Causes of the disease
Among the causes of compression of the brain, intracranial hematomas (epi-, subdural, intracerebral, intraventricular) come first.
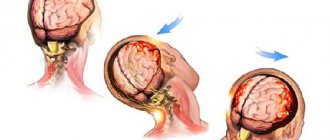
This is followed by depressed fractures of the skull bones, areas of crushing of the brain, increasing edema-swelling of the brain, acute subdural hydromas resulting from rupture of the subarachnoid cisterns, more often the base of the brain, and rapid accumulation of cerebrospinal fluid in the subdural space, pneumocephalus, the appearance of air in the cranial cavity, arising from a fracture of the base of the skull (ethmoid labyrinth). In the latter case, a valve mechanism is formed; when sneezing, coughing, or straining, air is pumped into the cranial cavity. Compression of the brain is characterized by a volumetric accumulation of liquid or coagulated blood, cerebrospinal fluid or air under the membranes. This causes local and general compression of the substance with displacement of the midline structures of the brain, deformation and compression of the ventricles, and pinching of the trunk, which leads to the development of a life-threatening condition. Intracranial hematoma (accumulation of blood) can be localized:
- Above the dura mater (epidural) 20;
- Under the dura mater (subdural) 70-80%;
- Inside the brain (intracerebral) 10%.
Symptoms and course of the disease
Compression of the brain has vague symptoms, which are similar to other organic lesions of the characteristic area. As a rule, alarming signs of the disease appear after a short period of time and affect all important organs and systems. So, the patient has a predominant disturbance of consciousness, migraine attacks are intensifying, psychomotor agitation predominates, as well as repeated vomiting. Focal symptoms are represented by unexpected epileptic seizures, and stem symptoms are represented by attacks of bradycardia, increased blood pressure, limited gaze and tonic spontaneous nystagmus.
Based on the form of the prevailing diagnosis, pathological compression of the brain rapidly progresses, and at an early stage it does not manifest itself clearly, and the symptoms are not so eloquent. As the hematoma forms, the patient's condition noticeably worsens, and the progress of the pathological process is accompanied by an epileptic attack, constriction of the pupil, repeated vomiting and a noticeable slowdown in the pulse. Meningeal symptoms, which also predominate in this clinical picture, are more clearly defined.
In any case, a characteristic anomaly entails disastrous consequences for the human body. Symptoms of compression entirely depend on the type of predominant hematoma, however, this pathogenic formation in any case has the same diagnosis and general treatment regimen. It’s just that in one case the chance of returning to a past life is quite high, but in the other, doctors have to fight for a long time for the patient’s life.
Features of the course of the pathological process are sometimes frightening with their unpredictability and reduced viability.
Treatment of the disease
Indications for mandatory hospitalization of patients with cerebral compression:
- head injury combined with progressive deterioration of neurological status;
- persistent impairment of consciousness;
- general cerebral neurological symptoms or local neurological deficit;
- convulsions;
- penetrating wound;
- open or depressed skull fracture.
It is extremely important to ensure that the patient is transported so that he does not die in the ambulance. In this clinical picture, gentle delivery of a representative patient is required, and the surface must be motionless, but not rigid.
If there is a hematoma, a ruptured bleeding vessel or depressed bone parts, a neurosurgical operation is performed - craniotomy with removal of the pathological focus. The task of a qualified neurosurgeon is to promptly eliminate the hematoma, which tends to spread and affects large areas of the brain.
After the immediate operation, the patient undergoes a long rehabilitation course, which allows him to restore his previous brain activity to a greater extent. However, it is important to understand that all surgical procedures are not always completed successfully, and in medicine there have been cases when surgical treatment ended in the death of the patient.
Subsequent treatment is carried out in the intensive care unit:
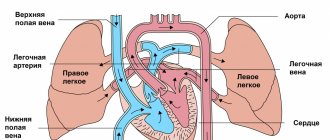
- maintaining vital functions (ventilation, monitoring heart activity);
- dehydration therapy (administration of large quantities of solutions intravenously);
- antibiotics to prevent infection;
- nootropics and neuroprotectors for the speedy restoration of brain functions;
- symptomatic therapy (anticonvulsants for seizures, sedatives for agitation).
Against the background of intensive drug therapy during the rehabilitation period, regular diagnostics are required, which includes CT and MRI. These examination methods allow you to monitor the recovery of the brain, and also promptly prevent all possible health complications. However, a patient who survives such treatment must understand that irreversible changes have occurred in his brain, so prevention must be a priority for the rest of his life.
Brain concussion
The most common injury among possible traumatic brain injuries (up to 80% of all TBIs).
Clinical picture
Depression of consciousness (to the level of stupor) during a concussion can last from several seconds to several minutes, but may be absent altogether. Retrograde, congrade and antegrade amnesia develops for a short period of time. Immediately after a traumatic brain injury, a single vomiting occurs, breathing becomes more frequent, but soon returns to normal. Blood pressure also returns to normal, except in cases where the medical history is aggravated by hypertension. Body temperature during a concussion remains normal. When the victim regains consciousness, there are complaints of dizziness, headache, general weakness, cold sweat, flushing of the face, and tinnitus. The neurological status at this stage is characterized by mild asymmetry of skin and tendon reflexes, small horizontal nystagmus in the extreme abductions of the eyes, and mild meningeal symptoms that disappear during the first week. With a concussion as a result of a traumatic brain injury, after 1.5 - 2 weeks, an improvement in the patient’s general condition is noted. It is possible that some asthenic phenomena may persist.
Diagnosis
Recognizing a concussion is not an easy task for a neurologist or traumatologist, since the main criteria for diagnosing it are the components of subjective symptoms in the absence of any objective data. It is necessary to familiarize yourself with the circumstances of the injury, using the information available to witnesses to the incident. Of great importance is an examination by an otoneurologist, with the help of which the presence of symptoms of irritation of the vestibular analyzer in the absence of signs of prolapse is determined. Due to the mild semiotics of a concussion and the possibility of a similar picture arising as a result of one of many pre-traumatic pathologies, special importance in diagnosis is given to the dynamics of clinical symptoms. The justification for the diagnosis of “concussion” is the disappearance of such symptoms 3-6 days after receiving a traumatic brain injury. With a concussion, there are no fractures of the skull bones. The composition of the cerebrospinal fluid and its pressure remain normal. CT scan of the brain does not detect intracranial spaces.
Treatment
If a victim with a traumatic brain injury has come to his senses, first of all he needs to be given a comfortable horizontal position, his head should be slightly raised. A victim with a traumatic brain injury who is in an unconscious state must be given the so-called. The “saving” position is to lay him on his right side, his face should be turned to the ground, his left arm and leg should be bent at a right angle at the elbow and knee joints (if fractures of the spine and limbs are excluded). This position promotes the free passage of air into the lungs, preventing the tongue from retracting and vomit, saliva and blood from entering the respiratory tract. Apply an aseptic bandage to bleeding wounds on the head, if any.
All victims with traumatic brain injury are necessarily transported to a hospital, where, after confirmation of the diagnosis, they are placed on bed rest for a period that depends on the clinical characteristics of the course of the disease. The absence of signs of focal brain lesions on CT and MRI of the brain, as well as the patient’s condition, which allows one to refrain from active drug treatment, allows us to resolve the issue in favor of discharging the patient for outpatient treatment.
For a concussion, overactive drug treatment is not used. Its main goals are to normalize the functional state of the brain, relieve headaches, and normalize sleep. For this purpose, analgesics and sedatives (usually in tablet forms) are used.
Brain contusion
Mild brain contusion is detected in 10-15% of victims with traumatic brain injury. A bruise of moderate severity is diagnosed in 8-10% of victims, a severe bruise - in 5-7% of victims.
Clinical picture
A mild brain contusion is characterized by loss of consciousness after injury of up to several tens of minutes. After regaining consciousness, complaints of headache, dizziness, and nausea appear. Retrograde, congrade, and anterograde amnesia are noted. Vomiting is possible, sometimes with repetitions. Vital functions are usually preserved. Moderate tachycardia or bradycardia and sometimes increased blood pressure are observed. Body temperature and respiration without significant deviations. Mild neurological symptoms regress after 2-3 weeks.
Loss of consciousness with a moderate brain contusion can last from 10-30 minutes to 5-7 hours. Retrograde, congrade and anterograde amnesia are strongly expressed. Repeated vomiting and severe headache are possible. Some vital functions are impaired. Bradycardia or tachycardia, increased blood pressure, tachypnea without respiratory distress, and increased body temperature to subfebrile are detected. The manifestation of meningeal signs, as well as stem symptoms, is possible: bilateral pyramidal signs, nystagmus, dissociation of meningeal symptoms along the body axis. Pronounced focal signs: oculomotor and pupillary disorders, paresis of the limbs, speech and sensitivity disorders. They regress after 4-5 weeks.
Severe brain contusion is accompanied by loss of consciousness from several hours to 1-2 weeks. It is often combined with fractures of the bones of the base and vault of the skull, and profuse subarachnoid hemorrhage. Disorders of vital functions are noted: respiratory rhythm disturbances, sharply increased (sometimes decreased) blood pressure, tachy- or bradyarrhythmia. Possible blockage of the airways, intense hyperthermia. Focal symptoms of hemispheric damage are often masked behind stem symptoms that come to the fore (nystagmus, gaze paresis, dysphagia, ptosis, mydriasis, decerebrate rigidity, changes in tendon reflexes, the appearance of pathological foot reflexes). Symptoms of oral automatism, paresis, focal or generalized seizures may be detected. Restoring lost functions is difficult. In most cases, gross residual motor and mental disorders remain.
Diagnosis
The method of choice for diagnosing a brain contusion is a CT scan of the brain. A CT scan reveals a limited area of low density, possible fractures of the calvarial bones and subarachnoid hemorrhage. With a brain contusion of moderate severity, CT or spiral CT in most cases reveals focal changes (non-compactly located areas of low density with small areas of increased density). In case of severe contusion, CT scan reveals areas of heterogeneous increase in density (alternating areas of increased and decreased density). Perifocal cerebral edema is severe. A hypodense track is formed in the area of the nearest section of the lateral ventricle. Through it, fluid with breakdown products of blood and brain tissue is discharged.
Diagnosis of the disease
The doctor suspects the presence of a characteristic pathology, but computed tomography allows an accurate diagnosis. The obtained studies provide an opportunity to assess the focus of pathology, as well as visually examine the features of the predominant hematoma.
- An epidural hematoma on a computed tomogram looks like a biconvex, less often plano-convex, zone of increased density adjacent to the calvarium. The hematoma is limited in nature and, as a rule, is localized within one or two lobes. With venous sources of bleeding, it can spread over a considerable distance and have a crescent shape.
- A subdural hematoma on a computed tomogram is often characterized by the presence of a crescent-shaped zone of altered density, plano-convex, biconvex or irregular in shape. Often subdural hematomas spread to the entire hemisphere or most of it. Intracerebral hematomas have the appearance of round or elongated zones of homogeneous intense increase in density with clear boundaries. Hematomas are formed both as a result of direct damage to the vessel and as a result of angioonecrosis at the site of a crush injury to the brain. Intraventricular hematomas are detected by a zone of intense homogeneous increase in density, in its topic and shape corresponding to a particular ventricle of the brain.
- Intracranial hemorrhages in victims with severe anemia may have a density similar to that of the brain. Blood clots are characterized by a higher density than liquid blood. They are more clearly differentiated from surrounding tissues. Intracranial hematomas containing fresh, uncoagulated blood may have the same density as the brain or even lower density on a computed tomogram, against the background of which, with an epidural hematoma, displacement of the dura mater may be detected.
With subsequent liquefaction of the contents of hematomas, degradation of fibrin in blood clots, and disintegration of its pigments, a gradual decrease in the density of the hematoma occurs, making it difficult to diagnose hemorrhages, especially in cases where the absorption coefficient of altered blood and the surrounding brain matter become the same. This is followed by a phase of reduced density, during which the absorption coefficient of the spilled blood approaches the density of the cerebrospinal fluid.
Diagnosis of this disease must be immediate, since the characteristic pathological condition significantly threatens the patient’s life. Thus, the primary assessment is performed according to the “ABCD” rule, and the secondary assessment includes a detailed examination of the entire body to determine the condition of the head.
Focal symptoms
General cerebral symptoms accompany focal ones, which arise and worsen. They are affected by the pathological process. This leads to drooping of the upper eyelid, diplopia, strabismus, mydriasis, central facial paresis (facial asymmetry, lagophthalmos, “sailing” cheek) on the side of the lesion.
The opposite side heterolaterally suffers from paresis, paralysis, tendon hypo- or areflexia, and hypoesthesia. Often the manifestation of epileptic seizures, hormetonic convulsions (paroxysms of muscle hypertension), tetraparesis, coordination disorders, bulbar syndrome (dysarthria, swallowing disorders, dysphonia). How to diagnose brain contusions with compression?
Prices
| Disease | Approximate price, $ |
| Prices for diagnosing migraine | 7 060 — 8 260 |
| Prices for diagnosing childhood epilepsy | 3 100 — 4 900 |
| Prices for brain shunting for hydrocephalus | 33 180 |
| Prices for treatment of Parkinson's disease | 58 600 |
| Prices for migraine treatment | 9 680 |
| Prices for the diagnosis of amyotrophic lateral sclerosis | 6 550 |
| Prices for diagnosing epilepsy | 3 520 |
| Prices for rehabilitation after a stroke | 78 300 — 82 170 |
| Prices for treatment of childhood epilepsy | 3 750 — 5 450 |
| Prices for treatment of multiple sclerosis | 4 990 — 17 300 |
| Disease | Approximate price, $ |
| Prices for pediatric neurosurgery | 30 000 |
| Prices for craniotomy | 43 490 — 44 090 |
Diagnostic methods
When compression occurs, there is a serious danger to the patient's life. Therefore, it is important to conduct diagnostic tests in a timely manner.
To determine the presence of increased pressure on organ tissue, information about the injury is first collected and a neurological examination is performed. If the patient is unconscious, the doctor interviews witnesses to the incident. To clarify the diagnosis, instrumental techniques are used:
- Magnetic resonance imaging. During the procedure, they can identify the exact area of ischemic disorders and contusion, determine the severity of the damage and check the condition of the conduction pathways.
- Computed tomography. During its course, they determine what formation caused the compression of the brain, the location of the damaged area, edematous processes and the degree of displacement of brain structures.
After studying the results of the procedures, a suitable treatment method is selected.