerve in the internal ankle fibrous canal, which connects the ankle joint with the plantar region. The Richet canal has 2 openings (superior and inferior), through which the tendons of the tibialis posterior muscle, long flexor muscles of the big and other toes, and the posterior tibial neurovascular bundle pass. The nerve lies outside the artery and projects at an equal distance between the Achilles tendon and the posterior edge of the inner malleolus. Most often, tarsal tunnel syndrome develops due to mechanical compression of the nerve by tight shoes, trauma, or repeated microtrauma of the ankle with fibrosis and thickening of the plantar fascia. In addition, it can be observed in rheumatoid arthritis, hypothyroidism and tenosynovitis. Damage to the nerve itself or the neurovascular bundle in this area makes it impossible to flex the foot towards the sole, as well as the toes. The patient cannot stand on the toe of the corresponding leg; his foot is bent to the rear. The muscles of the back of the lower leg atrophy over time. A neurological examination reveals the absence of the Achilles reflex. The impossibility of active supination of the foot develops, the toes take on a claw-like position. Sensory disorders manifest themselves in the form of intense pain. In addition, hypoesthesia of the sole and back of the leg may be observed. In some cases, pain irradiates from the foot along the sciatic nerve to the gluteal region, which makes diagnosis difficult. Vegetative-trophic disorders are sharply expressed. Compression (Goldberg test) and percussion (Tinel test) of the nerve in this area can cause characteristic pain and paresthesia in the plantar part of the foot, sometimes spreading to the posteromedial part of the leg. The same symptoms occur with simultaneous pronation and extension of the foot; Supination of the foot and flexion of the ankle joint reduce pain.
The treatment tactics for compression-ischemic neuropathies are based on an adequate combination of etiological, pathogenetic and symptomatic approaches. For effective treatment, it is necessary to identify the cause and mechanisms of compression and, if possible, eliminate these causes [9, 10]. The radical method of treating most tunnel syndromes is surgery - dissection of the tissues compressing the nerve and creation of optimal conditions for the nerve trunk, preventing its injury. However, according to numerous studies, the long-term effectiveness of surgical and conservative methods does not differ significantly [11].
The main mechanism of conservative etiotropic therapy for compression-ischemic neuropathies is the restoration of an adequate motor stereotype and biomechanics of movements. However, despite the high effectiveness of these methods in the treatment and prevention of neuropathies, they act slowly and require the indispensable addition of pathogenetic and symptomatic techniques [12].
Pathogenetic therapy for neuropathies is based on the restoration of damaged nerve tissue. Metabolic therapy of the nerve includes vitamin therapy, antioxidants, and vasoactive drugs. Relatively new in domestic neurological practice is the use of nucleotides - low-molecular structural elements that play a fundamental role in metabolic processes, are involved in energy conservation and the transfer of certain groups of molecules, and also act as intracellular signaling proteins. In addition, nucleotides are important components of nucleic acids, particularly DNA and RNA. One of the most frequently mentioned nucleotides in medicine, uridine monophosphate plays a major role in the neuronal synthesis of all necessary pyrimidine nucleotides [13, 14]. The mechanism of action of uridine in peripheral neuropathies is multifactorial in nature and includes regeneration and prevention of further degeneration of the peripheral nervous system. After penetration into the nerve cell, part of the uridine undergoes amination to form cytidine, and the remaining uridine and newly formed cytidine become fundamental components of DNA and RNA, increasing the activity of their transcription and translation processes. It is these substances that have an important enzymatic function in the biosynthesis of membrane components such as phospholipids, glycolipids and glycoproteins, which perform an important function in the formation and action of axons and their myelin sheath. In addition to the intracellular effect, pyrimidine nucleotides also have an effect on the nervous system, activating membrane receptors, which stimulates the proliferation of Schwann cells and their migration and adhesion to the axon of the damaged nerve [15, 16].
Uridine monophosphate is presented in the form of a dietary supplement (BAA) Keltican complex, which also includes vitamin B12 and folic acid. This combination was selected as the most effective stimulator of nervous tissue restoration - B12 is involved in the stages of synthesis of purine and pyrimidine nucleic bases, nucleic acids and proteins, and folic acid acts as a coenzyme in many catalytic reactions, especially in the metabolism of protein and nucleic acids (in the synthesis purine, DNA and the assembly of various amino acids), is involved in the biosynthesis of neurotransmitters, phospholipids and hemoglobin. Thus, the Keltican complex promotes nerve regeneration by replenishing the increased need of nervous tissue for the synthesis or utilization of lipids and proteins [17].
The results of numerous foreign clinical studies [18–21] have shown the effectiveness of nucleotides in various metabolic, vertebrogenic, infectious and compression-ischemic lesions of nervous tissue. In the domestic literature there are only isolated reports [22, 23] on the effectiveness of nucleotides, which is associated with the recent appearance of the dietary supplement Keltican complex on the Russian market. Nevertheless, the authors' own limited experience confirms the optimistic prospects for the use of nucleotides in patients with peripheral neuropathies.
We observed 34 patients (18 women and 16 men) with back pain and compression-ischemic neuropathies of various locations. Nucleotide therapy was used for patients with a long history of the disease (from 3.5 months to 1.5 years). Traditional pharmacotherapy was supplemented by taking 1 capsule of the dietary supplement Keltican complex with meals for 1 to 2 months. All patients receiving nucleotides experienced a more rapid recovery of motor functions, including restoration of reflex activity and improvement of vegetative-trophic function. However, the most significant was the reduction in the intensity of the pain syndrome, which made it possible, on the one hand, to reduce the dose of painkillers and thereby reduce the number of side effects; on the other hand, the reduction in pain syndrome made it possible to carry out the process of rehabilitation of motor function more actively, with the inclusion of kinesitherapy and therapeutic physical education, which made it possible to reduce the period of disability of patients. The dietary supplement Keltican complex can be used in patients with back pain as a source of additional substances and helps restore damaged nerve fibers in diseases of the spine and peripheral nerves, thereby facilitating a more rapid restoration of well-being and performance. Particular attention in this study was paid to safety issues. There was not a single patient who refused nucleotide therapy due to side effects, which is quite predictable: the components of the Keltican complex dietary supplement are organic compounds, some of them are synthesized in the human body itself. The safety of uridine (in combination with or without vitamins) was also demonstrated during large-scale foreign studies [24, 25], which involved a large number of patients. No serious adverse effects or deaths were reported.
It should be noted that therapy for back pain and compression-ischemic neuropathies must necessarily include non-drug treatment methods. Manual therapy with elements of kinesitherapy, kinesitis taping, and biofeedback methods play a leading role in the formation of the correct motor stereotype and restoration of the disturbed biomechanical pattern. Of the physiotherapeutic methods, the most effective are massage, phonophoresis with glucocorticosteroids on the area of compression in the acute stage of inflammation, and for chronic scar-adhesive processes - electrophoresis with lidase and shock wave therapy of high frequency and low intensity. Reflex treatment methods are also important: acupuncture, laser, and auriculotherapy. Physical therapy exercises under the guidance of an experienced instructor, who will be able to continue to monitor the correctness of independently performed exercises, will help restore adequate movements.
Thus, back pain accompanied or caused by compression-ischemic neuropathies remains a difficult therapeutic task due to the complexity of diagnosis and the need for complex treatment. But the therapeutic options available today allow us to hope for its successful solution, since emerging new drugs have a high degree of efficiency in restoring damaged nerve fibers, good compliance and safety.
The authors declare no conflict of interest.
*e-mail; https://orcid.org/0000-0003-4364-0123
Tripod symptom for osteochondrosis
Another reliable sign of the development of osteochondrosis is tripod syndrome. It allows you to distinguish between psychogenic pain in the back and that reflected in the development of pathologies of the internal organs of the chest and abdominal cavity. Using the tripod syndrome, the doctor can assess the condition of the spinal column, the muscular frame of the back, nerve fiber, tendon and ligament apparatus.
With vertebrogenic pain syndrome, characteristic clinical signs are present. This is muscle tension and spasm, the inability to perform certain actions, a feeling of stiffness and much more.
A specific sign of the development of osteochondrosis and an attack of vertebrogenic radicular pain is tripod syndrome. In order to recognize this tension syndrome, the doctor must pay attention to the position of the patient’s body when trying to rise from a lying position, when sitting on a chair, when getting out of bed, etc.
Distinctive signs of positive tripod tension syndrome:
- lying on his back, the patient tries to raise his torso by resting his hands on a hard surface; if he sits down in a semi-recumbent position, he must support the weight of his torso by resting on his hands;
- when asked to get out of bed, the patient first turns over on his side or stomach and only after that, leaning on his hands, he rises, while trying not to use the muscles of the back and lower back as much as possible;
- the seating position on the chair is also specific - the torso is tilted back, the arms are moved behind the back and the body weight is transferred to them.
Tripod syndrome is a unifying term for all positions of the human body in which he tries to maximally unload the muscles of the back and lower back and at the same time transfer weight to his arms.
IV. Treatment of radiculitis (radiculopathies)
IMPORTANT! Treatment is aimed, first of all, at eliminating the causes leading to the disease!
The main method of treatment is complex therapy, which is aimed at:
- to eliminate muscle spasms and pain,
- to eliminate compression of nerve roots, blood vessels,
- to activate metabolic processes in the affected area, improve trophism and microcirculation,
- for the prevention of repeated exacerbations of radiculitis and other spinal diseases
- central analgesics that help to avoid or reduce chronic pain syndrome associated not with problems in the spine, but with pathological restructuring of the pain perception system.
The most effective complex treatment , which includes:
- restriction of physical activity during an exacerbation should not be long; according to research, early expansion of physical activity helps prevent chronic pain;
- during an exacerbation, a method of drug therapy using painkillers, anti-inflammatory non-steroidal drugs, muscle relaxants, corticosteroids, drugs that improve microcirculation in tissues;
- manual therapy (osteopathic techniques), reflexology, massage and skeletal traction;
- physiotherapeutic treatment methods - shockwave therapy, laser radiation, ultrasound therapy, etc.
- physical therapy, swimming
Symptoms of tension in cervical osteochondrosis
Osteochondrosis of the cervical spine also gives symptoms of tension, which manifest themselves in the collar area, upper chest, and shoulders. Determining the symptoms of tension in cervical osteochondrosis is quite simple - for this, the person needs to be asked to raise or move their arm to the side, and tilt their head.
For example, with positive Bonnet tension syndrome, the patient cannot move the arm raised to shoulder level to the side and bring it back. In this case, the upper limb on the side where there is no damage to the radicular nerve moves freely in different directions. In Bonnet syndrome, sensory disturbances are also present. Local areas of decreased skin sensitivity are identified along the back surface of the shoulder and forearm. When palpating the cervical spine, shoulder, collar area and upper limb, pain is detected only at the site of localization of degenerative dystrophic destruction of the intervertebral disc.
The Wasserman-Matskevich symptom is a combination of two clinical signs that appear with severe muscle tension in the neck and collar area. To determine them, the patient is asked to lie on his back on a hard surface. Then he should take turns raising his arms up in front of him and abducting them in different directions at different angles. With positive tension syndrome, raising your arm up in front of you will be accompanied by severe pain in the area of the shoulder blade and forearm.
Neri's tension syndrome may indicate inflammation or compression of the dorsal roots of the spinal cord. To determine it, the patient must stand up straight with his legs straight. Then the doctor asks him to tilt his head as far as possible towards his chest so that his chin touches his chest. If it is impossible to do this on their own, the doctor helps the patient until the chin touches the sternum or until the patient says that he has severe pain in the lumbar or collar area. This tension syndrome is present with radiculitis, myelitis of the roots, herniated intervertebral disc in the cervical spine.
Neri's tension syndrome can be positive when osteophytes grow in the area of the cervical and cervicothoracic spine, osteochondrosis with radicular syndrome, displacement of vertebral bodies, destruction of intervertebral joints with compression of the roots, etc.
Also, with cervical osteochondrosis, Dejerine's syndrome is of great diagnostic importance. It indicates damage to the membranes of the spinal cord. If a person experiences pain only during a certain type of physical activity, for example, when turning the head to the side, then this indicates a positive symptom of Dejerine’s tension.
Introduction
Vertebrogenic diseases of the peripheral nervous system are observed in most cases in people aged 25-50 years and are the main cause of temporary disability (Kuznetsov V.F. 2000), which is a serious medical and social problem.
In the nosological aspect, among other diseases, 5-10% of all patients suffer from dorsopathy. Dorsopathy is a group of diseases of the musculoskeletal system and connective tissue, the leading symptom complex of which is pain in the trunk and extremities of non-visceral etiology. The most common cause of dorsopathies is spinal osteochondrosis - a degenerative process in the intervertebral discs involving the bodies of adjacent vertebrae (spondylosis), intervertebral joints and the ligaments of the spine (Fedin A.I. 2002).
Neurological manifestations of spinal osteochondrosis account for about 50-80% (Voznesenskaya T.G., 2000) of all diseases of the peripheral nervous system, mainly during the period of active work (Markin SP. 2005). In first place in terms of frequency of occurrence is damage to the lumbosacral spine (60-80%).
Clinically, spinal osteochondrosis manifests itself in the form of a reflex syndrome (occurs in 90% of cases) and compression syndrome (detected in 5-10% of cases). Compression syndromes are caused by the mechanical effect of a hernial protrusion, bone growths or other pathological structure on the roots, spinal cord or blood vessels. Compression syndromes, in turn, are divided into radicular (radiculopathy), spinal (myelopathy) and neurovascular syndromes (Yakhno N.N. 2001).
The most important type of dorsopathies is dorsalgia (back pain), which affects about 80% of the population during their lifetime (Waddel G. 1998). Among all types of dorsalgia, lumbodynia accounts for about 70%. More often than others, combined pain syndromes occur, in particular lumboischialgia, which has the following forms: muscular-tonic, neurodystrophic and neurovascular (Shostak N. 2005).
Neurovascular lesions with a predominant localization in the extremities are divided according to clinical manifestations into vasospastic, vasodilator and mixed types. The mechanism of vascular (dyscirculatory) lesions can be compression, due to a direct effect on the radiculo-medullary vessels, or reflex (Visscher CM, 2001), leading to acute or chronic insufficiency of the spinal roots or spinal cord, which leads to the development of motor disorders and sensory impairment ( Popelyansky Y.Yu. 2003).
Taking into account the multifactorial etiopathogenesis and diversity of clinical manifestations of dorsopathy, the development of new methods for the rehabilitation of this pathology remains relevant in order to increase the clinical effectiveness of treatment.
In the arsenal of applied methods for treating this disease, an important place is given to the use of natural and preformed physical factors that have both local and general effects, causing adaptive reactions, activating the body's reserve capabilities and aimed at relieving pain, correcting vascular disorders, and improving the functional state of the nervous system .
Numerous studies indicate the wide therapeutic potential and high efficiency of low-frequency pulsed electromagnetic fields, the local effect of which has a pronounced anti-edematous, absorbable, anti-inflammatory, antispasmodic, analgesic, trophic-regenerative effect (Prato FS 2000). The magnetic field improves microcirculation in the perineural sheath, the trophic function of the myelin sheath, and helps normalize the functional state of the neuromuscular system.
The technical capabilities of most modern physiotherapeutic devices generating a low-frequency magnetic field are limited in terms of the area of maximum impact on all pathogenetically and clinically significant areas of the lesion. In this regard, the presence of volumetric tape remote inductors in the “POLIMAG-01” device allows for the possibility of simultaneous exposure to large areas of the patient (torso, legs), increasing the effectiveness of magnetic therapy for this nosology.
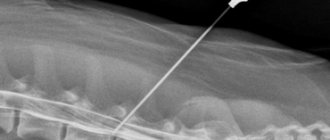
At the Russian Scientific Center for Rehabilitation Medicine and Balneology of Roszdrav, clinical trials were carried out on the effects of low-frequency traveling magnetic fields generated by the physiotherapeutic device “POLIMAG-01” in patients with neurovascular syndrome due to dorsopathy of the lumbar spine.
The device "POLIMAG-01" was produced in Russia: Elatomsky Instrument Plant.
The purpose of the study was to study the feasibility and effectiveness of using a low-frequency traveling magnetic field generated by the physiotherapeutic device "POLIMAG-01" in patients with neurovascular syndrome and dorsopathy of the lumbar spine.
Criteria for inclusion in the study:
- Dorsopathy of the lumbar spine (osteochondrosis, lumboischialgic syndrome)
- The presence of discopathy (hernia, protrusion of the intervertebral disc) confirmed by MPT, CT of the lumbar spine
- Neurovascular syndrome (clinical data, rheovasography indicators of the lower extremities)
- Absence of absolute signs of atherosclerotic vascular lesions (lipid profile, ECG, etc.)
- Patient consent
Exclusion criteria from the study:
- General contraindications to physiotherapeutic effects of a magnetic field.
- Atherosclerotic vascular damage (dyslipidemia, coronary heart disease).
- Arterial hypotension
Table 1: Scheme of the clinical study of the effectiveness of "POLYMAG"
| 1 day | 1-14 day | Day 14 | |
| Clinical and neurological status | X | X | X |
| Visual analog pain scale | X | X | |
| Clinical blood test | X | X | |
| Biochemical blood test (lipidogram) | X | ||
| Analysis of urine | X | X | |
| Rheovasography of the lower extremities | X | X | |
| ECG | |||
| Magnetic therapy course | X | X | X |
What to do if tension pain syndromes appear
Painful tension syndromes indicate that compression damage to the structures of the autonomic nervous system occurs. This may be the spinal cord, its dural membranes or radicular nerves. In any case, muscle spasm occurs, which is not relieved by the use of non-steroidal anti-inflammatory drugs. Pain from muscle tension can only be relieved with the help of muscle relaxants. But this measure does not always give a positive result.
What to do if tension pain syndromes appear? It is necessary to conduct a thorough differential diagnosis. This should be done by a neurologist, vertebrologist or orthopedist. These doctors determine what pathological change has occurred in the tissues of the spinal column. Then, after an accurate diagnosis is made, treatment is carried out.
It is most effective to treat osteochondrosis and its complications using manual therapy methods. The following techniques are used:
- osteopathy allows you to restore normal processes of microcirculation of blood and lymphatic fluid, due to which the physiological structure of the tissue is restored;
- massage improves the elasticity and permeability of muscle tissue, increases its saturation with oxygen and glucose, which has a positive effect on the diffuse nutrition of cartilaginous intervertebral discs;
- therapeutic exercises and kinesiotherapy regulate the tone of the muscular frame of the back and restore its performance;
- reflexology allows you to start the process of regeneration of all damaged tissues by using the hidden reserves of the human body.
Physiotherapy, laser treatment and much more are also used. If you need effective and safe treatment for tension pain syndromes due to osteochondrosis of the spinal column, then you can contact our manual therapy clinic in Moscow. Here you will be offered a free initial examination. During it, a preliminary diagnosis will be made and recommendations for subsequent examination and treatment will be given.
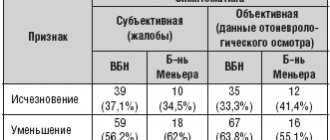
Research results
Upon completion of the course of exposure to POLYMAG, a subjective and objective assessment of the effectiveness of treatment was carried out.
In general, the procedures were well tolerated. As a result of the treatment, the majority of patients improved their general condition, and positive changes occurred in the subjective and objective manifestations of the disease. Analysis of effectiveness (significant improvement or improved performance) showed that clinical effect was observed in 59% of cases. As a result of the treatment, according to the VAS pain (measured in cm), the intensity of the pain syndrome decreased from 4.8 ± 1.5 points to 2.1 ± 1.6 points, while in the control group to 3.5 ± 0. 5 points.
Against the background of the treatment, in 48% and 42% of patients in the main group, respectively, there was a positive trend in the symptoms of Lasegue and Matskevich in the form of a decrease in the angle of onset of pain.
A study of the dynamics of activity of the reflex sphere revealed activation of initially weakened tendon reflexes of the lower extremities in the main group in 52% of patients, while the appearance of initially absent reflexes was not observed.
Also in the main group, 78% of patients who complained of cramps in the calf muscles experienced a significant decrease in the incidence of cramps. In the control group, a decrease in the frequency and severity of calf muscle cramps was recorded in 21% of patients.
In the main group, there was a tendency towards a decrease in both systolic (SBP) and, to a greater extent, diastolic (DBP) blood pressure, which is probably explained by the effect of peripheral vasodilation observed when exposed to a magnetic field (Table 2).
Table 2: Dynamics of blood pressure in patients with lumbar spine dorsopathy
| GARDEN | DBP | |||
| Before treatment | After treatment | Before treatment | After treatment | |
| 1 group | 138±4,5 | 124±3,8* | 88,4±4,6 | 69,2±6,5* |
| 2nd group | 135±6,3 | 30±7,5 | 86,1±7,2 | 81,4±7,3 |
*-P<0.05
Rheovasographic studies showed a beneficial effect of “POLYMAG” on the regional hemodynamics of patients in the form of improvement in the shape and structure of rheographic curves and quantitative indicators of RVH. However, these positive changes mainly affected patients with a vasospastic type of peripheral circulation. An increase in the initially reduced RI was noted (in 57% of patients with an initially reduced RI), which characterizes an increase in pulse blood filling of the lower extremities; a decrease in the tone of small vessels was also observed in the form of a decrease in the initially high values of DkI (64% of patients). In 71% of patients, a decrease in CI was noted, which indicates an improvement in venous outflow.
In patients with the hypotonic type of RVH, there was a significant decrease in the initially elevated RI, CI and an increase in the initially reduced DCI in the main group in 28% of patients, while in 45% there was an increase in RI and this is probably due to the vasodilating effect of the magnetic field.
Table 3: Dynamics of rheovasography indicators of the lower extremities during the treatment “POLIMAG-01” for discogenic dorsopathy
| Groups of Patients | RVG indicators | Values |
| Group 1 (n=20) | RI (Ohm) | 0,51±0,08* 0,78±0,05 |
| DkI (%) | 43,9±2,1* 35,2±1,25 | |
| CI (%) | 39,4±2,5 35,4±1,6 | |
| Group 2 (n=20) | RI (Ohm) | 0,48±0,08 0,62±0,1 |
| DkI (%) | 43,7±1,8 39,2±1,9 | |
| CI (%) | 40,2±1,8 39,2±1,5 |
Note: n is the number of patients; in the numerator - indicators before treatment, in the denominator - after treatment * - P <0.05
The content of total cholesterol in both groups was within normal limits (4.8 ± 0.6 mmol/l, triglycerides - 1.3 ± 0.3 mmol/l) and no significant dynamics were observed during treatment.
Thus, a course of treatment with a magnetic field generated by the “POLIMAG-01” device in patients with neurovascular syndrome with discogenic dorsopathy of the lumbar spine contributed to a decrease in the severity of radicular syndrome (lumboischialgia, cramps, sensory disorders) and improvement of peripheral hemodynamics (mainly with vasospastic type of circulation lower extremities).