Price list Doctors clinic
Spinal manual therapy is a set of techniques for manipulating the spinal column and back muscles. It is used for various diseases of the musculoskeletal system and allows you to eliminate pinched nerves, improve the mobility of the vertebrae, improve blood supply to tissues, and helps accelerate the relief of inflammation. Do not confuse manual therapy with massage - in the latter case, a specialist acts only on muscles, while a chiropractor works with muscles and vertebrae, intervertebral discs, joints, bones, and ligaments.
Operating principle
Manual spinal massage is based on ancient treatment techniques that came to us from the East. These include the following:
- techniques for working with soft tissues: skin, muscles, subcutaneous fat;
- work with joints;
- manipulation of tissues coming from the field of osteopathy;
- body-oriented therapy: relaxation techniques, removing tension;
- impact on the cervical spine;
- visceral therapy: work with putting internal organs in place.
Therapy can be combined with certain treatment methods: medication, surgery (after tissue healing). It is not recommended to accompany manual therapy with a number of methods that involve thermal effects - mud therapy, paraffin-ozokerite applications, physiotherapy.
Objectives and results
The main objectives of manual therapy are to restore normal muscle tone, relieve pain, and improve the mobility of the vertebrae and tissues. Using this approach you can achieve the following results:
- slow down age-related changes by increasing range of motion;
- strengthen the muscle corset;
- improve posture;
- reduce spinal column deformities;
- eliminate pinched nerves and blood vessels.
One session of manual spinal therapy can reduce pain symptoms. It restores blood supply to tissues and eliminates headaches and muscle pain. Relieving muscle spasm allows you to return the correct anatomy to the musculoskeletal system, and therefore cope with the consequences of hernias and osteochondrosis. The return of normal posture leads to normalization of the position of internal organs, improvement of overall health and well-being.
Clinically Relevant Anatomy
Clinically Relevant Anatomy
Extensor pollicis brevis
- Beginning: ½ of the posterior surface of the body of the radius, interosseous septum of the forearm.
- Attachment: base of the proximal phalanx of the thumb.
- Functions: wrist joint: radial abduction;
- thumb: extension.
Abductor pollicis longus muscle
- Beginning: posterior surface of the radius and ulna, interosseous septum of the forearm.
- Attachment: base of the first metacarpal bone.
- Functions: wrist joint: radial abduction;
- thumb: abduction.
Features of the event
Manual therapy involves the use of hands as the only instrument of influence. There are several basic techniques:
- manipulative: these are short, medium-intensity jerk-like movements, with the help of which a specialist restores the mobility of joints and vertebrae;
- mobilization: movements that restore joint mobility, improve blood flow, gently stretch the spine, relieve swelling by normalizing lymph flow;
- soft: the technique is designed to normalize muscle tone, relieve pain, eliminate ligament pathologies, make them more elastic and mobile. It does not involve sudden movements.
There are other techniques: craniosacral therapy, shiatsu massage, lymphatic drainage, kinesiological techniques, etc. In each clinical case, the specialist selects a set of techniques, taking into account the disease, symptoms, and condition of the patient.
The frequency of sessions is determined by the state of health and the goals set. Usually up to 2 procedures are performed per week, but for some diseases it is advisable to visit a chiropractor more often. The number of sessions required also varies, in one case three are enough, in another a course of up to 15 will be required.
The duration of one session is 10-30 minutes.
Treatment
The goal of treatment for de Quervain's tendonitis is to reduce pain caused by irritation and swelling.
Conservative treatment
The goal of nonsurgical treatment is to reduce pain and swelling. At the initial stage the following can be used:
- Immobilize the thumb or wrist joint with a splint or splint to rest the tendons. So far, clinicians have not reached a consensus on the duration of wearing orthoses: a number of experts recommend wearing them for 4-6 weeks, others recommend wearing them only during periods of pain.
- Avoiding repetitive movements and movements that aggravate the condition.
- Applying ice.
- Taking NSAIDs.
- Injections of corticosteroids into the synovial membranes.
- Physical therapy.
Patients may also be required to be immobilized for up to 6 weeks. To do this, use a bandage on the thumb. It was found that when wearing an orthosis, improvements occurred in 19% of cases. However, with simultaneous use of NSAIDs, this figure was even higher and amounted to 57%.
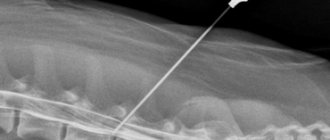
Ultrasound examination, according to some estimates, can have a positive effect on treatment results. In addition, it can act as a diagnostic tool. Injections administered under ultrasound guidance were more effective. In addition, there were no side effects. Ultrasound-guided injections performed into the extensor pollicis brevis area with septation are more effective than manual injection.
Another effective conservative treatment option is steroid injection, but more research is needed to establish its full benefits.
Direct injection of a small dose of cortisone into both tendons has worked well. For primary disease, the effectiveness of this measure is about 60-70%.
Who is indicated for spinal manual therapy?
The main indications for manual spinal massage are the following:
- back pain, including muscle pain, associated with osteochondrosis;
- discomfort in the cervical-collar area;
- headaches and dizziness;
- pain associated with previous injuries;
- deformations and curvatures of the spine - kyphosis, lordosis, scoliosis;
- contractures, mobility restrictions, decreased range of motion;
- protrusion, hernia;
- pinched nerves;
- spasms, disturbances in the tone of the muscles of the back and neck.
You can contact a chiropractor not only if you have painful symptoms, but also for preventive purposes. People who practice a sedentary lifestyle are at risk for developing musculoskeletal diseases. Working behind the wheel or at a computer monitor can lead to impaired blood supply, congestion, inflammatory and degenerative processes in the spine and adjacent tissues.
Pinched nerve
Often after increased stress or hypothermia we hear: such pain, a nerve is pinched! And everyone understands that it is difficult and bad for a person, that he moves with difficulty, and experiences constant pain. What is a pinched nerve and how to get rid of it?
Symptoms of a pinched nerve
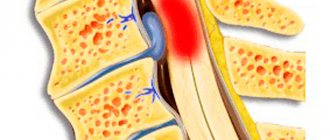
It is known that from the spinal cord nerves diverge throughout the body, innervating every muscle. If provoking factors occur, the nerve may become pinched by a spasmed muscle, a neighboring vertebra, or a painful formation on the spine. It is in the area where the pinched nerve occurs that the symptoms of the disease increase most clearly. The main symptom is always pain. Pain when a nerve is pinched can be sharp, stabbing, aching, tugging, or whatever, but it is always present. The second characteristic symptom is limited mobility in the affected area, or in the area innervated by the pinched nerve.
Treatment of a pinched nerve
If you find signs of a pinched nerve, you need to consult a neurologist. But before you get an appointment, you can ease your condition a little. You can put a mustard plaster on the painful area or apply a warming ointment. Through local action, the thermal procedure will relieve pain for a short time. You can take any painkiller, but you shouldn’t get too carried away with them. In addition, it is necessary, if possible, to eliminate the causes of the pinched nerve. There are not so many external reasons, these are:
- Fatigue associated with increased load on the spine;
- Hypothermia;
- Traumatic impact.
Other causes of a pinched nerve include:
- Exacerbation of osteochondrosis;
- Intervertebral hernia;
- Radiculitis and other diseases.
In order for the treatment of a pinched nerve to produce positive results, an integrated approach to the problem is necessary. Your doctor will tell you how to treat a pinched nerve with medications. Nowadays, there are a huge number of non-steroidal anti-inflammatory drugs that are successfully used. Along the way, physiotherapeutic procedures are prescribed: DDT, UHF, reflexology. The patient should also know what to do if a nerve is pinched at home, and how to organize their routine.
Here are the basic requirements:
- Sleep on a hard, flat surface;
- Exclude spices, hot seasonings, smoked meats, marinades, alcohol from the diet;
- Carefully follow the recommendations of the neurologist.
Massage has become widely popular for the treatment of pinched nerves. Let's take a closer look at how to use it correctly.
Massage for pinched nerves
Let's start with the fact that in the acute period, massage with a pinched nerve is contraindicated! This procedure should be carried out only by a medical specialist and only when the disease is not exacerbating. Massage is carried out in long courses, 10-15 sessions, and repeated courses can be carried out for preventive purposes. In the media you can find many advertising offers from specialists in manual therapy, but if you risk contacting one of them, you must be absolutely sure that the manual is familiar with medicine first-hand. Hence the conclusion: a good massage is a massage in a medical facility.
Exercises for pinched nerves
Physical therapy is of great importance in the treatment of spinal pain. A medical specialist should also teach it. Exercises for pinched nerves are not performed during the period of exacerbation; they are started after the pain has been relieved. Among the therapeutic exercises, the following types can be distinguished:
- Flexion – extension exercises;
- Exercises that are performed lying on your back, on a hard surface;
- Relaxation exercises;
- Stretching exercises.
Which doctors should I contact:
- Cardiologist - Neurologist
Headache
Disorders in the cervical spine are a common cause of headaches. With the help of manual therapy, you can get rid of the root cause, as well as cope with the so-called tension pain. People who lead a sedentary lifestyle may suffer from vertebral blockade and limited mobility of the cervical spine. As a result, the muscles become toned, neck pain occurs, and subsequently frequent headaches. Improper body position during sleep (high pillow) and sudden head movements can provoke deterioration.
The price of a manual therapy session includes an initial examination and diagnosis. The doctor identifies problem areas and determines which parts of the spine are functioning incorrectly. Clarifying the source of the problem allows for effective therapy. It is important to understand that most often an X-ray or an MRI diagnostic report is required. Only after a comprehensive assessment will a specialist develop a course of treatment to normalize the condition.
Survey
Inspection
Evaluation of a patient with signs and symptoms of de Quervain's tenosynovitis should begin with a thorough history followed by a physical examination.
History taking
- Overuse injury or acute injury.
- Have symptoms appeared before?
- Repetitive hand movements during work or daily activities.
- The pain is localized above the base of the thumb and in the dorsolateral region of the wrist near the styloid process of the radius.
- One hand dominance.
- Pregnancy or postpartum period.
Physical examination
Vital Signs
- Height.
- Weight.
- HELL.
- Pulse.
- NPV.
- Temperature (if required).
In a sitting position
- Resting hand/thumb position.
- Inflammation around the base of the finger on the dorsal side and/or near the styloid process of the radius.
Neurological examination
If you have symptoms such as numbness and tingling, as well as pain, it is necessary to conduct a neurological examination and check whether the symptoms are associated with pathology in the cervical spine. It is important to determine whether the central nervous system is involved in the process, whether the sensitivity of the skin at the base of the thumb and index finger is reduced (this area is innervated by the superficial branches of the radial nerve). Pay attention to a symptom such as hand weakness and determine whether it is due to pain or a neurological problem.
Dermatomes (C4-T1)
- Myotomes (C4-T1).
- Reflexes (C5, C6, C7).
- Pathological Hoffman reflex.
Palpation
During palpation, the most significant will be the detection of such a deviation as painful sensitivity over the base of the thumb and/or the 1st compartment of the wrist extensors above the styloid process of the radius. It is also possible to palpate the thickening of the synovial vagina. It is very important to rule out arthritis or a fracture of the scaphoid by palpating the first carpometacarpal joint to determine whether there is tenderness or deformity there.
- Dorsoradial region.
- Styloid process of the radius.
- “Anatomical snuffbox” - scaphoid, trapezius, extensor digitorum longus, extensor pollicis brevis, abductor pollicis longus and first carpometacarpal joint.
- Soft tissue surrounding the affected area.
Range of motion
Range of motion can also be used as a screening tool to rule out involvement of the cervical spine, proximal joints, and anatomical structures. Note any deviations in range of motion and be aware that when testing the thumb, there may be a clicking sound and a feeling of “sticking” in the thumb. All this is associated with reduced tendon mobility.
- Range of motion in the cervical spine.
- Flexion, extension, adduction and abduction of the shoulder (right and left).
- Flexion and extension in the elbow joint (right and left).
- Pronation and supination of the forearm (right and left).
- Wrist: Flexion, extension, ulnar and radial deviation.
- Fingers two to five:
- Abduction and adduction in the metacarpophalangeal joints.
- Flexion and extension (in the metacarpal, metacarpophalangeal and interphalangeal joints).
- Abduction and adduction (in the metacarpal-carpal, metacarpophalangeal joints).
- Opposition.
Muscle tests with resistance
In the presence of pain, strength naturally decreases. Note the maximum force possible in the absence of pain. This data will be useful in tracking the patient's progress during treatment.
- Grip strength.
- Pinch strength (finger squeezing force).
Muscle length
Watch for signs of hyper/hypomobility. Treatment will be prescribed based on dysfunction. Keep in mind that areas of hypomobility are often areas of referred pain.
- Congenital flexibility (clawed hand symptom).
- Extensors and flexors of the wrist.
Joint mobility
- Distal radioulnar joint.
- Wrist joint.
- Midcarpal joint.
- Thumb.
- Metacarpal, metacarpophalangeal and interphalangeal joints.
- Brush.
- Intercarpal joints.
Specific tests
Finkelstein test
- To confirm - Finkelstein test.
- To exclude: test for osteoarthritis of the first metacarpal joint (Grind Test);
- palpation to identify a scaphoid fracture;
- Upper Limb Tension Test, or ULTT B - to determine neuritis of the superficial sensory branch of the radial nerve;
- assessing the clinical likelihood of cervical radiculopathy;
- intercarpal instability.
Neurological tests
- Upper Limb Tension Test, or ULTT B.
- Test to detect damage to the radial nerve.
- Test to detect damage to the superficial sensory branch of the radial nerve.
- Tinel's sign.
Be careful with the position of your thumb while performing tests.
Circulation
- Pallor/Capillary refill.
- It is important to use the capsule-ligamentous apparatus in the acute phase of traumatic injury.
- Stress test of the collateral ligaments of the fingers (varus/valgus).
Intervertebral disc protrusion
Manual therapy for intervertebral disc protrusions will help achieve the following results:
- removing excess muscle tone. Protrusion of the disc into the spinal canal leads to compression of the nerve roots and a reflex spasm of the adjacent muscles. Muscle relaxation can significantly reduce pain;
- stimulation of metabolism in cartilage tissue. Improving blood supply to tissues and lymph flow allows you to normalize metabolic processes around the diseased disc and speed up recovery;
- gentle stretching of ligaments and tendons. Allows you to increase the mobility of the spine, including by increasing the elasticity of soft tissues;
- reduction of protrusion. If the protrusion has recently occurred, manual therapy methods can gently realign the tissue.
The set of techniques and the strength of impact are selected individually. Twisting, manual pressure on tissue, work with ribs to increase the distance between vertebrae, etc. can be used. The specialist also chooses the position of the patient’s body individually - lying on his back or on his side. Protrusions in the cervical spine are rare. With them, the doctor acts especially carefully, paying attention to gentle stretching.
Differential diagnosis
- Intercarpal instability. The wrist is a complex anatomical area consisting of a large number of small bones and ligaments. Degenerative processes or direct trauma can lead to instability between the articulating bones, which in turn leads to pathological changes in the biomechanics of the hand and the appearance of pain. Scapholunate dissociation, scaphotrapeziotrapezial joint degeneration, and lunate-triquetral dissociation can all be associated with radial wrist pain.
- Fracture of the scaphoid bone.
- Most often, a scaphoid fracture occurs as a result of a fall on an outstretched arm with an extended wrist. In this case, pain occurs on the side of the radius, there is also swelling in the area of the anatomical snuffbox, limited range of motion, pain when performing a movement, especially at the end of the amplitude. If the patient has been injured and subsequently experiences pain in the wrist from the side of the radius, then it is first necessary to exclude a fracture of the scaphoid bone.
- Damage to the superficial branches of the radial nerve (Wartenberg syndrome). The superficial branches of the radial nerve innervate the dorsal surface of the first and second fingers and the first interdigital space. Nerve fibers can become compressed between the extensor carpi radialis brevis and brachioradialis tendons due to scar tissue formation after injury or from wearing tight jewelry. As a result of compression, ischemia develops and, as a result, numbness and tingling in the area of innervation.
- Radiculopathy of the cervical spine at the C6 level. Compression of the spinal nerve roots can cause sensory disturbances, muscle weakness, and weakened reflexes. The key dermatomes of the C6 segment are the radius of the second metacarpal and the index finger, which is approximately the same area where pain occurs in de Quervain's syndrome. It is precisely because of the similarity of symptoms that it is important to exclude cervical radiculopathy and carefully check the C6 segment.
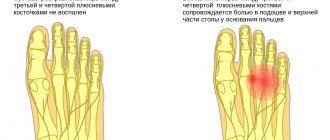
- Osteoarthritis of the first metacarpal joint. Osteoarthritis of the first metacarpal joint usually occurs in people over 50 years of age and usually manifests itself as stiffness of the joint in the morning, decreased range of motion, and tenderness in the area. With this disease, the squeeze test will be positive.
- Crossover syndrome. With this syndrome, pain will occur closer to the back of the forearm, mainly in the middle and about 5 cm below the wrist.
Scoliosis
The main goals of manual therapy for scoliosis are improving the mobility of the spine, its flexibility, stimulating muscles with reduced tone, and removing functional blocks. A thorough diagnosis includes determining the angles of curvature; it is important to provide the doctor with accurate information about the degree of the disease and concomitant diseases.
A manual spinal therapy session includes gentle stretching, working with pain areas and areas of curvature along the entire length of the spinal column. Particular attention is paid to the outer vertebrae, after which the specialist moves to the center. The doctor will definitely give recommendations for home exercises to consolidate the results obtained. Usually the course consists of ten sessions; for preventive purposes, it is enough to undergo treatment twice a year.
Kyphosis and lordosis
With a moderate degree of curvature of the spine, the doctor acts on it in such a way as to “put” the vertebrae, intervertebral discs, muscles, and ligaments in place. Typically, the course of treatment involves several sessions every other day. Pain may occur after exposure, but in this case this is a normal symptom. It is associated with the gradual movement of tissues trying to take the right position. After the course of treatment, noticeable improvements in posture, relief of pain and unpleasant symptoms are noted.
Osteochondrosis
Osteochondrosis is a degenerative-dystrophic disease in which it is important to have a comprehensive effect on the body. First of all, it is important to return the spine to its normal shape, as well as stimulate metabolic processes. The doctor may use the following techniques and techniques:
- quick movements to restore joint mobility;
- relaxing effects to relieve muscle spasms and reduce the severity of pain;
- gentle traction to normalize spinal mobility, improve blood supply, lymph flow, and metabolic processes.
You can achieve noticeable improvement after the first session. At the end of the course, pain, dizziness, tinnitus disappear, and normal range of motion in the neck and shoulders is restored.
The price of manual spinal massage is not the only advantage; this method of treatment is preferred for other reasons:
- versatility – the ability to treat osteochondrosis of any part of the spine;
- safety - unlike drug treatment, the method has few contraindications, and all techniques are used only after a thorough diagnosis by an experienced specialist;
- painlessness – the actions of a chiropractor do not cause discomfort or pain;
- general strengthening effect – manual therapy improves overall well-being, stimulates the body’s own resources for recovery;
- effectiveness - the first results can be observed after just one session; by the end of the course of treatment, a lasting positive effect is observed in most cases.
Carpal tunnel syndrome
The basis of treatment tactics is to eliminate the causes of narrowing of the carpal tunnel. This includes reduction of dislocations, immobilization of the hand, correction of endocrine and metabolic disorders, relief of inflammation and reduction of tissue swelling. Conservative therapy is carried out by a neurologist, if necessary, together with other specialists. The issue of surgical treatment is resolved with a neurosurgeon.
Conservative methods of therapy are limited to immobilization of the affected hand with a splint for a period of about 2 weeks, anti-inflammatory, analgesic, and decongestant pharmacotherapy. NSAIDs are used (ibuprofen, indomethacin, diclofenac, naproxen, etc.), in severe cases they resort to the prescription of glucocorticosteroids (hydrocortisone, prednisolone), in case of severe pain, therapeutic blockades of the wrist area are performed with the administration of local anesthetics (lidocaine). Decongestant therapy is carried out using diuretics, mainly furosemide. Vitamin therapy with gr. preparations has a positive effect. B, mud therapy, electrophoresis, ultraphonophoresis, compresses with dimethyl sulfoxide. Vascular therapy with pentoxifylline and nicotinic acid can reduce ischemia of the median nerve. After achieving clinical improvement, physical therapy, hand massage, and myofascial massage of the hand are recommended to restore nerve function and strength in the hand muscles.
If conservative measures are ineffective, carpal syndrome requires surgical treatment. The operation involves cutting the transverse carpal ligament. It is performed on an outpatient basis using endoscopic techniques. In case of significant structural changes in the carpal tunnel area due to the impossibility of using endoscopic techniques, the operation is performed in an open manner. The result of the intervention is an increase in the volume of the carpal tunnel and relief of compression of the median nerve. 2 weeks after surgery, the patient can already perform movements with his hand that do not require significant load. However, it takes several months for the hand to fully recover.
Prognosis and prevention of carpal tunnel syndrome
With timely comprehensive treatment, carpal tunnel syndrome usually has a favorable prognosis. However, about 10% of compression cases do not respond to even the most optimal conservative treatment and require surgery. The best postoperative prognosis is for cases that are not accompanied by complete loss of sensitivity and atrophy of the hand muscles. In most cases, one month after surgery, hand function is restored by approximately 70%. However, awkwardness and weakness can be observed even after several months. In some cases, relapse of carpal tunnel syndrome occurs.
Prevention consists of normalizing working conditions: adequate equipment of the workplace, ergonomic organization of the work process, changing types of activities, and taking breaks. Preventive measures also include the prevention and timely treatment of injuries and diseases of the wrist area.
Intervertebral hernia
Manual therapy for a hernia involves gentle pressure - pressure on certain centers, which allows you to return the correct position to the disc. The goals of therapy are to relieve pinched nerves, eliminate muscle tone, and restore normal sensitivity to the limbs. In case of hernias of the lumbosacral region, it is possible to restore pelvic function and relieve acute pain.
The results of the chiropractor's actions may be as follows:
- improvement of blood flow in the muscle corset;
- normalization of tissue supply with oxygen and important substances;
- acceleration of recovery;
- normalization of the position of the spine;
- improvement of metabolic processes.
Manual therapy of the spine for a hernia can complement drug treatment, while it allows you to avoid surgical intervention, reduce the dosage of medications or completely abandon them if we are talking about a symptomatic approach (taking painkillers).
Who is contraindicated for manual therapy?
Absolute contraindications to manual massage include the following diseases:
- malignant formations of any localization;
- tuberculosis;
- osteomyelitis;
- 3rd and 4th degree of vertebral instability;
- 3rd and 4th stages of osteoporosis;
- stroke;
- thrombosis of the vertebral arteries;
- inflammatory diseases of the central nervous system.
Relative contraindications include recent injuries, acute inflammatory diseases, and severe somatic illnesses. In this case, the doctor decides on the need for treatment individually; consultation with another specialist may be required.
Women need to postpone the course of treatment in the first days of the cycle. It is better to choose the time between menstruation. This is due to the fact that during the exposure the blood supply to the tissues improves, especially when it comes to working with the lumbosacral spine.
Benefits of Manual Therapy
The advantages of manual therapy for diseases of the musculoskeletal system include the following:
- the possibility of effective treatment of chronic diseases;
- general strengthening and general healing effect on the body;
- rapid analgesic effect;
- improvement of metabolic processes;
- increased range of motion;
- positive psycho-emotional effect.
Manual therapy is an art that requires impeccable professionalism. With one wrong move, a specialist can worsen the situation, so it is important to contact only qualified chiropractors with extensive experience. You can check certificates and other documents confirming the specialist’s education.
You can find an experienced doctor, check the price of a manual therapy session in Moscow and undergo preliminary diagnostics at the Family Doctor clinic.
For your information
It is necessary to distinguish normal symptoms after a session from the severe consequences of therapy. Thus, headaches and back pain can be observed as a common reaction to exposure. The sensations are associated with changes in the position of muscles and ligaments, and improved functioning of cerebral vessels. In this case, after 2-3 days there is a lasting improvement, and the pain is not acute. To improve your well-being, you can limit physical activity; massage and physical therapy prescribed by your doctor are allowed. If the pain is severe, does not tend to ease, or gets worse, you should consult a doctor.
Dizziness is a rare side effect. However, it can arise as a response of the body to a redistribution of blood volume in the body. Normally, dizziness is mild, does not interfere with daily activities, and there is no unsteadiness in gait or loss of coordination. If this symptom is pronounced or dizziness occurs after a sharp temperature fluctuation, consultation with a specialist is required.
Increased body temperature occurs even less frequently than dizziness. But if this symptom occurs, we are talking about chronic inflammatory processes that worsen when exposed. Only a doctor can clarify the reasons.
Numbness of the limbs. Causes and treatment
The most common cause of numbness in the arms and legs and sudden pain in the lumbar or neck area is a pinched nerve. This is compression of the nerve branch caught between the intervertebral disc and the vertebra. Sometimes such a nuisance is accompanied by twitching of the arms or legs, weakness and even disruption of the functioning of various organs.
Numbness of the extremities - arms and legs causes:
- Monotonous physical actions performed for a long time.
- Incorrect structure of the spine due to congenital anomalies.
- Obesity, overexertion and spinal injuries.
- Hereditary predisposition.
- Excessive physical activity.
- Rheumatoid arthritis.
- Incorrect posture.
- Respectable age.
The presence of symptoms and their intensity depend on the presence or absence of an inflammatory process, as well as on the location of the pinching. If the sciatic nerve is pinched, not only numbness can be observed, but also limited movement due to sharp pain.
First aid provided for a pinched nerve is:
- Complete rest and minimum movement.
- Rest on a hard surface.
- Call a doctor and get pain relief.