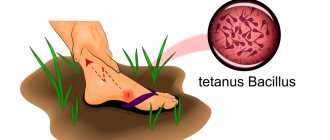
The disease develops when the pathogen enters the body through damage to the skin and mucous membranes (wounds, burns, frostbite). Minor injuries sustained when working with soil on personal plots are especially dangerous.
The incubation period of the disease ranges from 3 to 30 days.
Often, at the onset of a person’s illness, the wound has healed and the sick person does not remember the location and nature of the damage. First, vague symptoms appear: deafness, headaches, loss of appetite, anxiety, a slight increase in temperature, and later a convulsive contraction of the masticatory and facial muscles joins. Then the cramps can spread to the entire muscle. When the occipital muscles and back muscles are affected, the body bends backward. The arms and legs are less affected, but extensor spasms are possible. Particularly dangerous are prolonged spasms of the respiratory muscles, which lead to death.
Emergency prevention of tetanus is carried out for any injuries and wounds with a violation of the integrity of the skin and mucous membranes, frostbite, and burns of the second, third and fourth degrees, animal bites, penetrating injuries or surgical interventions on the gastrointestinal tract, in unvaccinated persons or persons with an unknown vaccination history , out-of-hospital abortions, childbirth outside of medical institutions, gangrene or tissue necrosis of any type, abscesses, carbuncles. Emergency prophylaxis of tetanus is carried out until the 20th day from the moment of injury. The decision to carry out emergency prophylaxis is made based on the conclusion of a doctor at a clinic or hospital.
Immunization is the only reliable way
prevention of tetanus. Vaccinations against tetanus are mandatory and are carried out in accordance with the national calendar of preventive vaccinations from the age of three months, along with vaccinations against diphtheria. Vaccination consists of 3 vaccinations followed by revaccination at the age of 18 months, 7 years, 14 years, and then revaccination is carried out every 10 years until the last revaccination (for life).
Vaccinations against tetanus are carried out in medical institutions (clinics) at the place of residence or work free of charge.
At the same time, against the background of mass immunization in the Russian Federation, the epidemiological features of tetanus have changed: diseases are registered among the adult population, mainly among people over 50 years of age, who account for about 70%; the most affected group are pensioners. Infection occurs in 90% of cases with minor injuries, for which the victims, as a rule, do not seek medical help. But an early visit to the surgical office or emergency department (on weekends and holidays) to a medical institution and emergency tetanus prophylaxis can save your life and the lives of your loved ones.
Immunological control for emergency prophylaxis of tetanus
In the absence of reliable information about vaccinations, the state of tetanus immunity is assessed immediately at the time of the patient’s treatment for injury. The scheme for choosing emergency prophylaxis is based on the results of determining the level of a specific antitoxin in the blood serum of a patient with trauma or on indirect criteria for the fact of vaccination against tetanus (age, gender, absence of contraindications, military service, etc.)
A blood volume of 0.2 ml sufficient for research can be obtained from a wound or simultaneously with taking blood from a finger for any clinical analysis. Blood is collected into a capillary or test tube, which is left at room temperature or in a household refrigerator for 15-20 minutes, after which the supernatant liquid over the red blood cells (serum) is used for serological studies.
When taking blood from a vein, a standard method of separating blood serum is used. The determination of tetanus antitoxin in the patient’s blood serum is carried out in the RPGA in accordance with the instructions for the use of diagnosticums. The minimum titer of tetanus antitoxin, indicating immunization, is 1:20.
Diagnosis of tetanus
With tetanus, laboratory diagnostics are practically meaningless, since at the onset of the disease the toxin is not detected in the blood, antibody titers do not increase (even a lethal dose of the toxin is an insignificant antigenic irritant and does not cause an immune response). The detection of antitoxic antibodies can only indicate a history of vaccinations. Sometimes bacteriological methods are used (histological examination of tissues obtained during surgical treatment of wounds, microscopy of fingerprint smears, inoculation of wound discharge under anaerobic conditions in nutrient media).
However, early diagnosis of this disease is possible only with a careful collection of epidemiological history (injuries, burns, wound infections, surgical interventions received within a time frame that corresponds to the incubation period) and with the active detection of symptoms of the prodromal period. At the height of the disease, there are no problems with diagnosis due to the presence of pathognomonic symptoms. At the same time, there are no deviations from the internal organs, meninges, cerebrospinal fluid, blood and urine.
In some cases, wound examinations are carried out using a bacteriological method:
- histological examination;
- smear microscopy;
- inoculating samples from the wound under conditions similar to the human body.
Based on the signs of the disease during the clinical course of the disease, the diagnosis is made without difficulty or doubt. Despite the fact that the symptoms may be similar to diseases such as rabies, strychnine poisoning and hypofunction of the thyroid glands, lockjaw and a painful smile are unique to tetanus.
Meningitis and meningoencephalitis, traumatic brain injuries, hysterical and epileptic seizures, exacerbations of osteochondrosis also require study when diagnosing tetanus.
Complications of tetanus
Severe complications of tetanus with a high probability of death are asphyxia and cardiac arrest. In addition, tetanus can contribute to the occurrence of bone fractures, muscle ruptures, and compression deformation of the spinal column. A common complication of tetanus is pneumonia, and coronary spasm and myocardial infarction may develop.
During recovery, contractures and paralysis of the third, sixth and seventh pairs of cranial nerves are sometimes noted. In newborns, tetanus can be complicated by sepsis.
Causes of sunworm infection
Tetanus is caused by Clostridium tetani spores entering a wound. In the absence of oxygen, they transform into active forms. The bacterium itself is harmless. But it produces the strongest biological poison - tetanus toxin, which is second only to botulinum toxin in its toxic effect.
Routes of infection with tetanus:
- puncture, cut or laceration wounds;
- splinters, skin abrasions;
- burns/frostbite;
- fractures and animal bites;
- umbilical wound in newborns.
People who need frequent injections are also at greater risk. Any wound (including bites and burns) increases the risk of contracting tetanus.
The most common causes of death from tetanus are:
- choking as a result of prolonged spasm of the vocal cords or respiratory muscles;
- heart failure;
- spine fracture;
- pain shock.
- In children, tetanus is complicated by pneumonia, and at a later date by indigestion and anemia.
Active-passive prophylaxis of tetanus
AC should be administered in a volume of 1 ml, having previously read the instructions for the drug. At the same time, PSCH 250 IU must be injected into another part of the body; in the absence of PSCH, 3000 IU PSS must be injected. Before administering PSS, an intradermal test with horse serum diluted in a ratio of 1:100 is required to determine sensitivity to horse serum proteins (the ampoule is marked in red). An intradermal test cannot be performed if the victim was tested with 1:100 diluted anti-rabies gammaglobulin from horse serum for 1-3 days before the administration of PSS due to the need to administer anti-rabies gammaglobulin.
To perform the test, you need to use an individual ampoule, as well as sterile syringes with 0.1 ml graduations and a thin needle. The serum diluted 1:100 is injected under the skin into the flexor surface of the forearm in an amount of 0.1 ml. The reaction is monitored after 20 minutes. The test is considered negative if the diameter of the swelling or redness at the injection site is less than 1.0 centimeters.
The test is considered positive if the swelling or redness in diameter is 1.0 cm or more. If the skin test is negative, PSS (from an ampoule marked in blue) is injected subcutaneously in a volume of 0.1 ml. If there is no reaction after half an hour, you need to inject the remaining dose of serum with a sterile syringe. During this period, the opened ampoule with PSS should be covered with a sterile napkin.
Note : For people with allergic diseases and reactions to various allergens, as well as those who have previously received drugs containing horse serum (PSS and others) or heterologous gammaglobulins (anti-rabies, anti-encephalitis, etc.), it is best to resort to the administration of antihistamines before administering the main dose of PSS.
Persons with a positive reaction to intradermal injection of 0.1 ml of horse serum diluted 1:100 or who had a reaction to subcutaneous injection of 0.1 ml of PSS cannot undergo further administration of PSS.
Considering that after the administration of PSS and drugs that contain tetanus toxoid, particularly sensitive individuals may develop shock, each vaccinated person must be monitored medically for 60 minutes after vaccination. And the institution where people are vaccinated should be provided with anti-shock therapy in case of need.
What is tetanus?
Tetanus (tetanus) is a severe infectious disease with wound transmission, manifested by damage to the motor structures of the nervous system with the subsequent development of muscle contraction uncontrollable by a person in the form of constant tonic tension and periodic clonic convulsions. Due to the severity of this infectious pathology and high mortality rate, even with modern medical capabilities, most countries carry out specific vaccination, which is included in the compulsory vaccination calendar. However, the incidence, especially in countries with poor sanitary standards and lack of vaccination, remains quite high.
Signs of tetanus
Signs of tetanus that you should pay attention to and go to the hospital immediately include:
- facial muscle spasms;
- "sardonic smile";
- spasms of the muscles of the back and abdomen;
- labored breathing;
- temperature increase;
- increased excitability and insomnia;
- increased sweating;
- asphyxia and apnea;
- impaired renal and urethral function;
- cramps with pain throughout the body.
Tonic and clonic convulsions replace each other and cause severe pain in the patient. The slightest creaking or other loud sound, jolts and even touches cause irritation in the patient and, as a result, another attack of convulsions. Due to severe spasms and contractions of the muscles of the limbs, bone fractures, damage to the diaphragm and respiratory muscles can occur, which causes asphyxia and death from suffocation. Congestion due to poor circulation can affect the subsequent development of pneumonia.
Body temperature directly depends on the strength of convulsive attacks; with frequent and severe convulsions, it can rise to 42ºC. The heart rate increases to 120 beats per minute. Heart sounds are distinct and loud. When blood pressure drops, the prognosis can no longer be reassuring. The removal of waste products becomes more difficult against the background of spasms of the perineal muscles.
Despite the worsening symptoms of tetanus, the person remains conscious and clearly understands the situation throughout the entire course of the disease. No specific changes in internal organs are observed
Types and forms of tetanus disease
Tetanus is dangerous for a person at any age and can affect various organs, causing either sudden death or a slow course of the disease. The following features are noted in this category:
- tetanus in an adult;
- tetanus of a newborn (infection can occur through an umbilical wound that has not yet healed);
- local form of tetanus (affects the muscles or limbs around the wound, causing convulsions);
- neurotetanus;
- cephalic tetanus (affects the muscles of the face, neck, pharynx, leading to death).
Infection with the spore-bearing tetanus bacillus can occur through a wound on the skin during injury, through a suture in the postoperative period, due to burns and after injections or abortion.
According to the form of the disease, tetanus can differ in:
- mild - there is no temperature or it does not rise much, and signs of the disease appear only on the 5-6th day;
- moderate - signs of tetanus are observed within 3-4 days, the body temperature is moderate, the appearance of convulsions occurs periodically throughout the day;
- severe - the disease progresses over 1-2 days, convulsions occur frequently, body temperature rises greatly, sweating and heartbeat increase, breathing and swallowing become more difficult, muscles are toned, facial expressions change dramatically;
- extremely severe - a sharp deterioration in health, body temperature reaches 40ºC, convulsions almost do not stop, the face takes on a bluish appearance, shortness of breath appears and breathing becomes difficult until it stops, death.
Based on the prevalence of tetanus in the human body, several forms are observed - the primary acute form, the ascending form of tetanus and the descending, local development of the disease.