Facial neuritis is an inflammation that can lead to distortion and partial paralysis of the face.
Typically, inflammation of the facial nerve occurs unexpectedly and takes you by surprise. Its development is happening rapidly. If in this situation you delay with medical help, then paralysis and facial distortion may remain forever. But this can be almost completely avoided if treatment is carried out in time and correctly,
At the Tibet Clinic, the effectiveness of treatment for facial neuritis exceeds 97-98%. Positive results are achieved relatively quickly. Their success is explained by the extensive experience of our doctors and complex therapy of oriental medicine.
Facial neuritis – cold disease
In Tibetan medicine, facial neuritis refers to diseases of the Wind system, or Rlung (Tib.). The main reasons why such diseases occur are icy, piercing winds, sudden cooling, combined with psycho-emotional problems.
This explains the fact that inflammation of the facial nerve often occurs in cold, windy weather against a background of nervous and emotional stress, and mental overload. A provoking factor for inflammation can be, for example, a strong draft or a flow of cold air from an air conditioner.
general information
The trigeminal nerve consists of sensory and motor fibers. It originates in the structures of the brain and is divided into three branches:
- ophthalmic: responsible for the eye, forehead and upper eyelid;
- maxillary: innervates the area from the lower eyelid to the upper lip;
- mandibular: involves the chin, lower jaw, lips and gums.
With neuralgia, one or more branches of the trigeminal nerve are affected, which determines the main symptoms of the pathology. People over 45 years of age are most susceptible to the disease, and women get sick more often than men.
Make an appointment
Causes
The causes of trigeminal neuralgia can be of different nature:
- compression of the entire trigeminal nerve or its branches against the background of: enlargement of the arteries or veins of the brain (aneurysms, atherosclerosis, strokes, increased intracranial pressure due to osteochondrosis, congenital developmental features);
- tumors of the brain or facial tissues in close proximity to nerve fibers;
- congenital anomalies of bone structure, narrowed openings through which nerve branches pass;
- injuries of the skull, facial area: bone fractures, post-traumatic scars of soft tissues;
- proliferation of scar tissue after injury, surgery, inflammation;
The risk of developing trigeminal neuralgia increases significantly:
- over the age of 50;
- against the background of mental disorders;
- with regular hypothermia;
- with insufficient intake of nutrients and vitamins into the body (anorexia, bulimia, malabsorption, etc.);
- with regular overwork, stress;
- for helminthic infestations and other helminthiases;
- for acute infections: malaria, syphilis, botulism, etc.;
- for chronic inflammation in the oral cavity (caries, gingivitis, abscesses, etc.);
- against the background of autoimmune lesions;
- with excessive exposure to allergies;
- for metabolic disorders.
Forecast
Full recovery after suffering a pathology is possible only if all the specialist’s instructions are followed conscientiously. A favorable prognosis is observed in 60-70% of all cases of pinched facial nerve.
Neuritis, which threatens with adverse consequences, can be suspected by the following symptoms:
- rapid development of paralysis ;
- dry eyes ;
- lack of positive dynamics in disease therapy for 3 weeks.
Pinched facial nerve (or neuritis) is a problem whose causes are still not understood. The pathology is not accompanied by a life-threatening condition, but has many consequences if you do not contact a specialist in a timely manner.
Only early diagnosis of neuritis, its proper treatment and compliance with all doctor’s recommendations will give a chance for a successful outcome of the pathology.
Symptoms
The main characteristic symptom of trigeminal neuralgia is paroxysmal pain. It comes suddenly and in its intensity and speed of spread resembles an electric shock. Typically, intense pain forces the patient to freeze in place, waiting for relief. The attack can last from a few seconds to 2-3 minutes, after which there is a period of calm. The next wave of pain may come within hours, days, weeks or months.
Over time, the duration of each attack of neuralgia increases, and periods of calm are reduced until a continuous aching pain develops.
The provoking factor is irritation of trigger points:
- lips;
- wings of the nose;
- eyebrow area;
- middle part of the chin;
- cheeks;
- area of the external auditory canal;
- oral cavity;
- temporomandibular joint.
A person often provokes an attack when performing hygiene procedures (combing hair, caring for the oral cavity), chewing, laughing, talking, yawning, etc.
Depending on the location of the lesion, the pain takes over:
- the upper half of the head, temple, orbit or nose if the ophthalmic branch of the nerve is affected;
- cheeks, lips, upper jaw – if the maxillary branch is affected;
- chin, lower jaw, as well as the area in front of the ear - with neuralgia of the mandibular branch.
If the lesion affects all three branches or the nerve itself before it is divided, the pain spreads to the entire corresponding half of the face.
Painful sensations are accompanied by other sensory disturbances: numbness, tingling or crawling sensations. Hyperacusis (increased hearing sensitivity) may be observed on the affected side.
Since the trigeminal nerve contains not only sensory, but also motor pathways for the transmission of impulses, with neuralgia the corresponding symptoms are observed:
- twitching of facial muscles;
- spasms of the muscles of the eyelids, masticatory muscles;
The third group of manifestations of neuralgia are trophic disorders. They are associated with a sharp deterioration in blood circulation and lymph outflow. The skin becomes dry, begins to peel, and wrinkles appear. Local graying and even hair loss in the affected area is observed. Not only the scalp suffers, but also the eyebrows and eyelashes. Impaired blood supply to the gums leads to the development of periodontal disease. At the time of the attack, the patient notes lacrimation and drooling, swelling of the facial tissues.
Constant spasms of muscle fibers on the diseased side lead to facial asymmetry: narrowing of the palpebral fissure, drooping of the upper eyelid and eyebrow, upward movement of the corner of the mouth on the healthy side or drooping on the diseased side.
The patient himself gradually becomes nervous and irritable, and often limits himself to food, since chewing can cause another attack.
Algorithm for patient management in the acute phase (first 30 hours)
There is a limited time window of up to 30-48 hours to make the most correct decision - to recognize the fact of damage to the alveolar and/or lingual nerve after implantation, endodontic treatment or removal of mandibular third molars.
Report by reference Khawaja N, Renton T Case studies on implant removal influencing the resolution of inferior alveolar nerve injury. Br Dent J. 2009 Apr 11;206(7):365–370 suggests that early removal of the causative implant (within the first 30 hours) results in maximum recovery, but the evidence remains weak.
Suggested protocol based on available evidence:
- Homecheck - The attending physician should contact the patient between 6 and 24 hours after surgery to determine the presence/absence of persistent partial neuropathy after local anesthesia has worn off. This contact is based on the relationship between doctor and patient, which is achieved through signed informed consent.
- Confirm the presence of neuropathy . If the neuropathy affects +/- most of the dermatome, severe nerve injury should be considered, which will be accompanied by neuropathic severe pain if not treated immediately.
- Admit the damage and apologize. An apology is NOT an admission of guilt.
- Additional CT scans or radiography are not necessary or valuable for decision-making in cases of implantation, but are absolutely necessary in cases of third molar extraction.
- Initiate treatment for implant-related nerve damage: - Consider removal of the implant within 30 hours of implantation or sooner; - early therapeutic treatment.
- Acute phase - nerve damage during surgery - Implant removal, immediate nerve restoration +/-.
Diagnostics
A neurologist diagnoses trigeminal neuralgia. During the first visit, he carefully interviews the patient to find out:
- complaints: nature of pain, its intensity and localization, conditions and frequency of attacks, their duration;
- medical history: when pain attacks first appeared, how they changed over time, etc.;
- life history: the presence of chronic diseases, previous injuries and operations is clarified, special attention is paid to dental diseases and interventions.
A basic examination includes assessing the condition of the skin and muscles, identifying asymmetry and other characteristic signs, checking the quality of reflexes and skin sensitivity.
To confirm the diagnosis, the following is carried out:
- MRI of the brain and spinal cord with or without contrast: allows you to identify tumors, consequences of injuries, vascular disorders; sometimes the study is replaced by computed tomography (CT), but it is not as informative;
- electroneurography: study of the speed of nerve impulse transmission through fibers; allows you to identify the fact of nerve damage, assess the level of the defect and its features;
- electroneuromyography: not only the speed of impulse passage along the nerve bundle is studied, but also the reaction of muscle fibers to it; allows you to assess nerve damage, as well as determine the sensitivity threshold of trigger zones;
- electroencephalography (EEG): assessment of the bioelectrical activity of the brain.
Laboratory diagnostics includes only general studies to exclude other causes of painful attacks, as well as to assess the condition of the body as a whole (usually a general blood and urine test is prescribed, as well as a standard set of biochemical blood tests). If the infectious nature of the disease is suspected, tests are carried out to identify specific pathogens or antibodies to them.
Additionally, consultations with specialized specialists are prescribed: ENT specialist (if there are signs of nasopharynx pathology), a neurosurgeon (if there are signs of a tumor or injury), and a dentist.
Treatment of trigeminal neuralgia
Treatment is aimed at:
- to eliminate the cause of damage;
- to alleviate the patient's condition;
- to stimulate the restoration of nerve structures;
- to reduce the excitability of trigger zones.
Properly selected treatment can reduce the frequency, intensity and duration of pain waves, and ideally achieve stable remission.
Drug treatment
Trigeminal neuralgia requires complex treatment using drugs from several groups:
- anticonvulsants (carbamazepine and analogues): reduce the excitability of nerve fibers;
- muscle relaxants (baclofen, mydocalm): reduce muscle spasms, improve blood circulation, reduce pain;
- B vitamins (neuromultivit, milgamma): stimulate the restoration of nerve fibers, have an antidepressant effect;
- antihistamines (diphenhydramine): enhance the effect of anticonvulsants;
- sedatives and antidepressants (glycine, aminazine): stabilize the patient’s emotional state.
For severe pain, narcotic analgesics may be prescribed. Previously, drug blockades (injecting the problem area with anesthetics) were actively used, but today this method of treatment is almost never used. It contributes to additional damage to nerve fibers.
Treatment of the root cause of the disease is mandatory: elimination of dental problems, taking medications to improve cerebral circulation, etc.
Physiotherapy and other non-drug methods
Non-drug methods complement drug therapy well and help stabilize patients’ condition. Depending on the condition and concomitant diseases, the following may be prescribed:
- ultraviolet irradiation: inhibits the passage of impulses along nerve fibers, providing an analgesic effect;
- laser therapy: reduces pain;
- UHF therapy: improves microcirculation and prevents muscle atrophy;
- electrophoresis with analgesics or antispasmodics to relieve pain and relax muscles;
- diadynamic currents: reduce the conductivity of nerve fibers, significantly increase the intervals between attacks;
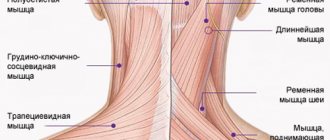
- massage of the face, head, cervical-collar area: improves blood circulation and lymph outflow, improving tissue nutrition; must be carried out with caution so as not to touch trigger zones and provoke an attack; the course is carried out only during the period of remission;
- acupuncture: helps relieve pain.
Surgery
The help of surgeons is indispensable when it is necessary to eliminate nerve compression. If indicated, the following is carried out:
- removal of tumors;
- displacement or removal of dilated vessels pressing on the nerve (microvascular decompression);
- expansion of the bone canals in which the branches of the nerve pass.
A number of operations are aimed at reducing nerve fiber conductivity:
- exposure to a gamma knife or cyber knife;
- balloon compression of the trigeminal node: compression of the node using an air-filled balloon installed in close proximity to it, followed by death of the nerve fibers; surgery often leads to partial loss of sensation and decreased muscle movement;
- resection of the trigeminal node: rarely performed due to the complexity and large number of complications.
Make an appointment
Pharmacological therapy in the acute phase (first 30 hours) and intermediate phase (up to 4-8 weeks)
Pharmacological treatment of acute nerve fiber injuries includes the use of corticosteroids and non-steroidal anti-inflammatory drugs.
- Glucocorticosteroids – adrenocorticotropic hormone has been shown to inhibit central axon sprouting, reduce ectopic discharges in damaged sensory axons, and prevent neuroma formation. Seo K. et al.: Efficacy of steroid treatment for sensory impairment after orthognathic surgery. J Oral Maxillofac Surg 2004;62:1193-1201. Drug of choice - Dexamethasone - 8-12 mg/day for one week - Dexamethasone not only minimizes neuropathy after nerve injury when administered in high doses for one week after injury, but is especially recommended due to its significant anti-inflammatory effect compared to other corticosteroids. The recommendation is to prescribe a decreasing dose of dexamethasone (from high to low) for 5-7 days after a trigeminal nerve injury. Galloway EB, Jensen RL, Dailey AT, Thompson BG, Shelton C. Role of topical steroids in reducing dysfunction after nerve injury. The Laryngoscope 2000;110(10):1907-10. Kraut RA, Chanal O. Management of patients with trigeminal nerve injuries after mandibular implant placement. J Am Dent Assoc 2002;133:1351-1354.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are the best inhibitors of prostaglandin synthesis from damaged peripheral nerve endings. Prostaglandins released as a result of peripheral nerve injury sensitize peripheral nociceptor fibers and central neurons. Muller HW, Stoll G. Nerve injury and regeneration: basic insights and therapeutic interventions. Cun Opin Neurol 1998;11:557-559. Thus, maintaining therapeutic levels of NSAIDs in the blood as an adjunct to corticosteroids for 1-3 weeks after injury is very useful during the acute and intermediate phase of trigeminal nerve repair. Because any change in sensation may be caused by an inflammatory response, postoperative treatment with steroids followed by high-dose nonsteroidal anti-inflammatory drugs is given as soon as possible after any nerve injury. The drug of choice is Ibuprofen - 600 - 800 mg three times a day for three weeks (after finishing dexamethasone!). If necessary, two to three weeks after the injury, based on a repeat neurosensory examination, the doctor may prescribe an additional three weeks of taking NSAIDs if there are no signs of gastrointestinal disorders.
- Additional pharmacological agents - antidepressants, anticonvulsants, antisympathomimetic drugs, etc. Caution should be exercised with these types of pharmacological treatments, as they must be prescribed and monitored by a doctor who is familiar with the side effects of these drugs and has experience in treating nerve damage.
- Supportive pharmacological agents: - Neurorubin-Forte Lactab - one tablet twice a day for 4 weeks - contains high doses of vitamins B1, B6, B12, which play an important role in ensuring optimal metabolism in nerve cells. In high doses - has a weak analgesic effect; - Nucleo CMF Forte - one tablet twice a day for 20 days - Cytidine 5-monophosphate takes part in the synthesis of a complex of lipids that form the sphingomyelin membrane as the main component of the myelin sheath; - myogymnastics.
Complications
Without treatment, trigeminal neuralgia gradually progresses. Over time, a pathological pain focus forms in one of the parts of the brain. As a result, the pain covers the entire face, is provoked by any minor irritant and even the memory of an attack, and subsequently becomes permanent. Vegetative-trophic disorders progress:
- irreversible atrophy of the facial muscles is formed;
- teeth become loose and begin to fall out due to advanced periodontal disease;
- baldness is increasing.
Due to constant pain, the patient's sleep is disturbed and severe depression develops. In severe cases, patients may commit suicide.
Consequences
After an illness, nerve conductors take a long time to heal. This fact complicates treatment. Many patients, not seeing noticeable improvements, give up and do not follow the doctor’s instructions.
Failure to comply with therapeutic prescriptions leads to a number of complications:
- atrophy of the facial muscles;
- tightening of facial muscles;
- involuntary twitching of certain parts of the face;
- synkinesis;
- conjunctivitis.
To prevent these consequences of the disease, it is necessary to perform daily massage and gymnastics on the inflamed side of the face. Conjunctivitis occurs due to the patient's inability to close their eyes. To avoid inflammation of the eye membranes, it is important to use drops.
Prevention
Prevention of trigeminal neuralgia is a set of simple measures that significantly reduce the risk of developing pathology. Doctors recommend:
- undergo regular preventive examinations;
- at the first signs of the disease, seek help (the sooner treatment is started, the greater its effect will be);
- eat right, get the required amount of vitamins, minerals, unsaturated fatty acids;
- regularly engage in light sports and gymnastics;
- get enough sleep and rest;
- minimize stress and physical overload;
- avoid hypothermia and harden yourself;
- to refuse from bad habits.
Treatment at the Energy of Health clinic
If you or your relative are bothered by severe pain in one or another part of the face, the neurologists of the Health Energy clinic will come to the rescue. We will conduct a full diagnosis to identify the causes of the pathology and prescribe comprehensive treatment. At your service:
- modern drug regimens to reduce the frequency and intensity of attacks;
- physiotherapeutic procedures: magnetotherapy, laser therapy, electrophoresis, phonophoresis, etc.;
- delicate therapeutic massage;
- acupuncture;
- help from a psychologist if necessary.
Advantages of the Health Energy Clinic
The Health Energy Clinic is a multidisciplinary medical center where every patient has access to:
- screening diagnostic programs aimed at early detection of diseases and pathologies;
- targeted diagnostics using modern equipment and laboratory tests;
- consultations with experienced specialists, including foreign ones;
- modern and effective comprehensive treatment;
- necessary certificates and extracts;
- documents and appointments for spa treatment.
Trigeminal neuralgia is a serious pathology that can seriously disrupt a person’s normal lifestyle. Don't let pain and fear take over your thoughts, get treatment at Health Energy.
Improvement criteria
One of the key criteria for improvement is a significant reduction in the size of the neuropathic area of the sensory dermatome, detected during control neurosensory examinations, which indicates spontaneous recovery of the nerve, which in most cases is partial.
In cases of lingual nerve neuropathy, a common finding is a residual neuropathic area on the lateral surface of the tongue adjacent to the teeth.
After using the 5% lidocaine patch, patients with IANI should experience an average reduction in mean pain levels on the PainDetect by half.
A decrease in the level of paresthesia is usually accompanied by an improvement in mechanosensory function, which ultimately leads to an overall improvement in the quality of life of such patients, however, it is very important to inform patients that treatment may not fully restore mechanosensory functions such as eating, drinking, articulation, etc., or special sensory functions, i.e. taste.
It is very important for patients with speech problems to have access to speech therapy.
A clinical psychologist can help patients cope with pain and allow the patient to lead as normal a life as possible, but it must be understood that a clinical psychologist cannot reduce the actual level of perceived pain.
Surgery in the late phase (3–6 months after nerve injury) should be the last option and only in cases where there is minimal or no dynamics of the large neuropathic area, poor mechanosensory function persists, and moderate to high levels of daily pain. After reparative surgery, exacerbation may occur in the form of increased pain from intermittent to constant, about which patients should be warned in advance and have the opportunity to agree or refuse the operation.