Disorders of the venous circulation of the brain
Classification. The following chronic and acute variants of venous circulation in the brain are distinguished. Chronic include venous congestion and venous encephalopathy, acute include venous hemorrhage, thrombosis of the veins and venous sinuses, thrombophlebitis.
Venous stagnation. The most common form of venous circulation disorder is due to various reasons: cardiac and cardiopulmonary failure, respiratory diseases (bronchitis, bronchiectasis, bronchial asthma, emphysema, etc.); compression of extracranial veins (internal jugular, innominate, superior vena cava), struma, arterial aneurysm, tumor in the neck; neoplasms of the brain, membranes and skull, arachnoiditis, traumatic brain injury, thrombosis of the veins and sinuses of the dura mater, compression of the veins with cerebral edema and craniostenosis. With venous stagnation, metabolic changes and brain hypoxia occur, venous and intracranial pressure increases, and cerebral edema develops. More often, milder disorders occur in the form of changes in the tone of the cerebral veins, which is detected using orbital plethysmography and rheography.
Clinical manifestations. A dull headache, more pronounced in the morning, increases with movements of the head to the sides, changes in atmospheric pressure, changes in ambient temperature, after excitement, drinking alcohol, etc., there is a hum or noise in the head, cyanotic lips, cheeks, ears, nose , mucous membranes of the oral cavity, swelling of the lower eyelids, especially in the morning, dilation of the veins in the fundus. Venous pressure ranges from 55 to 80 mmH2O, arterial pressure is usually within normal limits. Stupefaction, dizziness, darkening of the eyes, fainting, and numbness of the extremities are observed. Epileptic seizures and mental disorders are possible. With severe venous stagnation, patients are unable to lower their heads and remain in a horizontal position.
Measurements of pressure in the ulnar vein, radiography of the skull (increased development of diploic veins, graduates and veins of the dura mater), and phlebography are of diagnostic value in venous pathology.
Venous encephalopathy. With venous encephalopathy, the following syndromes are distinguished: hypertensive (pseudotumorous), diffuse small-focal brain damage, bettolepsy and asthenic.
Bettolepsy, or cough epilepsy, develops with chronic bronchitis and emphysema, pneumosclerosis, bronchial asthma, especially with cardiopulmonary failure. A persistent cough may result in sudden loss of consciousness (syncope).
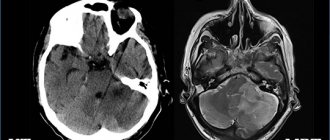
Venous hemorrhages. Capillary-venous hemorrhages in the brain and capillary-venous stasis are observed in hypertension. Venous stroke occurs in patients with heart failure, traumatic brain injury, brain tumor, infectious and toxic brain lesions. Clinical manifestations develop slowly: confusion, speech disorders, diplopia, pyramidal reflexes, hemiparesis, hemihypesthesia, damage to cranial nerves.
Thrombosis of cerebral veins. It occurs in the practice of clinicians of many specialties as a complication of various inflammatory processes, infectious diseases, operations, abortions, pregnancy, childbirth, skull trauma, “blue” heart defects, etc. Changes in the walls of the veins, a slowdown in the speed of blood flow and increased blood clotting play a role in the pathogenesis, as well as a change in the colloidal properties of endothelial cells, which contributes to the aggregation of blood cells. Often, thrombosis of the cerebral veins is combined with thrombosis of the sinuses of the brain, as well as the veins of the lower extremities.
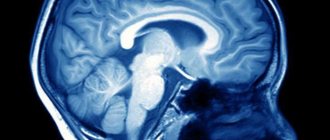
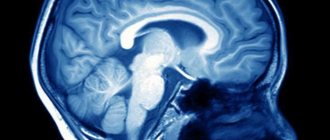
Clinical manifestations. Cerebral vein thrombosis usually develops gradually. Headache, nausea, vomiting, meningeal symptoms, congestive optic discs, increased body temperature, and increased ESR appear. In the cerebrospinal fluid, mild pleocytosis and an increase in protein content, sometimes blood, are detected. Characterized by confusion, partial motor-type seizures, and less commonly generalized convulsions. Depending on the location of the venous lesion, focal symptoms occur: aphasia, alexia, hemianopsia, flaccid or spastic paresis or paralysis, and sensory disturbances. The outcome is often favorable, focal symptoms often undergo significant or even complete regression, but there are relapses of the disease. A slow chronic course over many months and even years is possible. Sometimes there are consequences in the form of mental disorders, aphasia, convulsive seizures and paresis of the limbs.
Thrombosis of the dural sinuses. Usually develops when infection penetrates into them from a nearby focus (furuncles or carbuncles of the scalp, face, erysipelas, etc., purulent osteomyelitis of the skull bones, purulent acute and chronic otitis media, mastoiditis, purulent processes in the orbit, paranasal sinuses) along the brain and diploic veins. In addition, phlebitis and thrombosis of the dural sinuses can occur hematogenously with thrombophlebitis of the veins of the extremities or pelvis and during septic processes. Thrombosis of the cerebral sinuses is sometimes accompanied by thrombophlebitis of the retinal veins, purulent meningitis, brain abscesses, etc. Sinus thrombosis can also occur with chronic infections (tuberculosis), malignant tumors and other diseases that occur with cachexia, in debilitated patients and in old age.
Clinical manifestations. Low-grade or sometimes very high, stable or fluctuating body temperature, headache, vomiting, leukocytosis in the blood, increased intracranial pressure. With thrombosis of the sinuses of the convexital surface of the brain, general cerebral symptoms predominate; in the sinuses of the base of the brain, signs of damage to the cranial nerves predominate. Drowsiness develops, sometimes, on the contrary, motor restlessness, insomnia, delirium, epileptic seizures, rigidity of the neck muscles, Kernig's symptom, hyperesthesia to visual, auditory and skin stimuli, and sometimes trismus. Focal symptoms of brain damage correspond to the location of the sinus. Swelling and cyanosis of the face or mastoid area are noted. In the fundus, dilated veins and swelling of the optic discs are detected. The cerebrospinal fluid is clear or xanthochromic, sometimes with an admixture of red blood cells; moderate pleocytosis is noted. Septic thrombosis of the dural sinuses is manifested by chills and very high remitting temperature. With thrombosis of the superior sagittal sinus, epileptic seizures of the motor type, hemi- and paraplegia or paresis occur.
Symptoms of thrombosis of the transverse or sigmoid sinus: headache, bradycardia, sometimes double vision, septic temperature, chills, stupor, turning into a soporous and even comatose state, sometimes delirium and agitation, anti-pain position of the head with an inclination to the painful side, meningeal phenomena, leukocytosis in blood. The jugular vein may be involved in the process. In this case, swelling of the tissue surrounding the vein and signs of damage to the glossopharyngeal, vagus, accessory and hypoglossal nerves occur.
Symptoms of cavernous sinus thrombosis: exophthalmos, swelling and venous hyperemia of the eyelids, orbits, forehead, root of the nose, dilation of the fundus veins (congestion), pain and hyperesthesia in the area of innervation of the superior branch of the trigeminal nerve, chemosis of the conjunctiva, ophthalmoplegia - paralysis or paresis of muscles, innervated by the III, IV, VI cranial nerves, stupor, delirium, sometimes coma, metabolic and endocrine dysfunction.
Complications: purulent meningitis, metastatic abscesses in the lungs, septic pneumonia.
Thrombophlebitis of the cerebral veins. With thrombophlebitis of the cerebral veins, the temperature rises to subfebrile levels with periodic rises to 38–39 °C. Patients complain of headache, nausea, and vomiting. Observed stupor, stuporous state, epileptic seizures, paresis of the limbs; in the fundus – swelling and dilation of veins; in the blood - leukocytosis; in the cerebrospinal fluid - slight pleocytosis, an increase in the amount of protein and positive protein reactions, sometimes an admixture of erythrocytes.
How can you help yourself without pills?
There are two simple ways. The first can be used by each person independently without preparation. The second one is a little more difficult, but regular viewers and readers of Dr. Shishonin will master it very quickly.
It is better to use both methods: working on the points on the sides of the front of the neck, and working under the back of the head. This way, you will not only get rid of headaches and other symptoms of impaired venous outflow, but you will also feel more energetic, your mood and memory will improve. The main thing is to regularly devote time to yourself and help your body recover. The capabilities of the human body are almost limitless, but you need to develop them by doing gymnastics and self-massage.
Treatment of the syndrome
Therapy for vertebrobasilar insufficiency should be comprehensive. The therapist usually prescribes the following medications:
- Vasodilators - aimed at dilating the walls of blood vessels.
- Antiplatelet agents are necessary to minimize the risk of blood clots.
- Neuroprotectors - prevent disorders of cerebral metabolism.
- Antihypertensive - normalizes blood pressure.
- Nootropics - improve brain function.
Non-drug components of the treatment of the syndrome include:
- Manual therapy. Helps improve joint mobility, eliminates disorders in the muscle and ligament system.
- Massotherapy. Reduces pain and muscle strain.
- Physiotherapy. Reduces the load on the spine and increases its mobility.
- Acupuncture. It is prescribed as a pain reliever and strengthens the body.
- Magnetotherapy. Eliminates pain, dilates blood vessels.
Important! If the patient contacts the doctor too late, drug therapy in combination with physical procedures may not give the desired effect. In such cases, surgical intervention is required to restore blood circulation in the narrowed arteries.
Forecast
If the symptoms of venous discirculation pathology are already pronounced, the prognosis is not very favorable. There is a high probability that the disease will progress further. The risk of stroke is also increased.
However, if you follow all the doctor’s recommendations regarding the treatment of the underlying disease and symptomatic treatment of cerebral venous circulation, you can almost completely get rid of unpleasant manifestations and delay the progression of the disease until old age.
If you identify the disease at an early stage, when it is still hidden (this is why preventive annual visits to a neurologist are needed), then you can prevent even the appearance of the first symptoms.
Working out the back of the neck
As we have already found out, the problem arises due to compression of blood vessels, which is a consequence of the incorrect position of the vertebrae. Gymnastics will help solve and even more so prevent such a situation. For urgent help, you can gently influence the vessels. Let's take a closer look at how to do all this.
Gymnastics for the neck
Gymnastics should be performed regularly. Spend just 3-5 minutes a day and you will almost 100% protect yourself from headaches. A bonus is the prevention of high blood pressure – both intracranial and arterial.
There are many sets of exercises for the neck; you can see in detail, with step-by-step instructions and explanations, in Dr. Shishonin’s publications on cervical osteochondrosis. You've probably already read these articles and watched the videos, so let's briefly remind you. Tilts and rotations of the head, movements of the neck should not be performed abruptly, but carefully, so that there are pleasant sensations similar to those you experience when stretching after sleep.
Triggering a reflex response
The back of the neck can be treated with a piece of ice. The temperature effect causes a reflex reaction of the vessels: they react by restoring their shape. Dr. Shishonin spoke in detail about these techniques in specialized articles on cervical osteochondrosis.
Here we just remind you that you need to work with ice carefully. Don’t be afraid, you physically won’t be able to harm yourself, but don’t overdo it, otherwise the effect will be worse than from a delicate influence.
Three stages of pathology
Venous discirculation develops in 3 stages:
- The first is that symptoms do not appear.
- Secondly, the signs are present, but although they worsen the quality of life, they do not exclude the ability to work and the ability to self-care.
- Third, the symptoms are so strong that they provoke severe complications in the brain and throughout the body. The patient can no longer work. Over time, he cannot take care of himself; he requires constant care from other people.
The disease is insidious in that it does not manifest itself at the first stage, and when the symptoms begin to make themselves felt, the changes are sometimes irreversible. And at the second stage, you can only prevent the disease from moving into the third – the most severe phase. You can also completely alleviate the disturbing symptoms, but it is unlikely that you will be able to get rid of the pathological changes that have occurred in the brain 100 percent.
Conservative therapy
The most common treatment option is conservative therapy with anticoagulants. Drugs used for inferior vena cava syndrome include the anticoagulant warfrin or Xarelto. Detralex or phlebodia are used to improve blood flow from the legs. The main means of conservative treatment is the constant wearing of compression tights of compression class 2-3. They need to be changed every 3 months, as they lose their properties with prolonged wear.
Treating the symptoms of inferior vena cava syndrome with medications and compression can reduce chronic venous insufficiency. Considering the technical complexity of surgical treatment, conservative methods are predominant in modern medical practice.
Signs
Obvious signs of venous discirculation are varied. They are in many ways similar to other ailments and often worsen in the morning:
- Dull pain in the head.
- Feeling of lethargy and weakness, a weak body even after proper rest; difficult to get out of bed.
- Deterioration of condition before changes in atmospheric conditions.
- Tingling in different parts of the body.
- Decreased visual acuity, the appearance of spots and floaters in the visual field.
- Swelling of the eyelids.
- Blueness and swelling of the nasolabial triangle.
- When coughing, flushing of the facial skin may develop.
- Frequent fainting.
- Expansion of the network of blood vessels in the fundus.
- Loss of coordination, dizziness - this is especially common if blood stagnation is localized in the VBB (in the vertebrobasilar region).
- Epileptic seizures.
- Nausea.
- Speech or swallowing may be impaired (if the pathology affects the vertebrobasilar region).