Structure of the spinal cord
Before talking about the components, you should understand the system itself. The spinal cord is located in the spinal canal, and is surrounded by three boundaries in the form of membranes:
- Soft
- Cobweb
- Solid
It is in constant interaction with internal organs and the brain. Its length is approximately 40 centimeters for women and 45 for men, weighing about 30 grams. It’s not for nothing that there is an expression: the spool is small, but expensive. The psychological state, the functioning of internal organs, reflexes and motor activity of a person depend on this small link.
The components of the spinal cord are gray and white matter. The location of the first of them is the central departments, the second is the periphery. In the embryo, the spinal cord occupies almost the entire spinal canal, and with subsequent growth it moves upward.
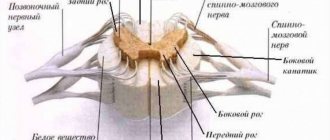
Looking at a cross-section of the human spinal cord (SC), you can see a central canal filled with brain fluid, gray matter in the shape of a butterfly (whose wings resemble horns) and white matter formed from paired cords - posterior, anterior and lateral.
Each of these sections performs a specific function that plays a vital role for a person. They ensure the passage and delivery of nerve impulses to various parts of the human body.
What is gray matter?
Because the gray matter surrounds the central canal, it is called the intermediate canal. It is presented in the form of two vertical strands of irregular geometric shape, located on both sides of the central channel, called the left and right gray pillars. These elements are connected to each other by a thin plate (adhesion), surrounding and protecting the canal on all sides, adjacent from above to the fourth ventricle of the brain, ending below with the terminal ventricle called Krause.
The basic structure of the gray matter of the SC is clearly represented in the form of horns:
- The anterior ones are the location of the largest neurons, forming five main clusters or nuclei. These clusters provide motor activity of the human body, abdominal and thoracic vibrations during breathing.
- The structure of the posterior pillars (horns) is heterogeneous. It consists of axons and neurons, which are multi-polar cells. Each of them occupies a specific place on the territory of the CM. The processes of these neurons extend to the corresponding adjacent segments of the anterior layer.
- The lateral horns are responsible for the functionality of the autonomic nervous system (ANS) and have protrusions in the areas of the eighth cervical and second lumbar vertebrae. The upper (cervicothoracic) region regulates the functioning of the heart, digestive organs, sweat glands and blood vessels. Lower (lumbosacral) – defecation, urination, erection and ejaculation.
The nerve centers of the SC are segments with neurons located in them that affect all functioning receptors and internal organs. It is quite clear how important they are for the full life of the body.
What is the composition of gray matter?
Gray matter is formed from nerve cells, of which there are more than thirteen million (including glia and processes). All neurons grouped into nuclei or plexuses that make up the gray matter of the SC are divided into three main groups:
Internal cells with numerous processes that do not extend beyond the boundaries of the substance itself and provide interaction (forming synapses) with other neurons of the SC.
Root cells (the largest motto- and multi-neurons of the ANS), the neurons of which protrude beyond the boundaries of the gray matter and innervate skeletal muscles.
Tufted neurons forming many pathways leading to the brain. These cells got their name due to their ability to form bundles, which are a kind of switches connecting SC segments.
So, the spinal cord includes neuroglia, ganglion nerve cells, pulpal and non-pulpate nerve fibers. These cells are grouped into nuclei and are located in segments along the entire length of the spinal cord and its primary three-membered reflex arc.
Each segment of gray matter is separated by barriers in the form of Rexed plates that perform specific functions:
- Reception of impulses from the dorsal roots and their transmission to the spinothalamic tract.
- Accompaniment of impulses (afferents) of temperature and pain sensitivity.
- Processing information from the muscular system.
- Receiving and transmitting brain impulses.
- Innervation of the muscles of the limbs, body and internal organs.
Disturbances in the functioning of any of the links in this system lead to serious consequences, including paralysis, partial or complete.
Symptoms
Symptoms of pathological processes develop over several years and can manifest themselves in two ways:
- Continuously evolving, with constant complication.
- During the period of progression of pathological changes, long periods of stabilization are observed without deterioration in the patient's health.
The clinical picture of the disease directly depends on the location of the pathological process in the brain and its type
Typically, symptoms worsen when your blood pressure is high for a long time.
In the initial stages, the clinical picture of leukoencephalopathy is characterized by:
- decreased mental performance;
- weakness in the limbs;
- absent-mindedness;
- slower reaction;
- apathy;
- tearfulness;
- clumsiness.
Further, sleep is disturbed, muscle tone increases, the person becomes irritable, susceptible to depression, feelings of fear, and phobias.
As a result, the patient becomes completely helpless, susceptible to epileptic seizures, unable to care for himself or control bowel and bladder emptying.
The disease develops quite quickly in most cases
First, attention is drawn to absent-mindedness, emotional lability, indifference, a tendency to depression, and the appearance of phobias. The patient loses the ability to pronounce words, concentrate and switch attention, quickly gets tired, cannot even analyze ordinary events of the day, and forgets the names of relatives. A progressive disease leads to sleep disturbances, irritability, increased muscle tone, and involuntary movements of the head and eyes
The patient's gait is disturbed
A progressive disease leads to sleep disturbances, irritability, increased muscle tone, and involuntary movements of the head and eyes. The patient's gait is disturbed.
It has been proven that leukoencephalopathy is caused by the presence of human polyomavirus. According to some data, about 80% of the world's population are carriers of the infection. But, despite this fact, cases of polyomavirus activation do not occur so often. Typically, the activation mechanism of the virus occurs under certain conditions, one and the main of which is a decline in the natural protective functions of the body, that is, immunity.
Important Multiple sclerosis: modern diagnostic methods
In addition to HIV infection and AIDS, predisposing causes for the development of this disease also include:
- leukemia and other blood pathologies;
- hypertension;
- tuberculosis;
- oncology;
- sarcoidosis;
- systemic lupus;
- rheumatoid arthritis;
- taking immunosuppressive drugs prescribed after organ transplantation;
- use of monoclonal antibodies;
- lymphogranulomatosis.
The disease has several forms:
- 1. Small focal leukoencephalopathy of vascular origin. It is a disease in which there is a chronic pathological condition of the blood vessels of the brain, which subsequently leads to damage to the cells of the white matter of the cerebral hemispheres. Predisposing factors to the development of this form of pathology is hypertension. Most often, this form is diagnosed in men whose age exceeds 55-60 years. Also at risk are people who have a genetic hereditary predisposition to the pathology. A complication of small focal leukoencephalopathy of vascular origin is the development of senile dementia.
- 2. Progressive multifocal encephalopathy. In this form of the disease, there is damage to the central nervous system by the virus, which, in turn, results in the destruction of the white matter of the brain. In most cases, progressive multifocal encephalopathy occurs against the background of human immunodeficiency. This pathology is one of the most dangerous, as its consequence can be sudden death.
- 3. Periventricular form. Develops against a background of chronic lack of oxygen and ischemia. The result of such circumstances is damage to the subcortical structures of the brain, mainly its trunk, the cerebellum and those parts that are responsible for motor activity. The periventricular form is characteristic of newborn babies and can lead to the development of cerebral palsy.
Secrets of his education
The gray matter of the SC is formed from many neurons with processes, united into nuclei and without a myelin sheath. To be more precise, it contains:
- Long neural processes
- Short neural processes
- Neuron cell bodies
- Connective and accompanying tissue
- Blood vessels
Each group of neurons is responsible for specific functions:
Sensitive ones provide the perception of impulses coming from tissues and organs. Their receptors are located throughout the human body and are concentrated on the skin and internal organs. Only their processes penetrate into the spinal cord, and the neurons themselves are located outside it.
Motor muscles are responsible for conducting impulses to the muscles from the centers of the spinal cord or brain.
Intercalary neurons have a complex structure and are located between the processes of sensory and motor neurons. Their main task is to receive and process all incoming information.
The anterior horn of the gray matter of the spinal cord is the largest and widest and houses motor neurons. The location of the sensitive nerve cells is the dorsal horn, which ensures the functioning of the internal glands and organs. The smallest and weakest middle horn is inhabited by intercalary neurons; it is here that the initial processing of all signals coming from various zones of the body takes place.
Most cells in the spinal cord are designed to control, analyze, receive and transmit pain impulses. They are multipolar, which distinguishes them from white matter neurons of the SC.
In a few words, gray matter can be characterized as a collection of nerve fibers and neurons with processes up to 0.1 millimeters in diameter and up to one and a half meters long. Each of these elements has its own purpose and different functionality.
Spinal cord
The spinal cord (medulla spinalis) is a complex of gray matter nuclei and white nerve fibers, forming 31 pairs of segments. The spinal cord has a length of 43-45 cm, a mass of about 30-32 g. Each segment includes a part of the spinal cord, a corresponding sensory (sensitive) root entering from the dorsal side, and a motor (motor) root emerging from the ventral side of each segment.
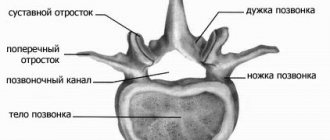
The spinal cord is located in the spinal canal, surrounded by membranes between which cerebrospinal fluid circulates. In length, the spinal cord occupies the space between the first cervical and the upper edge of the second lumbar vertebra. In the lower part it has a medullary cone (conus medullaris), from which the filum terminate begins, at the level of the II coccygeal vertebra, attached to the dura mater. The filament is part of the caudal section of the embryonic neural tube. When the spine flexes and extends, a slight displacement of the spinal cord occurs in the spinal canal. When a person is in an upright position during relative rest, the brain takes on the most stable position due to the elasticity of the spinal roots and mainly the dentate ligaments (ligg. dentata). Two pairs of dentate ligaments of each segment - derivatives of the pia mater - begin from the lateral surface of the spinal cord, between the anterior and posterior roots of the spinal nerves and are attached to the dura mater.
The diameter of the spinal cord along its length is uneven. At the level of the IV-VIII cervical and I thoracic segments, as well as in the lumbar and sacral regions, there are thickenings (intumescentiae cervicalis et lumbalis), which are caused by a quantitative increase in the nerve cells of the gray matter involved in the innervation of the upper and lower extremities.
The spinal cord consists of almost two symmetrical halves, separated in front by a deep median fissure (fissura mediana), and behind by a median groove (sulcus medianus) (Fig. 458). On the right and left halves there are anterior and posterior lateral grooves (sulci laterales anterior et posterior), in which the motor and sensory nerve roots are located, respectively. The spinal cord grooves delimit three cords of white matter located on the surface of the gray matter. They are formed by nerve fibers, which are grouped according to their functional properties, forming the so-called pathways (Fig. 459). The anterior cord (funiculus anterior) is located between the anterior fissure and the anterior lateral groove; the lateral cord (funiculus lateralis) is limited by the anterior and posterior lateral grooves; the posterior cord (funiculus posterior) is located between the posterior sulcus and the lateral posterior sulcus.
458. External shape of the spinal cord. A - spinal cord with spinal roots and sympathetic trunk (red); B - spinal cord from the ventral side; B - spinal cord from the dorsal side. 1 - fossa rhomboidea; 2 - intumescentia ccrvicalis; 3 - sulcus medianus posterior; 4 - sulcus lateralis posterior; 5 - fissura mediana anterior; 6 - sulcus lateralis anterior; 7 - intumescentia lumbalis; 8 - filum terminate
In the cervical region and upper thoracic region, between the posterior median and posterior lateral grooves, there is a barely noticeable posterior intermediate groove (sulcus intermedius posterior), dividing the posterior cord into two bundles.
459. Transverse section of the spinal cord. 1 - posterior median groove and septum; 2 - thin beam (Gaull); 3 - wedge-shaped bundle (Burdakha); 4 - posterior sensitive root; 5 - marginal zone; 6 - spongy layer; 7 - gelatinous substance; 8 - rear pillar; 9 - spinocerebellar posterior tract (Flexig); 10 - lateral cortical tract; 11 - reticular formation; 12 - own bundle of the spinal cord; 13 - red nuclear spinal tract; 14 - anterior spinocerebellar tract (Gowers); 15 - spinothalamic tract; 16 - vestibulospinal tract; 17 - anterior corticospinal tract; 18 - anterior median fissure; 19 - anterior median nucleus of the anterior column; 20 - anterior motor root; 21 - anterior lateral core of the anterior column; 22 - intermediate-medial nucleus; 23 - intermediate-lateral nucleus of the lateral column; 24 - posterior lateral core of the anterior column; 25 - dorsal nucleus; 26 - own nucleus of the posterior horn
The gray matter of the spinal cord (substantia grisea medullae spinalis) occupies a central position in the spinal cord, appearing in a transverse section in the form of the letter “H”. It consists of multipolar nerve cells, myelinated, unmyelinated fibers and neuroglia.
Nerve cells form nuclei, which along the spinal cord merge into the anterior, lateral and posterior columns of gray matter (columnae anterior, lateralis et posterior). These columns* are connected in the middle by the anterior and posterior gray commissures (commisurae griseae anterior et posterior), separated by the central spinal canal, which is a reduced canal of the embryonic neural tube.
*(The anterior, lateral and posterior horns do not exist in the spinal cord, since the gray matter is represented by the anterior, lateral and posterior columns.
)
Gray matter nuclei
. In the posterior columns (Fig. 459) there is a superficially located marginal zone (zona terminalis), consisting of small nerve cells; somewhat deeper is the spongy substance (substantia spongiosa), formed by tufted cells, the axons of which pass through the white matter and unite into pathways. These pathways carry nerve impulses from the nuclei of the spinal cord to its other segments or the brain. The spongy substance is covered with a gelatinous substance (substantia gelatinosa), consisting of small nerve and glial cells; then the own nuclei of the posterior column (nucll. proprii), formed by multipolar and tufted cells, are located. The axons of the tuft cells form the anterior white commissure (commissura alba), moving to the opposite half of the spinal cord, where they take part in the formation of the anterior spinocerebellar tract (tr. spinocerebellaris anterior) and the spinothalamic tract (tr. spinothalamics).
At the base of the posterior column there is a dorsal nucleus (nucl. dorsalis), formed by tufted cells, the axons of which extend into the white matter of the lateral cord and form the posterior spinocerebellar tract (tr. spinocerebellaris posterior). In the intermediate zone, at the level of the gray commissure, there is a central intermediate substance (substantia intermedia centralis) and lateral to it, in the area of the lateral columns - a lateral intermediate substance (substantia intermedia lateralis), which in the thoracic region is the center of sympathetic innervation; in the sacral region between the II-IV segments there is an intermediate substance - the center of parasympathetic innervation.
In addition to the dorsal column nuclei described above, there are small multipolar cells, the axons of which form associative and commissural bundles of the spinal cord. Association bundles are connected to the cells of their half of the spinal cord, commissural bundles are connected to the opposite side.
Between the anterior and posterior columns, the gray matter penetrates the white matter in strands, forming a network-like loosening, called the reticular formation (formatio reticularis).
In the anterior columns of the gray matter of the spinal cord there are the anterior medial and lateral, posterior medial and lateral nuclei and the intermediate nucleus, consisting of motor neurons.
There are large alpha (A) and small alpha (α) neurons, as well as smaller gamma (γ) neurons. The axons of large alpha neurons innervate muscles with a predominant content of white striated fibers, which are involved in performing fast movements. The axons of small alpha neurons innervate red striated muscle fibers, which contract slowly but with greater force. Gamma neurons contract muscle spindles, which in turn causes afferent impulses from the myotube, exciting alpha motor neurons. Both medial nuclei are well developed throughout the entire anterior column of the spinal cord and innervate the muscles of the trunk, while the muscles of the limbs are innervated from the lateral and intermediate nuclei.
Thus, the gray matter of the spinal cord represents nerve cells grouped into nuclei, united into nine plates (laminae):
The I plate is a flat thin layer of a mesh structure consisting of large nerve cells, which corresponds to the zona terminalis.
Lamina II consists of densely lying small neurons. This plate contains the substantia spongiosa.
The III lamina is similar in structure to the previous one, only the nerve cells are somewhat larger in size and form the substantia gelatinosa.
Lamina IV is formed by large multipolar and tufted cells. It contains nucl. proprius, where the neurons innervating the skin and muscle tendons switch.
Laminae V and VI also contain tuft cells that form nucl. dorsalis. These cells switch proprioceptive pathways.
The VII lamina represents the more ventral part of the interstitial gray matter between the two columns and the central part of the anterior column, corresponding to the substantia intermedia centralis.
The VIII plate is located on the medial part of the anterior column. Cell processes form associative and commissural fibers (commissura alba) of the anterior column.
The IX plate includes a group of large motor neurons of the anterior horn, where several motor nuclei are located.
The white matter of the spinal cord (substantia alba medullaris spinalis) is formed by myelinated nerve fibers (axons). Proper bundles of white matter surround the gray matter of the spinal cord. Projection pathways pass in the anterior, lateral and posterior cords of the white matter (Fig. 460).
Anterior cord
. Formed by four tracts and a white anterior commissure.
1. The anterior corticospinal tract (tr. corticospinalis anterior) mainly begins from the pyramidal cells of the anterior central gyrus of the cerebral cortex. It descends down the brain stem without crossing, reaching the spinal cord, where in each segment it passes to the opposite side.
2. The anterior spinothalamic tract (tr. spinothalamics anterior) is located lateral to the previous tract and in front of the anterior column of gray matter. Formed by crossed fibers of tuft cells of the posterior column of the spinal cord. Ends in the thalamus.
3. The vestibulospinal tract (tr. vestibulospinalis) is located superficially in the anterior part of the anterior cord. It is formed by fibers originating from the nuclei of the balance nerve of the medulla oblongata and ends in the nuclei of the anterior column of the spinal cord.
4. The tectospinal tract (tr. tectospinal) is located behind the lateral anterior groove. Its fibers start from the cells of the quadrigeminal nuclei and connect to the motor cells of each segment of the spinal cord.
Lateral cord
. The lateral cord of the white matter is a more massive formation in which most of the conductors are located (Fig. 459, 460).
460. Diagram of the location of pathways in the spinal cord (A, B). 1 - fasc. gracilis (Gaull's path); 2 - fasc. cuneatus (Burdach's path); 3 - beam for general sensitivity; 4 - tr. spinocerebellaris posterior; 5 - tr. corticospinalis lateralis; 6 - tr. rubrospinalis; 7 - own pathways of the spinal cord; 8 - tr. spinothalamic lateralis; 9 - tr. spinotectal; 10 - tr. spinocerebellaris anterior; 11 - posterior root; 12 - anterior root; 13 - tr. corticospinalis anterior; 14 - tr. vestibulospinal; 15 - tr. spinothalamics anterior; 16 - anterior connecting branch; 17 - sympathetic node; 18 — gray connecting branch; 19 - spinal nerve (ventral branch); 20 - spinal nerve (dorsal branch)
1. The lateral tract of the spinal cord (tr. dorsolaterals) is located on the lateral surface of the anterior, lateral and posterior columns.
2. The lateral pyramidal, or corticospinal, tract (tr. corticospinalis lateralis) consists of efferent fibers extending from the cells of the cerebral cortex. They occupy the area of the lateral cord between the posterior and lateral columns of the gray matter of the spinal cord. Its fibers in each segment on its side form synapses with the motor cells of the anterior column. Towards the spinal conus, the thickness of the lateral corticospinal fasciculus decreases.
3. The posterior spinocerebellar tract (tr. spinocerebellaris posterior) is located on the surface of the lateral cord of the spinal cord, covering tr. corticospinalis lateralis. It is formed by nerve fibers of tuft cells nucl. dorsalis of the posterior column on its own side and goes to the cerebellum.
4. The red nucleus-spinal tract (tr. rubrospinal) is a group of descending fibers that begin from the cells of the red nucleus. In the lateral funiculus they pass in front of tr. corticospinalis lateralis.
5. The lateral spinothalamic tract (tr. spinothalamicus lateralis) is the fibers of the ascending tract, which begin in the posterior column of the spinal cord, cross in the spinal cord, and are located anterior and lateral to tr. rubrospinal and end in the optic thalamus.
6. The anterior spinocerebellar tract (tr. spinocerebellaris anterior) is located on the surface of the lateral cord, behind the anterior lateral groove of the spinal cord, covering tr. spinothalamicus lateralis. It begins in the posterior columns of the spinal cord and goes to the cerebellum.
7. The spinal-tegmental tract (tr. spinotectal) and the tectal-spinal tract (tr. tectospinalis) are located directly behind the lateral anterior sulcus of the spinal cord. These fibers are direct and feedback connections between the nuclei of the posterior and anterior columns of the spinal cord, the superior and inferior colliculus.
Posterior cord
. The posterior cord consists of three bundles of fibers.
1. A thin fascicle (fasc. gracilis) is located between the median and intermediate grooves. It is formed from the central processes of nerve cells of the spinal nodes, from the IX thoracic and underlying nodes.
2. The wedge-shaped bundle (fasc. cuneatus) is located lateral to the previous one and is limited by the lateral posterior and intermediate grooves. It also consists of processes of cells of the thoracic and cervical spinal nodes. The fibers of these bundles end in the nuclei of the medulla oblongata.
3. The bundle for the tactile sense is located between the previous bundles. It starts from the nuclei of the posterior columns of the spinal cord and ends in the thalamus.
Central canal of the spinal cord
. The central canal represents a reduced remnant of the embryonic neural tube, which communicates at the top with the IV ventricle and ends with an expansion in the conus medullaris. Contains cerebrospinal fluid. It runs in the center of the spinal cord and has a diameter of 0.5×1 mm. In old age it may become partially obliterated.
Spinal cord segments
. The spinal cord combines 31 pairs of segments: 8 cervical (CI-VIII), 12 thoracic (ThI-XII), 5 lumbar (LI-V), 5 sacral (SI-V) and 1 coccygeal (COI). Each segment consists of a group of spinal ganglion cells that form the anterior and posterior columns, which connect with the fibers of the anterior and posterior roots of the spinal cord. The dorsal roots are formed by processes of sensory cells of the spinal ganglia, the anterior roots - by processes of motor cells of the nuclei of the anterior columns.
Embryonic development of the spinal cord
. Until the fifth month of intrauterine development, the spinal cord completely fills the spinal canal and the roots of the spinal segments correspond in topography to the level of the spinal segments. From the fifth month of the embryonic period, the spinal cord begins to lag behind in growth from the spine, but the connection of the spinal cord segments with the corresponding spinal nerves is preserved. In a newborn, the spinal cone is located at the level of the third lumbar vertebra, and at 18 years of age - at the level of the upper edge of the second lumbar vertebra. The discrepancy in the level and location of the spinal and vertebral segments is present in all parts of the spinal cord, but it is especially pronounced in its lower part (Fig. 461). Thus, in the cervical and thoracic regions, the spinal segments are located one vertebra higher. For example, the VII thoracic vertebra lies at the level of the VI thoracic arch. All lumbar segments are concentrated at the level of the XI thoracic vertebra, and all sacral and coccygeal segments correspond to the XII thoracic and I lumbar vertebrae.
461. Diagram of the relationship of nerve segments to vertebrae. I - cervical segments; II - thoracic segments; III - lumbar segments; IV - sacral segments; V - coccygeal segments. Arabic numerals indicate the corresponding vertebrae and spinal nerves
Age characteristics. In a newborn, the length of the spinal cord is 14 cm, weight is about 3 g, the lower end corresponds to the upper edge of the third lumbar vertebra. After birth, the thoracic region grows fastest, then the cervical region, and the slowest is the lumbar and sacral region. The lateral grooves are not clearly defined. The central canal is proportionally wider in diameter than in an adult. Significant differences are observed in the internal structure of the spinal cord. In children under 4-7 years of age, the process of myelination of the nerve fibers of the white matter cords occurs, except for the anterior pyramidal fasciculus, the fibers of which are already covered with a myelin sheath at the time of birth. Until the age of 8, the inclusion of pigment and the development of glial elements are noted in the cells of the gray matter.
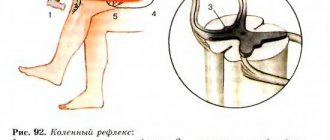
Function. The spinal cord participates in local unconditioned and conditioned reflex reactions to the received irritation; the primary arcs of afferent and efferent impulses are closed in it. The spinal cord contains fibers involved in the formation of cortical unconditioned and conditioned reflexes.
Damage to the nuclei of the columns of gray matter or the fibers of the white matter of the spinal cord disrupts these processes, causing paralysis of the muscular system and loss of various types of sensitivity.
Functions and Features
Gray matter is located in the center of the spinal cord along almost the entire spinal column. At the levels of the lumbar and cervical regions it has a pronounced thickening, the presence of gray brain tissue is somewhat increased here. Thanks to this structure, human mobility and the ability to perform certain manipulations are ensured.
In addition, the SM performs a number of other important functions:
- Protective. The gray matter, like a membrane, is located around the central canal, protecting and circulating the cerebrospinal fluid (CSF), which delivers nutrients to tissues and nerve fibers.
- Regulatory. Most of the neurons and cells of the gray matter of the SC are capable of controlling many vital processes. They regulate the proper functioning of certain organs: kidneys, intestines, bladder, secretory glands and reproductive system.
- Conductor, which consists in ensuring information exchange between the brain and all systems, muscles, blood vessels and internal organs.
- Reflex. Many impulses received by the spinal cord are processed independently by it. At the same time, the load on the brain is reduced, responses occur without its participation and are called unconditioned reflexes. They play an important role, as they are sometimes created in an instant reaction (for example, to impulses of a warning and painful nature).
It turns out that the set of responsibilities assigned to the spinal cord is very large. This explains its complex structure and intricate structure.
Treatment and diagnosis
The main way to find multiple lesions is to visualize the medulla on magnetic resonance imaging. On layer by layer
Spots and pinpoint changes in tissue are observed in the images. MRI shows not only lesions. This method also reveals the cause of the lesion:
- A single lesion in the right frontal lobe. The change indicates chronic hypertension or a previous hypertensive crisis.
- Diffuse foci throughout the cortex appear when the blood supply is disrupted due to atherosclerosis of the cerebral vessels or.
- Foci of demyelination of the parietal lobes. It speaks of a disruption in the flow of blood through the vertebral arteries.
- Massive focal changes in the white matter of the cerebral hemispheres. This picture appears due to atrophy of the cortex, which forms in old age, from Alzheimer's disease or Pick's disease.
- Hyperintense lesions in the white matter of the brain appear due to acute disruption of the blood supply.
- Small foci of gliosis are observed in epilepsy.
- In the white matter of the frontal lobes, single subcortical foci are predominantly formed after a heart attack and softening of the brain tissue.
- A single focus of gliosis in the right frontal lobe most often appears as a sign of brain aging in older people.
Magnetic resonance imaging is also performed on the spinal cord, in particular on the cervical and thoracic regions.
Related research methods:
Visual and auditory evoked potentials. The ability of the occipital and temporal regions to generate electrical signals is tested.
Lumbar puncture. Changes in the cerebrospinal fluid are examined. Deviation from the norm indicates organic changes or inflammatory processes in the cerebrospinal fluid ducts.
A consultation with a neurologist and psychiatrist is indicated. The first studies the functioning of tendon reflexes, coordination, eye movements, muscle strength and synchrony of extensor and flexor muscles. The psychiatrist examines the patient’s mental sphere: perception, cognitive abilities.
Foci in the white matter are treated with several branches: etiotropic, pathogenetic and symptomatic therapy.
Etiotropic therapy is aimed at eliminating the cause of the disease. For example, if vasogenic lesions of the white matter of the brain are caused by arterial hypertension, the patient is prescribed antihypertensive therapy: a set of drugs aimed at lowering blood pressure. For example, diuretics, calcium channel blockers, beta blockers.
Pathogenetic therapy is aimed at restoring normal processes in the brain and eliminating pathological phenomena. Drugs are prescribed that improve blood supply to the brain, improve the rheological properties of blood, and reduce the need for oxygen in brain tissue. Vitamins are used. To restore the functioning of the nervous system, it is necessary to take B vitamins.
Important Lecture No. 16. ontogeny of multicellular animals that reproduce sexually
Symptomatic treatment eliminates symptoms. For example, for seizures, antiepileptic drugs are prescribed to eliminate foci of excitation. In case of low mood and lack of motivation, the patient is given antidepressants. If lesions in the white matter are accompanied by an anxiety disorder, the patient is prescribed anxiolytics and sedatives. If cognitive abilities deteriorate, a course of nootropic drugs is indicated - substances that improve the metabolism of neurons.
Didn't find a suitable answer? Find a doctor and ask him a question!