Chronic cerebrovascular accident (cerebral vascular insufficiency) is characterized by a decrease in blood supply to the brain. This condition is very common among older people in developed countries due to the high prevalence of atherosclerosis. In most cases, the carotid artery is damaged. A pair of carotid arteries, one on each side of the neck, running parallel to the jugular vein, are the main arteries that supply blood to the brain.
As a rule, cerebral vascular insufficiency develops in the area of the bifurcation of the carotid artery - the splitting of the carotid artery into internal and external branches. This splitting is similar to a stream that has split into two streams. In bifurcation, as well as during bifurcation in a water flow, accumulation of slag occurs. Severe symptoms begin to appear in most cases only when the artery blockage reaches 90 percent. This situation is similar to what happens with coronary heart disease.
Symptoms of chronic cerebrovascular accident are caused by decreased blood flow and oxygen supply to the brain. Stopping the flow of blood and oxygen leads to a stroke. The official definition of stroke is "loss of nerve function for at least 24 hours due to lack of oxygen." Some strokes are mild; others result in paralysis, coma, or speech impairment, depending on what part of the brain is involved. Mini-strokes, or transient ischemic attacks, can result in loss of nerve function for an hour or more, but less than 24 hours. TIAs can lead to transient symptoms of cerebral vascular insufficiency: dizziness, ringing in the ears, blurred vision, confusion, and so on.
Atherosclerosis is one of the main causes of cerebrovascular insufficiency. As this process progresses, high cholesterol levels combined with inflammation in the walls of the arteries in the brain can cause cholesterol to accumulate on the vessel wall in the form of a thick, waxy plaque. This plaque can restrict or completely prevent blood flow to the brain, causing stroke, transient ischemic attacks, or dementia, which can lead to a variety of other health complications.
The most common forms of cerebrovascular disease of the brain are thrombosis (40% of cases) and cerebral embolism (30%), followed by cerebral hemorrhages (20%).
Another form of cerebrovascular disease includes aneurysms. In women with defective collagen, weak key arterial branch points result in ridges with a very thin endothelial covering that can easily rupture with minimal increase in blood pressure. It can also occur with poor capillaries caused by cholesterol deposition in tissues, especially in hypertensive patients with or without dyslipidemia. If bleeding occurs, the result is a hemorrhagic stroke in the form of subarachnoid hemorrhage, intracerebral hemorrhage, or both.
A drop in blood pressure during sleep can lead to a marked decrease in blood flow in narrowed blood vessels, causing ischemic stroke in the morning. Conversely, a sharp increase in blood pressure due to daytime agitation can lead to rupture of blood vessels, resulting in intracranial hemorrhage. Cerebrovascular disease primarily affects people who are elderly or have a history of diabetes, smoking, or coronary heart disease.
Etiology of transient cerebrovascular accidents
Transient disturbance of cerebral blood flow (TCI) is an acute disturbance of the blood circulation of the brain, which is accompanied by the appearance of focal, cerebral or mixed symptoms.
PNMK occurs in 30% of the population.
The main causative factors in the development of PNMK are: hypertension, symptomatic hypertension, atherosclerosis, vasculitis with autoimmune connective tissue lesions, heart defects, acute cardiac disorders (myocardial infarction, acute coronary syndrome, exertional angina), osteochondrosis of the cervical spine, vertebral artery syndrome .
The following forms of PNMK are distinguished: transient ischemic attacks (TIA) and hypertensive crises. PNMK of the TIA type is a short-term disturbance of blood flow and is not accompanied by pronounced destructive changes in brain tissue, but sometimes TIA can lead to the formation of cysts of small diameter.
Typically, TIA-type PNMK is reversible and this is due to the large compensatory capabilities of the brain, but it tends to form “silent” zones.
PNMK of the TIA type may also include diffuse atrophic changes in brain tissue, which can serve as a trigger in the development of ischemic stroke.
One of the causes of PNMC may be congenital vascular anomalies, for example, coarctation of the aorta, hypo- or aplasia of the arteries, pathological tortuosity of the choroid plexuses.
Severe spasm of the neck muscles, pathological compression from the outside by a growing tumor, enlarged lymph nodes can play an important role in the formation of PNMK.
Blood supply to the brain
Brain structures receive blood supply from the vertebrobasilar vascular system (VBB) and the carotid system.
The carotid system gives rise to the anterior and middle cerebral arteries, which supply:
- frontal, parietal and temporal lobes;
- striopallidal subcortical structures;
- inner capsule.
Areas of blood supply to the vertebrobasilar region:
- brain stem;
- cerebellum;
- occipital lobe;
- partially parietal and temporal regions;
- thalamus.
Predominant discirculation in the vertebrobasilar system is often associated with the anatomical features of the vertebral arteries, which are located in the canal of the cervical vertebrae. Osteochondrosis of this department, neck injuries and vertebral displacements deform blood vessels and prevent adequate blood supply to the brain.
The two blood supply basins are connected by communicating arteries, which close the Circle of Willis. It is believed that such a closed system is a manifestation of compensatory mechanisms necessary when one of the arteries is excluded from the bloodstream. If the communicating vessels do not fully function or are completely absent, the circle of Willis is considered open or open.
Pathogenesis of transient cerebrovascular accidents
If the patency of the vessels of the brain or vessels of the neck is impaired, for example, with atherosclerosis, vasculitis, thrombosis, blood circulation in the brain tissue may become difficult.
This leads to ischemia of brain tissue and activation of metabolism with the production of under-oxidized products that trigger the destruction of phospholipids in cell membranes.
The result of such exposure is the death of brain cells with the development of atrophic diffuse foci, which leads to dysfunction of the nervous system and is manifested by various symptoms.
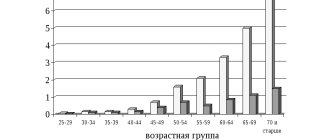
Causes of the disease
Cerebrovascular insufficiency mainly occurs in older people. However, recently there has been a sad trend towards “rejuvenation” of the disease. Moreover, the causes of the development of the disease often do not depend on the patient’s age. The main predisposing factors include:
- instability of blood pressure (hypertension, hypotension);
- atherosclerosis;
- cardiac pathology;
- vasculitis;
- blood rheology disorders;
- diabetes;
- chronic intoxication;
- physical inactivity;
- obesity;
- stressful situations.
The causes of the pathology may also be hidden in a person’s genetic predisposition to the development of the etiological components of the disease (hereditary forms of hypertension, diabetes mellitus, hyperlipidemia).
Development mechanisms
Insufficient cerebral blood flow provokes a number of morpho-functional disorders that play a major role in the development of the disease. Lack of adequate oxygen supply to cells:
- reduces the activity of redox processes;
- inhibits adenosine phosphate synthesis;
- inhibits the aerobic form of glycolysis;
- activates the anaerobic pathway for glucose utilization;
- disrupts the activity of ion transport through the cell wall.
These processes lead to the formation of small point foci of ischemia, diffusely scattered in the brain tissue. The degree of hypoxic damage to nervous tissue is determined by the causes of the pathological process, the severity of these factors, the duration of their influence and the state of the body itself (acid-base balance, blood gas levels).
Clinical manifestations
The clinical picture of the disease depends on the duration of the disease and the vascular basin where discirculation predominantly occurs. Due to the fact that foci of ischemia are most often localized diffusely, the symptoms of the disease may include several components.
Currently, a gradation of chronic cerebrovascular pathology into three degrees is used . This division reflects the severity of the main manifestations and severity of the disease.
Stage I insufficiency of blood supply to the brain is characterized by the presence of diffuse neurological symptoms, which do not allow identifying the leading neurological syndrome. As a rule, a small number of small foci of ischemia are observed that are not capable of leading to pronounced functional disorders. Patients report complaints of general weakness, periodic headaches, dizziness, absent-mindedness, memory loss, and fatigue. A neurological examination reveals pyramidal insufficiency with asymmetry of tendon and periosteal reflexes, symptoms of mild dysfunction of the vestibulo-cerebellar system, and autonomic manifestations.
Stage II of chronic cerebrovascular pathology is diagnosed when a focal symptom complex of the disease is identified. At this stage the following is most often formed:
- cerebellar syndrome. It manifests itself as static and dynamic ataxia, instability in the Romberg position, dysmetria and impaired performance of coordination tests.
- pyramidal disorders. Identified in the presence of paresis of the limbs with the manifestation of pathological reflexes;
- strio-pallidal disorders. Most often, vascular parkinsonism is diagnosed with a specific tremor of the “counting coins” or “rolling pills” type, increased muscle tone according to the extrapyramidal variant and hypokinesia;
- sensory disturbance syndrome. Occurs when the cerebral conductors of superficial and deep sensitivity are damaged. Symptoms of hypoesthesia, perversion of sensitivity, hyperpathy, and decreased two-dimensional spatial sense are formed.
- cognitive dysfunction. It manifests itself as a pathology of memory, attention, and thinking. For stage II chronic cerebral ischemia, severe cognitive decline is not typical.
III degree of chronic brain failure is diagnosed with severe cognitive pathology with the development of dementia. Patients are usually disoriented and not critical. During this period, symptoms of emotional disorders in the form of apatho-abulic syndrome and aggressive behavior are characteristic. Extensive areas of ischemia can act as an epileptic focus with the development of periodic somato-motor or somato-sensory paroxysms. The symptoms of the disease at this stage are practically impossible to control with medications. Its treatment comes down to social rehabilitation and environmental adaptation of the patient.
Patients with chronic impairment of cerebral hemodynamics of the third degree require constant monitoring by relatives and doctors.
Cerebral blood flow is directly related to the quality of peripheral circulation. With a decrease in brain perfusion, a clinical manifestation of a symptom complex of vascular disorders in the periphery is possible. Thus, chronic forms of cerebral dyscirculation may be associated with the development of peripheral Raynaud's syndrome.
There is a concept of “initial manifestations of cerebrovascular insufficiency.” Such a diagnosis is valid in the presence of subjective complaints typical of cerebral dyscirculation, in the presence of a normal neurological status.
Clinic of transient cerebrovascular accidents
Transient disorders of cerebral circulation, the symptoms of which can be divided into focal, cerebral or mixed.
Focal symptoms: loss of sensitivity, hypoesthesia or hyperesthesia of the skin of the face, limbs or torso.
Impaired motor activity with the development of paresis of the central type, which involves the muscles of the hands and feet.
Muscle hypotonia and decreased muscle strength are characteristic of TIA-type PMI. These processes can lead to the development of partial epileptic seizures.
Pathological reflexes may appear.
Visual impairment of the optic-pyramidal syndrome type appears with the development of monocular blindness on the side of the vessel occlusion.
General cerebral symptoms: nausea, vomiting, hiccups. Tinnitus, dizziness, imbalance, horizontal nystagmus, abnormal head position, photopsia, visual field defects, these symptoms may indicate a cerebrovascular accident.
Disorders of the bulbar part of the brain may occur: dysphonia, dysphagia, dysarthria.
Sudden attacks of muscle hypotension and immobility may occur with preserved consciousness.
Hypertensive crises are the result of a sharp increase in blood pressure, and are accompanied by vegetative symptoms.
Excursion into physiology
The uninterrupted supply of substances necessary for the nerve cells of the brain and the cleansing of waste are carried out by the cerebral circulatory system, where arterial blood carries oxygen and nutrition to the brain, and venous blood removes toxins and metabolic products.
The vessels of the brain have a unique, perfect structure that ideally regulates blood flow, ensuring its stability. They are designed in such a way that with an increased flow of blood into large vessels, the strong pulse impulse of the blood coming from the heart is weakened due to numerous bends (siphons) of the vessels along the vascular bed, which contribute to the pressure drop and smoothing of the pulsating blood flow. Due to complex regulatory mechanisms, when total blood pressure increases, the pressure in the brain remains stable for a long time. Regulatory systems allow blood flow to be redistributed from parts of the brain with less load to areas with increased brain activity.
The brain has an autonomous regulatory system, which allows it to be in a healthy functional state and control the processes of continuous adaptation of the body to constantly changing conditions of the external and internal environment. In a state of functional rest, the brain receives 750 ml of blood per minute, which is 15% of cardiac output. In children, blood flow activity is 50–55% higher, and in elderly people it is 20% lower than in adults.
It should be noted that the gray matter of the brain (cell bodies of neurons) is supplied with blood more intensively than the white matter (conducting pathways), which is due to greater cell activity. Thus, during intense mental work, local blood flow in the cerebral cortex can increase 2–3 times compared to the resting state.
The brain has the richest capillary network. Nerve cells are not only intertwined, but also penetrated by capillaries. The vessels of the brain are connected to each other by collaterals (“bridges”). Arterial collateral circulation of the brain, important for maintaining normal blood flow, plays a particularly significant role in compensating for circulatory disorders when one of the cerebral arteries is blocked.
With a high intensity of blood flow in the vessels of the brain, the blood pressure in them is maintained relatively constant. A complex chain of regulatory mechanisms protects the brain from a drop in blood pressure and hypoxia (decreased oxygen). Along the path of blood flow to the brain, there are many sensitive cells (pressoreceptors, chemoreceptors) that can respond to blood pressure and regulate heart rhythm and vascular tone.
The activity of the vasomotor centers of the brain is associated not only with nervous and humoral regulation mechanisms, but also with the autonomic regulation system, which allows, despite significant fluctuations in total blood pressure, to maintain cerebral blood flow at a constant level.
Thus, cerebral circulation is provided with complex regulatory mechanisms that make it possible to maintain a constant supply of the substances it needs.
With excessive blood supply to the brain, excessive hydration (fluid accumulation) may occur, followed by the development of edema and damage to vital centers that are incompatible with life. The cause of excess blood supply can be, for example, an increase in systemic blood pressure to 160–170 mm Hg. Art. and higher.
In the problem of impaired blood supply to the brain, much attention is paid to arteries. But venous circulation is no less important. The veins carry out the removal of waste substances (toxins) with the blood - that is, cleansing the brain. Thanks to these vessels, constant intracranial pressure is maintained.
Violation of the venous outflow leads to stagnation of blood and accumulation of fluid in the brain, causes hydrocephalus with compression of the brain centers, and contributes to the occurrence of phlebitis and thrombophlebitis.
There is one more feature of the cerebral veins that must be taken into account. The wall of a venous vessel in the brain does not have a valve apparatus, unlike, for example, the veins of the extremities (valves help withstand loads by moving blood upward and preventing it from moving in the opposite direction). Therefore, venous blood in the vessels of the brain passes freely in both directions, depending on the pressure that arises. This creates a danger of rapid spread of infection from the sinuses and eye sockets, which is facilitated by the atomic structure of the nose and its paranasal sinuses, located in close proximity to the brain. When coughing, venous pressure increases, reverse venous flow, congestion, and brain hypoxia become possible. There are known cases of loss of consciousness during a coughing attack in the presence of a chronic respiratory tract disease and in young children when they “go into a fit” of coughing during illness and crying and screaming until they cough.
It becomes clear why long-term respiratory problems, accompanied by constant swelling and coughing, can cause cerebrovascular accidents. Because they not only cause brain hypoxia, but also disrupt venous outflow and, being a constant source of infection, contribute to its penetration into the brain.
An ophthalmologist, for example, can observe manifestations of congestion in the brain (dilated, blood-filled vessels of the fundus). But this is also visible to the naked eye: red, puffy eyes after sleep (due to drinking alcohol the night before, overeating at night, lack of sleep) are a symptom of congestion in the brain.
After a brief excursion into physiology, it becomes clear that the reasons for the deterioration of cerebral circulation may be associated with disturbances in the flow of blood to the brain and the outflow of blood from the brain.
Diagnosis of transient cerebrovascular accidents
The diagnosis is made on the basis of the patient’s complaints, medical history and illness, the presence of concomitant pathologies, clinical examination, laboratory and functional research methods.
The diagnosis of PNMK is made when stenosis of intracranial arteries is excluded; for this purpose, ultrasound scanning of vessels, MR angiography, and contrast angiography are used.
A coagulogram is examined, and a CT and MRI of the brain is also performed.
The diagnosis of PNMK should exclude subarachnoid hemorrhage. The diagnosis of PNMK can be made as a concomitant pathology.
Diagnostics
To confirm the diagnosis, a number of diagnostic procedures are necessary. On the one hand, this makes it possible to clarify the presence of the main morphological substrate of the disease (foci of ischemia), as well as to identify predisposing factors and the degree of their manifestations. On the other hand, additional instrumental examination methods can exclude other brain pathology that can manifest itself as a similar neurological deficit.
The standards for diagnosing chronic cerebrovascular insufficiency include:
- neuroimaging;
- angiography;
- ultrasound scanning of head and neck vessels;
- daily monitoring of peripheral blood pressure;
- electrocardiogram;
- X-ray examination of the cervical spine;
- blood lipid spectrum analysis;
- coagulogram;
- glycemic profile.
Treatment and prevention of transient cerebrovascular accidents
A transient disorder of cerebral circulation, treatment of which begins immediately after diagnosis.
Treatment of PNMK may include: drug therapy, the prescription of antiplatelet agents and anticoagulants after studying blood tests, plasmapheresis and, of course, physical therapy.
Physiotherapy as a treatment method for PMN has been used for many years and is highly effective.
Prevention comes down to quitting smoking, controlling blood pressure levels, correcting cholesterol and lipids in the blood, correcting blood glucose levels, and regular physical activity.