Why does your back hurt after hypothermia?
After the back has been blown, symptoms may also appear in a healthy person, especially if he had previously worked actively physically and sweated.
But more often, hypothermia leads to pain in the spine, which has already undergone pathological changes. Often, it is a visit to the doctor after blowing the lower back with a fan or draft that helps diagnose the initial stages of osteochondrosis. Timely treatment and adherence to preventive measures help to avoid such severe complications of osteochondrosis as vertebral hernia, sequestered hernia, which can lead to complete immobility. If everything is in order with the intervertebral discs, then the appearance of symptoms after the lower back or neck has been blown indicates muscle inflammation - myositis. This disease can also occur due to muscle strain, uncomfortable position while sleeping or working. With myositis, the inflammatory process occurs only in muscle tissue and does not affect the joints and nerve roots of the spinal cord.
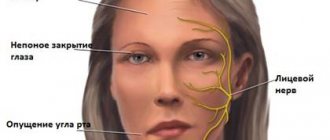
Symptoms of inflammation of the trigeminal nerve
Experts include short-term, but acute and intense pain in different parts of the head as the main symptoms of facial neuralgia. Shooting attacks spread over the entire surface of the face - lips, eyes, nose, upper and lower jaw, gums and tongue.
Patients also report the following symptoms:
- Metallic taste in the mouth
- Muscle weakness
- 2-3 days before facial expressions are affected, pain occurs behind the outer ear, spreading to the face, back of the head and eyes
- Facial asymmetry
- Inability to close the eye on the affected side
- Drooping corner of the mouth
- Dry mouth
- Slurred speech
- Cross-eyed strabismus
- Uncontrollable tearing
- Disorders of taste buds
- Increased drooling
- Facial muscle spasms
- Increased or decreased facial sensitivity
- Temperature increase
Due to discomfort and pain, the patient begins to develop a phobia and increased anxiety. He tries to avoid poses and movements that provoke discomfort.
Treatment of occipital neuralgia
Without influencing the cause of the disorder, it is impossible to completely eliminate its manifestations. The only case where therapy is purely symptomatic is idiopathic occipital neuralgia.
Until research results are obtained, all patients are prescribed symptomatic therapy. Once the root cause is known, treatment is supplemented with remedies aimed at eliminating it.
In most situations, neuralgia can be dealt with directly using conservative therapy. It assumes:
- drug treatment;
- massage;
- exercise therapy;
- physiotherapy.
If left untreated, occipital neuralgia can lead to destruction of nerve tissue and the development of complications, including hair loss and depressive disorders.
Drug therapy
Depending on the nature of the clinical manifestations and causes of nerve irritation, patients may be prescribed:
- muscle relaxants - a group of drugs that help eliminate muscle spasms;
- NSAIDs are drugs that have anti-inflammatory and analgesic properties;
- corticosteroids – have powerful anti-inflammatory properties, prescribed in short courses when NSAIDs are insufficiently effective;
- anticonvulsants – help reduce muscle tone;
- antidepressants – necessary to normalize the psycho-emotional state of patients;
- B vitamins - necessary to improve the condition of nervous tissue and impulse conduction.
In case of a severe attack of pain, a blockade can be performed, which involves pinpoint injections of anesthetics at certain points along the affected nerve.
Physiotherapy
To increase the effectiveness of drug therapy, patients are recommended to undergo courses of physiotherapeutic procedures:
- UVR method involves exposure to mid-wave ultraviolet rays. This leads to an intensification of the release of specific neurotransmitters, which has a beneficial effect on the transmission of nerve impulses. Typically, the course of treatment includes 10 procedures.
- UHF - the procedure is based on the action of high frequency currents, which provoke an improvement in the quality of blood circulation and restoration of the sodium-potassium membranes of nerve cells. Treatment duration is from 15 to 20 sessions of 15 minutes each.
- Electrophoresis is a procedure during which painkillers or other drugs are injected directly into the affected area using an electric current. Traditionally, 10 procedures are prescribed, performed every other day.
- inductometry;
- Laser therapy is a method based on the positive effect of the thermal energy of laser beams on nerve fibers. This effect reduces their sensitivity, which reduces the degree of their irritation and the frequency of attacks. Patients are recommended 10 procedures of 4 minutes each.
- Diadynamic currents - the procedure involves fixing electrodes on trigger points and passing Bernard current through them. This is an ultra-high frequency current, the impact of which provides a rapid decrease in the pain threshold and inhibition of the transmission of nerve impulses. The duration of the treatment course is 5 sessions, performed every other day.
- Spinal traction is a procedure aimed at increasing the size of intervertebral discs and normalizing the position of the vertebrae. It can be performed using dry or underwater methods. Its duration ranges from several minutes to an hour, and the course of treatment includes about 15 sessions. With the dry method, traction is carried out under the influence of its own weight in a vertical or horizontal position. When underwater, the procedure is carried out after the patient is immersed in water. The second method has a more gentle effect on the spine.
Additionally, patients may be recommended reflexology sessions. It has long been noted that targeted effects on biologically active points provoke increased blood circulation, improved lymph flow and a decrease in the severity of pain.
Massage
A properly performed massage helps eliminate pressure on nerve endings, improve blood circulation in the head, and eliminate muscle spasms. The mastoid process and the area under it are exposed to manual intervention. It is important that the procedure is carried out by a qualified specialist. Otherwise, you may accidentally hit trigger points, which will provoke a new attack of pain.
Traditionally, a course consisting of 12–14 procedures is prescribed. The duration of each of them is about a quarter of an hour.
Therapeutic exercise (physical therapy)
Regular exercise therapy classes according to individually designed programs will help normalize the functioning of the cervical spine. They are especially important for osteochondrosis, as they allow you to accelerate the processes of natural restoration of cartilage tissue and eliminate the prerequisites for compression of nerves.
For each patient, a set of exercises is selected separately, taking into account the characteristics of existing diseases. They should be performed daily at least once a day. On average, one physical therapy session takes about 20–30 minutes.
All exercises are performed carefully, without sudden movements. If a new attack of neuralgic pain or discomfort in the cervical spine occurs, you should immediately stop exercising and consult a doctor as soon as possible to understand the causes of pain and change the nature of the exercises to a more gentle one.
Diagnosis of inflammation of the facial nerve
If the doctor is properly qualified, then only based on the patient’s complaints will he be able to make a diagnosis and identify the severity of the pathological process. But even if the clinical picture is typical, the patient will have to undergo a series of diagnostic examinations:
- take blood and urine tests;
- undergo magnetic resonance imaging;
- do electroneurography.
The results obtained will help determine what treatment for inflammation of the facial nerve will be. In addition, such an examination will allow the doctor to identify the body’s perception of non-steroidal anti-inflammatory drugs - these are the drugs that will be used for therapy.
What are the benefits of going to the clinic?
The main advantage of visiting a medical facility for back pain is the opportunity to undergo an accurate diagnosis. After all, pain after hypothermia can occur not only with myositis, but also with much more serious diseases of the spine: protrusions, ordinary and sequestered hernia.
Having undergone diagnostics using modern highly informative devices, you will know exactly the cause of pain after hypothermia. If the pain is caused not by simple muscle inflammation, but by degenerative changes in the structure of the intervertebral discs, then you will be prescribed treatment that will help prevent further progression of the disease, which, without timely treatment, can lead to disability.
But it can blow out the lower back even with a healthy spine. In this case, treatment prescribed by a doctor will help you quickly cope with the disease and return to your normal rhythm of life. In this case, the likelihood of the disease becoming chronic will be minimized.