Extramedullary tumor
An extramedullary tumor is a tumor localized in the anatomical structures surrounding the spinal cord (roots, vessels, membranes, epidural membrane. Extramedullary tumors are divided into subdural (located under the dura mater) and epidural (located above this membrane). Most extramedullary tumors are meningiomas (arachnoidendotheliomas) and neuromas .
Extramedullary meningioma (arachnoidendothelioma)
Meningiomas are the most common extramedullary tumors of the spinal cord (approximately 50%). Meningiomas are usually located subdurally. They belong to the meningeal-vascular tumors, originate from the meninges or their vessels and are most often tightly fixed to the dura mater.
Extramedullary neuroma
Neuromas occupy the second place among extramedullary tumors of the spinal cord (approximately 40%). Neuromas, developing from Schwann elements of the spinal cord roots, are tumors of dense consistency. Neuromas are usually oval in shape and surrounded by a thin, shiny capsule. In the tissue of neuromas, regressive changes are often found with decay and the formation of cysts of various sizes.
Clinical manifestations of extramedullary tumors
Any lesion that leads to a narrowing of the spinal cord canal and affects the spinal cord is accompanied by the development of neurological symptoms. These disorders are caused by direct compression of the spinal cord and its roots, but are also mediated through hemodynamic disorders.
With extramedullary tumors (both intradural and epidural), symptoms of compression of the spinal cord and its roots appear. The first symptoms are usually local back pain and paresthesia. Then there is a loss of sensitivity below the level of pain, dysfunction of the pelvic organs.
The clinical picture of extramedullary tumors consists of three syndromes:
- radicular;
- half spinal cord syndrome;
- syndrome of complete transverse spinal cord lesion.
The exception is the clinical picture of damage to the cauda equina of the spinal cord (symptoms of multiple damage to the spinal cord roots from the L1 level).
Extramedullary tumors are characterized by early onset of radicular pain, objectively detectable sensitivity disorders only in the area of the affected roots, reduction or disappearance of tendon, periosteal and skin reflexes, the arcs of which pass through the affected roots, local paresis with muscle atrophy according to the lesion of the root.
As the spinal cord is compressed, conduction pain and paresthesia with objective sensitivity disorders occur. When the tumor is located on the lateral, anterolateral and posterolateral surfaces of the spinal cord, in the case of predominant compression of its half, in determining the stage of development of the disease, it is often possible to identify the classic form or elements of Brown-Séquard syndrome.
Over time, symptoms of compression of the entire diameter of the brain appear and this syndrome is replaced by paraparesis or paraplegia. Decreased strength in the limbs and objective sensory disturbances usually first appear in the distal parts of the body and then rise upward to the level of the affected segment of the spinal cord.
The symptom of a cerebrospinal fluid push is a sharp increase in pain along the roots irritated by the tumor. This increase occurs when the jugular veins are compressed due to the spread of increased cerebrospinal fluid pressure to the “displaced” extramedullary subdural tumor. With extramedullary tumors, especially if they are located on the posterior and lateral surfaces of the brain, radicular pain and sometimes conduction paresthesia often occur with percussion or pressure on a certain spinous process.
Diagnosis of a spinal tumor
X-rays are a traditional diagnostic method that allows one to see bone damage, but it is not reliable for identifying tumors.
CT scans rely on X-rays to provide a more accurate picture of the spine and accompanying bone structures, but they do not accurately show soft tissue.
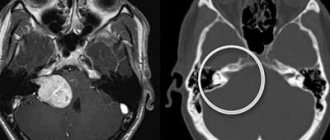
Magnetic resonance imaging is the most reliable method for diagnosing spinal tumors. The technique is based on obtaining photographs of the body, which can be viewed on a computer monitor. An MRI shows the spine along with the nerves, their roots, as well as tumors and other damage.
A biopsy is performed to find out whether the tumor is benign or malignant. During the procedure, a small area of tissue is removed for histological testing.
Intramedullary tumor
An intramedullary tumor is a tumor localized in the substance of the spinal cord. The incidence of intramedullary tumors is 10-18% of the total number of spinal cord tumors. If by their nature intramedullary tumors are often benign and slowly growing, then by their nature of growth and location they are the least favorable from the point of view of the possibility of their surgical removal. Intramedullary tumors of the spinal cord are mainly represented by gliomas ( ependymomas and astrocytomas ). Less commonly found are spongioblastoma multiforme, medulloblastoma, and oligodendroglioma.
Intramedullary ependymoma
Ependymomas most often arise from the ependyma of the central canal at the level of the cervical and lumbar thickenings. They can also develop from the filament terminale and be located between the roots of the cauda equina. Ependymomas are the most common intramedullary tumors. In 50-60% of cases, ependymomas are located at the level of the conus of the spinal cord and the roots of the cauda equina. This is followed by the cervical and thoracic spinal cord. Unlike the cervical and thoracic levels, where the tumor causes thickening of the spinal cord, at the level of the conus and roots it acquires all the properties of an extramedullary tumor. Sometimes ependymomas in this area can completely fill the spinal canal, reaching 4-8 cm in length. Ependymomas are classified as benign, slow-growing tumors. They differ from other spinal cord gliomas in their abundant blood supply, which can lead to the development of subarachnoid and intratumor hemorrhages. In more than 45% of cases, ependymomas contain cysts of varying sizes.
Intramedullary astrocytoma
Astrocytomas are characterized by infiltrative growth, are localized in the gray matter and are widely distributed along the length of the brain. Astrocytoma is the second most common intramedullary tumor after ependymoma in adults and accounts for 24-30% of all intramedullary neoplasms. In this age group, the peak incidence of tumors occurs in the 3rd and 4th decades of life. In children, on the contrary, astrocytoma is observed more often than ependymomas, accounting for up to 4% of all primary tumors of the central nervous system.
Diagnosis of intramedullary tumors
Radiological diagnosis of intramedullary tumors is quite widely developed, but most methods that can adequately judge the presence of a tumor lesion are labor-intensive and traumatic. One of the most sensitive methods in determining changes in the size of the spinal cord is magnetic resonance imaging (MRI), therefore, if the presence of an intramedullary tumor is suspected, the growth of which is usually accompanied by thickening of the spinal cord, the use of MRI should be considered the most appropriate.
Discussion
Peripheral nerve sheath myxoma is usually a multinodular benign tumor with varying degrees of stromal myxomatosis.
According to the literature [1], the typical localization is the upper limbs, head, neck, and chest. The peak incidence occurs in the fourth decade of life. In world practice, localization in the central nervous system is a rare phenomenon. In this case, it is necessary to clearly differentiate this histological type of tumor from neuroma and neurothecoma. Histological examination revealed extremely pronounced myxomatosis of the stroma; the tumor had a thin fibrous capsule over a larger area. Elongated spindle-shaped cells with eosinophilic cytoplasm and small nuclei were located relatively rarely in the myxomatous extracellular matrix, nuclei with clear chromatin, and no mitotic division figures were observed. Structures in the form of Verocay bodies, typical for neuroma, and Antony A and B patterns were also not found. An immunohistochemical study revealed the expression of protein S100, collagen type IV and Vim in tumor cells, CD34 mainly in blood vessels. Expression of smooth muscle actin, Des, EMA was negative (Fig. 4, 5)
.
Figure 4. Tumor with severe stromal myxomatosis. Hematoxylin and eosin staining. ×200.
Figure 5. S100 protein expression in tumor cells.
×400. As a result of the study, the morphological picture was regarded as a nerve sheath myxoma.
Single multinucleated giant cells and mitotic division figures were quite rare. Tumor cellularity was variable. During the study, it was necessary to make a differential diagnosis of myxoma and neuroma with stromal myxomatosis. A distinctive feature of the latter is the presence of structures typical for neuromas - Verocay bodies. Unlike myxoma, neurothecoma is a moderately cellular tumor with a less pronounced myxoid component. The cells are round or oval, more polymorphic. Among them, multinucleated giant cells are more common; at the microscopic level they have clearly defined lobulation. Immunohistochemical features of myxoma, like neuromas, are represented by the expression of the S100 protein. Neurothecoma, unlike the latter, does not express this protein. The epithelial membrane antigen EMA may be focally present in nerve sheath myxoma, while in neurothecoma it is lost, the same applies to the expression of type IV collagen and laminin. Vimentin (Vim) is quite intensely expressed in both tumors.
M. Yamato et al. [3] used multiclonal antibodies Schwann/2E. A feature of these antibodies is the ability to interact with the cytoplasm and nuclei of Schwann cells and myelin of the peripheral nervous system, while remaining intact when interacting with cells of the central nervous system. Thus, the authors, when identifying foci of interaction of antibodies with targets in the tumor, considered that the tumor originated from peripheral nerves. This fact, in addition to histological and immunohistochemical studies, confirmed that the tumor was a peripheral nerve myxoma [3].
Despite the fact that myxoma is a tumor of dermal origin, in world practice there are cases of localization of this tumor in the spinal canal [3, 4]. Compression of the spinal cord roots was caused by the tumor capsule. The clinical picture depended on the topographic-anatomical location of the tumor. Thus, the tumor more often manifested itself with pain, sensory and motor disorders [5]. Differential diagnosis, according to MRI, is difficult due to the fact that the X-ray picture is similar to meningiomas, neurinomas, neurofibromas and neurothecomas [6]. Therefore, the formation of a final diagnosis is possible only after receiving the results of the biopsy.
Symptoms of intramedullary neoplasms
The symptoms of the disease depend on the etiology of the spinal cord tumor and the severity of the pathogenesis. At the initial stages of pathology development, most serious morphological disorders are not expressed, and a person may not suspect for a long time that a dangerous process is taking place in his body. The absence of symptoms does not allow timely consultation with a specialist and initiation of treatment. The fight against neoplasms is most effective in the first stages of tumor development. The presence of pathology may be indicated by:
- pain in certain areas of the lower back, back, neck, often radiating to other parts of the body (shoulders, arms, hips, legs, buttocks, ribs, etc.);
- muscle weakness at the level of decreased or damaged tone, loss of sensitivity of the limbs, sometimes muscle atrophy;
- violation of musculoskeletal functions (decreased accuracy, retardation of movements, decreased mobility of the back, coordination disorders, unexpected falls when walking due to a surge of severe weakness in the legs, etc.);
- paresthesia of various types (numbness, burning sensation, tingling, crawling in certain areas of the back along the spine, in the abdomen, on the chest, in the limbs);
- paresis and paraplegia of any part of the body (most often the lesion affects the legs or arms);
- malfunctions of the genitourinary system or intestines, which are expressed by incontinence or retention of urine and feces; sometimes a symptom may be decreased potency or infertility;
- rise in body temperature, high blood or intracranial pressure, seizures combined with headache, weight loss.
Any discomfort in the back and spine (especially constant, often or regularly occurring) is a reason to contact a specialist and have your health checked. Clinically, a spinal cord tumor can manifest itself as an intervertebral hernia or osteochondrosis, and only differential diagnosis can help recognize which disease is associated with troubling symptoms.
Classification of intramedullary OSM
By type of formation
Depending on the type of intracerebral spinal neoplasms, the following are distinguished:
- gliomas (ependymomas, astrocytomas, oligoastrocytomas, oligodendrogliomas);
- vascular tumors (cavernomas, hemangioblastomas);
- lipomas;
- cholesteatomas;
- neuromas;
- dermoid tumors;
- teratomas;
- lymphomas;
- Schwannomas.
Vascular neoplasms are the second most common after gliomas and occur in approximately 15% of cases. Other types of OSM are much less common.
By place of origin
In accordance with this criterion, cancers are divided into two groups:
- primary.
They arise in the substance of the spinal cord; - secondary.
Another name for them is metastatic. They appear in neighboring tissues or organs (with lung cancer, breast cancer, melanoma, etc.) and spread metastases into the spinal canal.
By localization of formations
Cancers are classified by location:
- on the cervical
- chest,
- cervicothoracic,
- medullocervical,
- lumbar,
- tumors of the conus and epiconus.
In neurosurgical practice
From the point of view of neurosurgery, neoplasms are classified according to their type of growth into the following:
- diffuse.
Infiltratively growing tumors are not clearly demarcated from the spinal cord tissues and spread from one segment to complete damage to the entire spinal cord. Diffuse growth is characteristic of glioblastomas, astrocytomas, oligodendrogliomas; - focal.
They can occupy from one to seven spinal segments and have clear boundaries with the tissues of the spinal cord, which allows them to be surgically removed without unnecessary difficulties. Focal development is typical for lipomas, neuromas, ependymomas, teratomas, hemangioblastomas.
In surgical practice
From a surgical point of view, neoplasms are classified as follows:
- endophytic.
Such tumors grow inside the spinal cord and do not extend beyond the pial membrane. These include metastatic formations, astrocytomas, ependymomas; - exophytic.
These neoplasms spread beyond the boundaries of the pial membrane and grow on the surface of the spinal cord. These include lipomas, teratomas, dermoids, hemangioblastomas.
Radiation diagnostics
MRI semiotics:
Spinal tumors: expansive tumors are characterized by a rim of osteosclerosis along the periphery. Infiltrative neoplasms are characterized by a massive zone of bone marrow infiltration with uneven, unclear contours, surrounded at the periphery by a zone of edema; Cortical defects, tumor spread to the periosteum and the formation of an extraosseous component are also detected.
The structure of the neoplasm can be homogeneous or heterogeneous due to the presence of septations, cystic cavities, foci of hemorrhage, calcification and ossification.
T1-weighted image: iso-/hypointense signal.
T2-weighted image: hyperintense signal.
T1+Gd: predominantly contrast accumulation.
Spinal cord tumors: an increase in the size of the spinal cord, often with lumpy, uneven contours. Several segments of the spinal cord are affected. Peritumoral edema is often present.
T1-weighted image: iso-/hypointense signal.
T2-weighted image: hyperintense signal.
T1+Gd: contrast accumulation.
DIFFERENTIAL DIAGNOSIS (for spinal cord tumors): spinal cord infarction, multiple sclerosis, ADEM, transverse myelitis.
Rice. 1. T2 car, T1 car, T1+Gd. Space-occupying formation of the spinal cord at the level of the Th3-Th7 vertebrae, accumulating CV. Ependymoma.
Rice. 2. T2 car, T1+Gd. Volumetric formation of the presacral region involving the S4, S5 vertebrae and coccyx, diffusely and heterogeneously accumulating CV. Chordoma.
Rice. 3. T1+Gd. Focal accumulation of CV in the spinal cord at the level of C2, Th4, Th4-Th5, Th11 vertebrae. Lung cancer metastases to the spinal cord.
Causes
The rapid development of medicine today, unfortunately, does not make it possible to comprehensively answer the question of what is the reason for the development of intramedullary tumors of the spinal cord. However, the following factors may contribute to the appearance of neoplasms:
- genetic predisposition (if one of the parents was diagnosed with ASM, then the risk of its occurrence in the child increases significantly);
- consequences of previous diseases;
- negative impact of carcinogenic substances (contact with oncogenic substances such as acetaldehyde, work in conditions of high levels of radiation, negative environmental influences);
- neurofibromatosis (a genetic disease that is accompanied by the appearance of tumors);
- development of Hippel-Lindau syndrome;
- decreased immune system;
- severe stress.
Description example.
Example No. 1[briefly]:
Descriptive part: In…. in the sections of the sacrum, an irregularly shaped multinodular space-occupying formation with clear tuberous contours, a heterogeneous structure, moderately hypointense on T1-VI and iso-slightly hyperintense on T2-VI is determined;
The formation spreads into the pelvic cavity. Dimensions of the space-occupying formation... see.
CONCLUSION : MR picture of a multinodular space-occupying lesion.... sections of the sacrum with spread into the pelvic cavity (differentiate a depository lesion of a secondary nature and a primary process).
Example #2 [briefly]:
Descriptive part : In……. section of the spinal cord, an irregularly elongated shape (along the length of the spinal cord) is determined by a cystic-solid space-occupying formation (with a predominance of the cystic component) with fairly clear, scalloped contours, hyperintense on T2-VI, iso-moderately hypointense on T1-VI, maximum dimensions... … cm.
With intravenous contrast, minimally pronounced accumulation of CV is determined by the above-described space-occupying formation in the form of individual foci.
CONCLUSION : MR picture of an intramedullary cystic-solid space-occupying lesion.
General information
Intramedullary OSM are relatively rare. According to various sources, they account for 2.5 to 8% of cancers in the central nervous system and about 18–20% of spinal tumors. Another name for them is intracerebral, which is associated with their growth from the substance of the spinal cord. Such tumors can either be located directly in the spinal cord, without growing beyond the pial membrane, or emerge from it, filling the subdural space. Often intracerebral tumors are observed in the cervical segments of the spine. Also, about 70% of intramedullary formations are gliomas. However, there are many more varieties of the disease.