general information
The anatomy of the spinal cord differs from the brain in its oblong structure. In Latin the organ is called medulla spinalis. It is a thickened tube with a small channel inside, slightly flattened in front and behind. It is this structure that ensures the normal transportation of nerve impulses from the main organ located in the cranium to the peripheral structures of the nervous system.
Locally, the organ is located in the spinal canal, where soft and bone tissues and nerve endings responsible for many functions of the human body are concentrated. Without a normally functioning spinal cord, natural breathing, digestion, heartbeat, reproductive activity, and any motor activity are not possible.
In humans, it begins to form at about 4 weeks of development inside the mother’s womb. But in what form it is observed in an adult, it appears much later; at first it is a neural tube, gradually developing into a full-fledged organ. It completes its formation within 2 years after birth.
Spinal cord: characteristics of conduction and reflex functions. Brown-Stokes syndrome.
The spinal cord consists of 31-33 segments: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and 1-3 coccygeal.
A segment is a section of the spinal cord associated with one pair of anterior and a pair of dorsal roots.
Rear
(dorsal) roots of the s/m - the central processes of afferent sensory neurons.
Bodies - in the s/m and h/m nerve nodes (ganglia). Anterior
- axons of efferent neurons.
Bell-Magendie law , anterior roots are efferent, posterior roots are afferent.
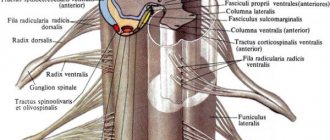
On a transverse section of the s/m: gray matter
- a collection of nerve cells.
It is bordered by white matter
- nerve fibers.
The nerve fibers of the white matter form the dorsal (posterior), lateral and ventral (anterior) cords of the spinal cord
, which include the conductive tracts of the spinal cord. In the posterior cords there are ascending cords, in the anterior cords there are descending ones, and in the lateral cords there are both ascending and descending pathways.
In the gray matter, dorsal (posterior) and ventral (anterior) horns
. In addition, there are lateral horns in the thoracic, lumbar and sacral segments.
All gray matter neurons can be divided into three main groups:
1) interneurons - in the dorsal horns of the spinal cord,
2) efferent motor neurons - in the anterior horns,
3) efferent preganglionic neurons of the autonomic nervous system, in the lateral and anterior horns of the s/m.
A segment of the spinal cord, together with the innervated areas of the body, is called a metamer . A group of muscles innervated by one segment of the spinal cord is called a myotome . The area of skin from which sensory signals travel to a specific segment of the spinal cord is called a dermatome .
There are three main functions of the spinal cord:
1) reflex,
2) trophic,
3) conductor.
Reflex function of the s/m: segmental
and
intersegmental
.
1) Segmental s/m consists in the direct regulatory influence of efferent neurons of the spinal cord on the effectors innervated by it when irritating the receptors of a certain dermatome.
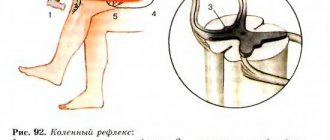
Reflexes whose arc switches in the spinal cord are called spinal . The simplest spinal reflexes include tendon reflexes .
Depending on the location of the receptors and the nerve center in humans, there are:
The ulnar flexion reflex occurs when the tendon of the biceps brachii muscle is struck (in the area of the cubital fossa) and is manifested in flexion of the arm at the elbow joint. The nerve center of this reflex is localized in the 5-6 cervical segments of the spinal cord.
The ulnar extensor reflex occurs when the tendon of the triceps brachii muscle is struck (in the area of the ulnar fossa) and is manifested in the extension of the arm at the elbow joint. The nerve center of this reflex is localized in the 7-8 cervical segments of the spinal cord.
The knee reflex occurs when the quadriceps tendon is struck below the kneecap and is manifested in the extension of the leg at the knee joint. The nerve center of this reflex is localized in the 2-4 lumbar segments of the spinal cord.
The Achilles reflex occurs when the heel tendon is struck and is manifested in flexion of the foot at the ankle joint. The nerve center of this reflex is localized in 1-2 sacral segments of the spinal cord.
types of fibers in skeletal muscle : extrafusal
and
intrafusal
, which are connected in parallel.
Intrafusal m.v. perform a sensory function. They consist of a connective tissue capsule
in which proprioceptors are located, and
peripheral contractile elements
.
Diagram of the reflex arc of the spinal tendon reflex
1) intrafusal muscle fiber, 2) proprioceptor, 3) afferent sensory neuron, 4) spinal cord motor neuron, 5) extrafusal muscle fibers.
The total time of the spinal tendon reflex is short, because its reflex arc is monosynaptic. It includes rapidly adapting receptors, phasic a-motoneurons, and FF and FR type motor units.
2) Intersegmental function of the s/m - implementation of intersegmental integration of spinal reflexes, which is provided by intraspinal pathways connecting different segments of the spinal cord.
The trophic function of the s/m is the regulation of metabolism and the provision of nutrition to those organs and tissues that are innervated by the neurons of the spinal cord. It is associated with the non-pulse activity of neurons capable of synthesizing many trophotropic biologically active substances. These substances slowly move into the nerve endings, from where they are released into the surrounding tissue.
The conductive function of the s/m is to ensure bilateral connections between the spinal cord and brain. It is provided by its ascending and descending pathways - groups of nerve fibers.
Ascending pathways:
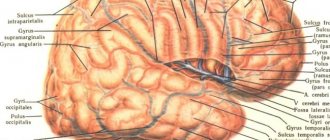
1) Gaulle and Burdach, conductors of skin-mechanical sensitivity from tactile receptors and proprioceptors to the sensory zones of the posterior central gyrus of the GBP. Gaulle's path provides information from the lower part of the body, and Burdach's - from the upper part.
2) spinothalamic, conductor of tactile, temperature and pain sensitivity. This pathway ensures the transmission of information about the quality of the stimulus to the posterior central gyrus.
3) spinocerebellar - from tactile receptors, as well as proprioceptors of muscles, tendons and joints to the cerebellar cortex.
Structure
The local location of the spinal cord along the entire back has its own characteristics. This physiology ensures that the organ performs its basic functions. The organ begins at the level of the 1st cervical vertebra, where it is gently rebuilt into the brain, but there is no clear division in them. At the junction there is a crossover of the pyramidal tracts responsible for the motor activity of the limbs. The spinal cord ends in the region of the 2nd lumbar vertebra, so it is shorter in length than the entire spine as a whole. This feature allows lumbar puncture to be performed at the level of the 3-4 lumbar vertebrae, without the risk of damaging the spinal cord.
What is special about the structure? The oblong tube has two grooves at the front and back. The brain is covered by three membranes:
- Solid. It is the tissue of the periosteum of the spinal canal, followed by the epidural space and the outer layer of the dura mater.
- Cobweb. A thin, colorless plate that fuses with the hard shell in the area of the intervertebral foramen. In the place where there is no fusion, the subdural space is located.
- Vascular. A soft membrane separated from the previous one by a subarachnoid space with cerebrospinal fluid. The membrane is adjacent to the spinal cord and consists mainly of choroid plexuses.
The space between them is filled with cerebrospinal fluid - cerebrospinal fluid. The gray matter is located in the center of the organ. It consists of intercalary and motor neurons. It also contains two types of horns: the anterior ones, which contain motor neurons, and the posterior ones, where interneurons are located.
No ads 1
External characteristics
The external structure of the spinal cord largely follows the contours of the spine, since the structures adapt to its physiological curves. Two thickenings are observed in the area of the neck and lower thoracic, the beginning of the lumbar calving. These places are characterized as exits of the roots of the spinal nerves responsible for the innervation of the arms and legs.
The external structure can be briefly described by the following characteristics:
- The shape is cylindrical, flattened on the front and back sides.
- Visually, the spinal cord looks like an elongated “cord” with processes.
- On average, the length of the organ is 42-44 cm, but directly depends on the person’s height.
- The mass is 34-38 g, which is 50 times less than the organ of the brain.
- There are two grooves in front and behind, which visually divide the organ into two symmetrical parts.
- In the middle there is a canal, which in the upper part communicates with one of the ventricles of the brain. Inferiorly, the central canal expands, forming the terminal ventricle.
The thickness of the spinal cord is uneven and depends on in which part the measurement is taken. The organ also has four surfaces: two rounded lateral, a convex posterior and a flattened anterior. The external structure is in many ways reminiscent of the internal part of the ridge, since the organ fills the entire canal. The organ is reliably protected by bone tissue.
[node:field_similarlink]
Internal structure
The spinal cord is made up of nerve tissue cells called neurons. They are concentrated closer to the center and form gray matter. According to rough estimates by scientists, the entire organ contains about 13 million cells, which is many times less than in the head section. The gray matter is located inside the white matter, and if you make a cross section, it will be shaped like a butterfly. This is especially clearly visible in the diagram.
Schematic cross-section of the spinal cord
This unique anatomy allows the spinal cord to be divided into several structures. It is arranged as follows:
- Front horns. They are distinguished by their rounded, wide shape and consist of neurons responsible for transmitting nerve impulses to the muscles. It is precisely because they perform such a task that they are called motor. The anterior roots of the spinal nerves begin in the anterior horns.
- Hind horns. They are distinguished by a long, narrow shape and consist of interneurons. They bear this name due to their ability to receive incoming signals from the sensory roots of the spinal nerves, otherwise they are called dorsal roots.
- Side horns. They are present only in the lower segments of the organ, and contain vegetative nuclei responsible for the dilation of the pupils, or the functioning of the sweat glands.
The physiological function of nerve endings is to transmit signals from the brain to the spinal cord, as well as deliver received impulses in the opposite direction. This ensures interconnection at all levels and areas of the nervous system. Nerve fibers are combined into bundles and are present along the entire length of the spinal cord.
Metamer and segmental structure
Each part of the spinal cord is a constituent element of a specific metamere of the body. Moreover, if there is a “piece” of the spinal cord that includes a section of gray matter with a pair of roots, then the metamer includes the spinal segment itself, muscle fiber (myotome), a section of the epidermis (dermatome), a bone component (scletorome), an internal organ (splanchiotome), controlled by this segment. In humans and higher representatives of the animal world, radicular metamerism is observed - the spinal cord is confined to certain parts of the body.
The skin areas of the body consisting of sensory fibers that approach the corresponding segment of the spinal cord are called dermatomes. They are strips of epidermis controlled by sensitive nerve endings. They are located throughout the body and sometimes overlap each other.
Visual representation of the connection between the skin and the spinal cord
Myotomes are muscle groups that receive motor fibers from certain areas of the brain. Thanks to the study and knowledge of their location, the process of damage and diagnosis of spinal cord lesions is greatly simplified. Damage to a certain segment of the spinal cord provokes sensory and motor disorders.
Connection between the spinal cord and muscle fiber
Segmental structure
The spinal cord is conventionally divided into five sections, although it is a single whole. The name of each directly depends on its location in the body. In total, a person may have 31-33 segments, which consist of:
- Cervical area - includes 8 segments.
- Thoracic region - 12 segments.
- Lumbar region – 5 segments.
- Sacral – 5 segments.
- Coccygeal – 1-3 segments.
This division allows us to examine the organ in more detail and simplify the process of diagnosing various pathologies.
No ads 2
White and gray matter
In cross-section, the symmetrical halves can be seen in detail and the anterior medial fissure and connective tissue septum can be seen. The part located inside is darker and is called gray matter (GM), it is located in a lighter substance - white matter (WM). Most of the SV is located in the lumbar region, the least is observed in the thoracic region. What are the main functions of gray matter:
- Transmission of pain impulses.
- Response to temperature changes.
- Closure of reflex arcs.
- Obtaining information from muscle tissue, tendons, ligaments.
- Formation of pathways.
What is the structure of white matter? It consists of myelinated, unmyelinated nerve fibers, blood vessels and a small amount of connective tissue. Its main task is to trigger simple reflexes and provide connections with skeletal muscles.
Spinal cord injury and its consequences
Treatment of spinal injury and spinal cord damage is a rather lengthy and serious process that does not always lead to a complete recovery of the patient. Some disorders appear immediately, and some can develop over time, appearing as symptoms of osteochondrosis, intervertebral hernias, and trigger the development of various arthrosis, stenosis, myelopathy and other diseases.
Anatomical structure of the spinal cord
The spinal cord, like the brain, despite its soft structure, is one of the most protected organs of the human body. It is covered with several membranes (soft layer, arachnoid and hard), the spaces are filled with cerebrospinal fluid. Thus, the brain is suspended in a liquid medium by thin cables, which allows it to withstand physical stress, shock from running and walking, stretching, and even shock.
The spinal cord is located in the spinal canal (a through hole in the spine) and is protected on all sides by bone structures, a strong muscular and ligamentous corset. The outer dense membrane of the brain does not touch the walls of the canal. Between them there is a gap called the epidural space, which is filled with fatty tissue, blood vessels, nerve roots and cerebrospinal fluid.
It is quite difficult to damage such a structure, even almost impossible in a calm and measured life. Therefore, even severe spinal injury usually occurs without damage to the spinal cord, although it provokes the development of chronic degenerative-dystrophic processes.
The consequences of damage to the spinal cord by fragments of spinal bone tissue can be very different and depend on the location of the damage (from temporary impairment of the motor abilities of the limbs to complete immobility or death). Sometimes there are cases when the initial problems can be quickly localized, and then the process of gradual death of brain cells, inflammation begins, oxygen starvation of the pathological area begins and further damage to healthy cells.
Causes and consequences of spinal cord injury
In everyday life, getting an injury that leads to a spinal fracture and spinal cord damage is quite difficult. But some extreme situations can provoke enormous stress, under which the body’s compensatory abilities are not effective enough.
Road traffic accidents. Car accidents are the most common cause of such severe injuries. In this case, not only the drivers themselves are at risk, but also pedestrians who find themselves at the scene of an accident at the wrong time.
Extreme sports. Some people deliberately put their lives in danger. These include skiers, rock climbers, mountain cyclists, roller skaters, skateboarders, divers, race car drivers, motorcycle drivers, etc.
Falls from heights. In this case, it does not matter at all from what distance and under what conditions the fall occurred - the risk of injury and damage is the same. Falling from scaffolding during construction work or childish jumping into water from a bridge or bungee jump can lead to the same consequences.
Domestic injuries and criminal cases. This section includes injuries sustained from an unsuccessful fall on ice in winter, from a stepladder or ordinary ladder, on a slippery floor (such injuries are more typical for older and elderly people, when coordination of movements is already impaired), as well as criminal stories when the integrity of the spine and spinal cord are damaged by knife or bullet wounds.
Injuries to the spinal column and spinal cord received in all of the above situations can have the most serious consequences. Of course, slight damage to the lining of the brain and leakage of cerebrospinal fluid may cause some temporary disturbances in motor abilities or nerve sensations, but nothing particularly terrible will result.
It is much more unpleasant when pathologies of muscle structures and internal organs do not disappear or kyphosis, scoliosis, vertebral instability, spondylolisthesis or retrolisthesis begin to develop, the treatment of which often requires surgical intervention. The occurrence and treatment of spinal neuromas are in most cases associated with injuries to the vertebrae and spinal cord. In some cases, the process of programmed death of spinal cord cells (apoptosis) may begin, in which clinical signs of damage appear progressively.
Complete rupture of the spine and spinal cord at the level of the cervical segment leads to instant death. Rupture of the lower sections gives a person a chance to live, since the lungs and heart are able to work independently of the spine, but the motor ability of the body will be blocked for some time by spinal shock.
Treatment of spinal cord injuries
The spinal cord reacts in a special way to serious injury - it shuts down (spinal shock). Until recently, doctors did not know how to deal with damaged area syndromes and bring the victim out of shock. To date, this condition has been studied quite well and after a few weeks the patient regains consciousness. Throughout spinal shock, the body is connected to intensive care devices that maintain breathing and heartbeat, as well as the tone of muscle joints.
After the shock has passed, the human body can be roughly divided into two halves: above the site of injury - controlled by the brain and below the site of injury - controlled autonomously using medical equipment. It is the lower part of the body and the spinal cord that will need to be treated.
If the spine and spinal cord are injured, the victim is immediately provided with medical assistance. Every minute of delay means even more damage to brain cells, their death and irreversible consequences. An urgent operation to remove splinters and fragments of bone structures from the spinal canal, restoration of the lining of the brain and decompression of the nerve roots provide a chance for faster and better further recovery of the body.
At the end of the emergency intervention, as far as possible, doctors restore blood circulation and fix the spine in a motionless state. The patient then remains in the intensive care unit for several weeks under constant observation.
Recovery after injury
Restorative processes of nerve cells in the spinal cord begin in proportion to the retreat of spinal shock. And only when the patient regains full consciousness will doctors be able to objectively assess his condition and chances of recovery. After the end of the resuscitation period, the patient’s condition is monitored by a neurologist and a spine doctor.
In most cases, initially not even damaged, but simply areas of the brain and nerve roots close to the injury and the corresponding body organs can work unstably, which manifests itself in loss of skin sensitivity or inability to move. Regeneration of nerve cells and roots is extremely slow, and the patient’s treatment will be lengthy. After a few months, motor ability and sensitivity of the limbs will gradually begin to return, and the functioning and control of internal organs will improve.
Those functions that have not recovered after one and a half years of treatment can be considered lost forever. But in some cases, brain cells regenerate, but the person is still unable to move or walk. This is explained by the body’s ability to “forget” long-unused muscle activity and atrophy of the muscles themselves.
Specially designed electrical stimulators and work on simulators helped overcome this problem. They allow you to “wake up” dormant connections, activate the work of channels and make them function again. After some time, the patient will be able to stand on his own and walk.
Further treatment for brain damage will take place in spinal rehabilitation centers and manual therapy clinics.
Physiotherapy, massages, swimming, exercise therapy and yoga, acupuncture and reflexology will help the body and human health recover faster. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Functions
Functional anatomy implies that, being part of the central nervous system, the spinal cord performs a reflex and conductive function. In the first case, the body controls the implementation of the simplest actions at the level of reactions contained in the subconscious. A striking example is the initiation of a motor function by withdrawing the hand if the surface is too hot. The limb does this before the person himself understands what happened. The second task of the organ is to transmit nerve impulses to the head section of the central nervous system, along the ascending and descending pathways.
Briefly about the main functions of the spinal cord
Reflex function
This main function of the organ is a response to external irritation. For example, the appearance of a reflex cough due to foreign objects and particles entering the respiratory tract, removing the hand from cactus spines or a source of danger. The impulse enters the spinal canal through motor neurons, which also trigger muscle contraction. This process does not require the involvement of the brain, and the motor reaction occurs without its participation. That is, a person does not even think about his action, often does not realize it.
Children's innate reflexes are checked after birth. They usually include the ability to suck milk, breathe, and jerk their legs. During development, acquired reflexes also appear, which help doctors identify the correct functioning of the arch elements and individual segments of the spinal cord. The test is carried out during a neurological examination. The main emphasis is on the plantar reflex, knee and abdominal. They allow you to check how healthy a person is at one time or another.
Conductor function
Treatment of spinal cord myelitis
Another important function of the spinal cord is conduction. It ensures the transmission of impulses from the skin, mucosal surface, internal organ to the brain and in the opposite direction. The white matter acts as a “conductor”. It is this that carries information about incoming impulses from the outside. Thanks to this ability, a person can characterize any object that surrounds him.
Cognition of the world is carried out through the transfer of information after touch to the brain. It is thanks to this function that a person understands that an object is slippery, smooth, rough or soft. With loss of sensitivity, the patient ceases to understand what is in front of him when touching an object. In addition, the brain receives data about the position of the body in space, tension in muscle tissue or irritation of pain receptors.
No ads 3
Structure and functions of the spinal cord
The Extreme Importance of the Spinal Cord
due to the fact that
it closes most of our reflexes and provides the ability to move
.
The human spinal cord, like all vertebrates, is located in
the spinal canal
. It is a white strand 40-45 cm long, 1 to 1.5 cm wide and weighing about 35 grams. At the top, the spinal cord passes into the lower part of the brain - the medulla oblongata, and at the bottom it ends at the level of the first and second lumbar vertebrae.
The spinal cord does not occupy the entire cavity of the spinal canal: between the walls of the canal and the brain there remains a space filled with adipose tissue
, blood vessels, meninges and
cerebrospinal fluid
.
Cerebrospinal fluid
bathes the spinal cord and protects it from shocks.
The outside of the brain is covered with three membranes
:
hard, cobwebby and
soft .
On the surface of the spinal cord, two longitudinal grooves are clearly visible: anterior and
posterior . They divide it into symmetrical halves - left and right.
31 pairs of spinal nerves arise from the spinal cord
, which divide it into segments.
roots
extend from each nerve to the posterior surface , and the anterior roots extend from the anterior surface to each nerve, respectively.
In the internal structure of this part of the central nervous system
the central canal
filled with cerebrospinal fluid and two parts differing in color are clearly visible
In the middle, around the spinal canal, there is the so-called gray matter.
, which in cross section resembles the appearance of a butterfly, and around
it is white
.
Gray matter
represented by the bodies of neurons and short branching processes -
dendrites
.
And white
consists of long, unbranched axons that form nerve fibers.
In the gray matter, anterior
and
posterior horns , and in the thoracic region there are also lateral ones.
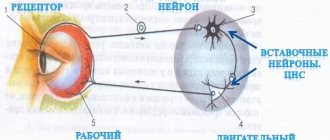
To understand which neurons represent the gray and white matter of the spinal cord, let us turn to the structure of the reflex arc and the direction of passage of the nerve impulse of the somatic reflex.
So, according to the sensitive neuron, which enters the spinal cord as part of the dorsal roots, the nerve impulse
reaches
the interneuron
, which is located entirely in the gray matter.
From it, information is transmitted to the motor neuron
, the body of which is located in the anterior horns of the gray matter, and its processes emerge from the spinal cord as part of the anterior roots.
Next, the nerve impulse enters the mixed spinal nerve
. It is called this because it contains both sensory and motor neurons. Along the mixed spinal nerve, the nerve impulse reaches the performing organ.
Functions of the spinal cord.
Reflex
. If we prick our finger, thanks to a complex system of interactions in the body with the direct participation of the spinal cord, we immediately pull our hand away.
This means that the reflex function of the spinal cord is that reflex arcs are closed on it. Therefore, it is the spinal cord that provides the reflex.
Conductor function
. Despite the fact that the spinal cord provides many of the human reflexes, it is still controlled by another part of the central nervous system - the brain.
If we come to the clinic to take a blood test, then we will not pull our hand away when receiving the injection. The fact is that information from the receptors is transmitted not only to the spinal cord, but also further to the brain, which processes it and in this situation sends instructions to slow down the spinal cord reflex to withdraw the hand.
Thus, the spinal cord conducts nerve impulses to the brain and in the opposite direction. Performing a conductive function.
The speed of passage of a nerve impulse along the arc of a somatic reflex is up to 120 m/s. This means that a nerve impulse will travel from the finger to the brain and back to the finger in about 0.05 seconds. For comparison, we can cite the speed at which we blink. The lowering and raising of the eyelid occurs in approximately 0.4 seconds. That is 10 times slower!
The striated (skeletal) muscles are under the control of the spinal cord, so it controls our movements. And when it is destroyed, for example by a spinal injury, paralysis occurs. That is, a person cannot move any parts of the body, since the nerves are destroyed and the nerve impulse does not reach the performing organs - the muscles.
The command to “contract” is sent to the executive organ, but due to damage to the path along which the signal should pass, it does not reach its destination. For a long time this problem was insoluble. But recent scientific research has made it possible to develop methods for returning victims of spinal injury to an active life.
Let's give a few examples.
40-year-old Pole Darek Fidyka, who was paralyzed from the waist down as a result of knife wounds in 2010, is now able to walk.
This operation, the first in the world, was performed by surgeons in Poland in collaboration with London scientists. For the first time, doctors were able to restore the ability to walk in a person paralyzed as a result of a spinal injury. Cells from the olfactory nerve tissue were transplanted into his spinal cord, since it is the only one that is capable of regenerating.
In parallel with natural methods of spinal cord restoration, artificial ones are also used.
Scientists and engineers from the École Polytechnique Fédérale de Lausanne and the Swiss research center NCCR Robotics have created a unique implant that could lead to a revolution in prosthetics. The implant allows you to “repair” damage to the spinal cord and has already proven itself successfully in many months of experiments on animals. Now researchers are preparing for experiments on humans.
The device is a strip 200 microns thick, which is only 0.2 parts of a millimeter, made of soft and stretchable silicone, which, when deformed, fully retains the ability to conduct electricity and chemicals necessary for stimulating nerves.
Rats with damaged spinal cords, which were experimented on, were able to walk two weeks after implantation, and wear the device for several months without tissue damage.
Traditional methods of treating spinal cord injuries have so far been ineffective because the implanted electrodes are difficult to accurately place within the tissue, and with prolonged use they rub against the tissue and damage the dura mater.
These examples tell us that every year the “repairability” of our body is growing, and humanity is not as fast as we would like, but is moving with confident steps towards immortality.
Lesson summary. The spinal cord is located in the spinal canal. The spinal cord is covered with dura, arachnoid and soft membranes. There are gray and white matter of the spinal cord. 31 pairs of spinal nerves arise from the spinal cord. The nerve impulse enters the spinal cord through the dorsal roots and dorsal horns (through sensory neurons), and exits through the anterior horns and anterior roots (through motor neurons). The spinal cord performs a reflex and conductive function.
What organs does the spinal cord control?
It is also important to understand which internal organs are connected to the spinal cord and may suffer if a particular area of the spine is damaged. Specific spinal segments control specific parts of the body by transmitting nerve impulses and transmitting responses along motor neurons. What each vertebra is responsible for can be clearly seen in the table.
| Back segment | Vertebra serial number | Controlled internal organs |
| Cervical | 3-5 | Diaphragm |
| Cervical | 6-8 | Articular tissue of the upper limbs |
| Chest | 1,2, 5-8 | Muscle tissue and epidermis of the hands, elbows and forearms |
| Chest | 2-12 | Muscles, skin of the body |
| Chest | 1-11 | Intercostal muscles |
| Chest | 1-5 | Heads, heart |
| Chest | 5-6 | Lower esophagus |
| Chest | 6-10 | Gastrointestinal tract |
| Lumbar | 1-2 | Prostate, groin area, adrenal glands, bladder, uterus. |
| Lumbar | 3-5 | Muscles and skin of the legs |
| Sacral | 1-2 | Muscle tissue and epidermis of the lower extremities |
| Sacral | 3-5 | External genitalia, reflex centers, erectile dysfunction and defecation |
Damage to the spinal cord in a specific section negatively affects the functioning of these internal organs. In some cases, dysfunction occurs before vertebral compression or displacement is detected.
Reflex activity of the spinal cord
A huge number of reflex arcs are closed in the spinal cord, with the help of which both somatic and autonomic functions of the body are regulated. Among the simplest reflex reactions are tendon reflexes and stretch reflexes , caused by irritation of the stretch receptors of the same muscle that develops the reflex contraction. The central endings of afferent fibers from stretch receptors form synapses directly on motor neurons without additional switching on interneurons. Thus, the arc of these reflexes may be monosynaptic in nature. This circumstance, as well as the high speed of conduction along afferent fibers coming from muscle receptors and along the axons of α-motoneurons, provide a short reflex time (which is especially demonstrative in the case of tendon reflexes).
Tendon reflexes are easily evoked by a short blow to the tendon and have important diagnostic value in neurological practice. The reflex reaction manifests itself in the form of a sharp muscle contraction. Tendon reflexes are especially pronounced in the leg extensor muscles, such as the quadriceps femoris (patellar reflex) or the triceps surae (Achilles reflex). However, tendon reflexes are also evoked in the flexor muscles. On the hand they are clearly visible on the biceps and triceps muscles, on the face - on the muscles of the lower jaw.
The speed of muscle contraction and the absence of aftereffects are due to the method of inducing the tendon reflex. An adequate stimulus for the corresponding receptors is muscle stretching. Tapping the tendon only stretches the muscle for a very short period of time.
But at the same time, stretch-sensitive receptors are activated with a high degree of synchrony.
Since the afferent fibers coming into the spinal cord from the stretch receptors are a fairly homogeneous group in diameter and conduction velocities, afferent impulses arrive at the motor neurons in the form of a synchronous wave. As a result, the motor neurons respond with little temporal dispersion, sending a synchronous discharge to the motor nerve that produces a brief muscle twitch similar to the response of a muscle to a single electrical stimulus to the motor nerve.
The stretch reflex, which occurs with adequate stimulation of the same muscle receptors, is characterized in a completely different way. Natural stretches are usually applied to the muscles by gravity. Thus, when standing, the quadriceps muscle is stretched due to the tendency of the knee to bend under the influence of gravitational forces.
The afferent impulses that arise in response to this stretch are characterized by significant asynchrony, since numerous stretch receptors, under the influence of a constant load, generate rhythmic impulses, the frequency of which is determined by the individual threshold of each receptor. Motor neurons receive long-term asynchronous impulses and themselves discharge asynchronously. As a result, the muscle responds with a smooth, prolonged contraction that automatically counteracts the force of gravity. This determines the great physiological significance of the stretch reflex as a mechanism for maintaining an upright posture or standing.
Reflex responses are more complexly organized, expressed in coordinated flexion or extension of the muscles of the limb. Flexion reflexes are aimed at avoiding various damaging influences. Therefore, the receptive field of the flexion reflex is quite complex and includes various receptor formations and afferent pathways of different speeds.
The flexion reflex occurs when pain receptors in the skin, muscles and internal organs are irritated. The afferent fibers involved in these irritations have a wide range of conduction velocities - from myelinated fibers of group A to unmyelinated fibers of group C. All the various afferent fibers, impulses along which lead to the development of the flexion reflex, are combined under the name flexion reflex afferents .
The central time of the flexion reflex is quite long, which is due to its polysynaptic nature. Flexion reflexes differ from the intrinsic muscle reflexes - myostatic and tendon - not only in the large number of synaptic switches on the way to motor neurons, but also in the involvement of a number of muscles, the coordinated contraction of which determines the movement of the entire limb.
Simultaneously with the excitation of motor neurons innervating the flexor muscles, reciprocal inhibition of the motor neurons of the extensor muscles occurs.
After decapitation, the frog is suspended by the jaw. The dorsal roots on the right side are cut, as a result of which there is no flexion tone on this limb.
With sufficiently intense stimulation of the receptors of the hind limb, irradiation of excitation occurs and the muscles of the forelimb and torso are involved in the reaction. When motor neurons on the opposite side of the body are activated, not flexion is observed, but extension of the muscles of the hind limb is observed - a cross extensor reflex.
Extensor reflexes, in addition to the myostatic reflexes and cross-extensor reflex already discussed above, include a number of polysynaptic reflexes that arise when the receptors of the foot are irritated.
Rhythmic and postural reflexes, or position reflexes, are even more complex. Rhythmic reflexes in mammals include the scratching reflex. Its analogue in amphibians is the rubbing reflex. Rhythmic reflexes are characterized by the coordinated work of the muscles of the limbs and torso, the correct alternation of flexion and extension of the limbs along with the tonic contraction of the adductor muscles, setting the limb in a certain position to the skin surface.
Postural reflexes are a large group of reflexes aimed at maintaining a certain posture, which is possible in the presence of a certain muscle tone. An example of a postural reflex is the flexion tonic reflex, which in a frog determines the main posture - sitting. Even in a decapitated frog suspended from a tripod, the hind limbs are always somewhat bent and the flexion tone disappears only after the destruction of the dorsal phyosta or cutting of the dorsal roots. The differences in the tone of the flexor muscles are especially clear if the dorsal roots are cut on one side, leaving the other intact (Fig. 83).
The flexion tonic reflex is also observed in mammals, which are characterized by a tucked position of the limbs (rabbit). At the same time, for most mammals, the main importance for maintaining body position is not flexion, but extensor reflex tone.
Due to the fact that the cervical segments of the spinal cord play a particularly important role in the reflex regulation of extensor tone, cervical tonic positional reflexes are specially distinguished. These reflexes were first described by the Dutch physiologist R. Magnus (1924).
The receptive field of cervical tonic reflexes is the proprioceptors of the neck muscles and fascia covering the cervical spine. The central part of the reflex arc is polysynaptic in nature, that is, it includes interneurons.
The reflex reaction involves the muscles of the trunk and limbs. In addition to the spinal cord, it also involves the motor nuclei of the brain stem, which innervate the muscles of the eyeballs.
Cervical tonic reflexes occur when turning and tilting the head, which causes stretching of the neck muscles and activates the receptive field of the reflex. Reflexes that are usually studied in humans are given in Table. 5.
In addition to the reflexes discussed above, which belong to the category of somatic, as they are expressed in the activation of skeletal muscles, the spinal cord plays an important role in the reflex regulation of internal organs, being the center of many visceral reflexes. These reflexes are carried out with the participation of preganglionic neurons of the autonomic nervous system located in the lateral and ventral horns of the gray matter. The axons of these nerve cells leave the spinal cord through the ventral roots and end on the cells of the sympathetic or parasympathetic autonomic ganglia. Ganglion neurons, in turn, send axons to the cells of various internal organs, including smooth muscles of the intestine, blood vessels, bladder, glandular cells, and heart muscle.
Risk of organ damage
Due to the characteristic structure of the brain, it is connected to most systems in the body. The integrity of its structure is extremely important for the correct functioning of the musculoskeletal system and the health of internal organs. Any injury, regardless of severity, can lead to disability. Sprains, dislocations, disc damage, vertebral fractures with or without displacement can cause spinal shock and paralysis of the legs, and disrupt the normal functioning of the cords.
Severe injuries result in shock lasting from several hours to several months. In this case, the pathological condition is accompanied by a number of neurological symptoms. These include numbness, sensory disturbances, pelvic organ dysfunction, and inability to control the process of urination and bowel movements.
Treatment of minor spinal injuries is carried out on an outpatient basis, using medications, therapeutic exercises and massage. Severe injuries require surgical intervention, especially if compression of the spinal cord is detected. Cells are quickly damaged and die, so any delay can cost a person’s health. The recovery period after such an intervention is up to two years. Various physiotherapeutic procedures help with this, for example, reflexology, ergotherapy, electrophoresis, magnetic therapy, etc.
The spinal cord is a key element of the human central nervous system, which is connected in one way or another with almost all internal organs and human muscle tissue. The specific structure allows you to transmit impulses and signals, ensure full motor activity, and perform a number of other functions.
Participation of the spinal cord in the regulation of muscle tone
Regulation of muscle tone is of a reflex nature and is carried out through myotatic and postural-tonic reflexes.
The myotatic reflex is a stretch reflex that begins with irritation of the muscle spindle. Almost every muscle contains muscle stretch receptors, called “muscle spindles” because of their shape (Fig. 2).
The muscle receptor consists of striated intrafusal muscle fibers surrounded by a connective tissue capsule and has the shape of a spindle. The length of intrafusal muscle fibers is 4 - 7 mm, thickness 15 - 30 µm. Muscle spindles are located parallel to the skeletal muscle and their ends are attached to the connective tissue membrane of the bundle of extrafusal muscle fibers using tendon-like strips of connective tissue 0.5 - 1 mm long.
The mechanism for regulating muscle tone is presented in Figure 2. Stretching of extrafusal muscle fibers (with relaxation of striated muscle fibers) leads to stretching of the muscle spindle. When the muscle spindle is stretched, the nuclear bursa is stretched and the stretch receptor is excited. Impulses enter the spinal cord to α-motoneurons. Excitation along the axons of α-motoneurons causes contraction of extrafusal muscle fibers.
Fig.2. Scheme of regulation of muscle tone.
1 – extrafusal fibers; 2 – muscle spindle; 3 – intrafusal
fibers; 4 – efferent nerve fibers; 5 – alpha motor neurons;
6 – gamma motor neurons
Gamma loop:
A number of effects from muscle and tendon receptors go not only to α-motoneurons, but also along the axon collateral to γ-motoneurons: γ-motoneurons are excited → send impulses to intrafusal fibers → intrafusal fibers contract → muscle spindle stretches → receptor is excited → impulses go to spinal cord → activation of α-motoneurons → contraction of extrafusal fibers.
Cervical posture-tonic reflexes
spinal cord are aimed at maintaining posture. With their help, muscle tone is regulated. These reflexes arise from the proprioceptors of the muscles and fascia of the neck. Switching from these receptors occurs at the level of the cervical spinal cord and leads to changes in muscle tone when the position of the head and neck changes.
Segmental and intersegmental principle
Spinal cord works
The spinal cord consists of 31-32 segments. Each segment corresponds to two pairs of roots (corresponding to the number of segments, 31-32 pairs of anterior motor roots exit the spinal cord and 31-32 pairs of posterior sensory roots enter it). When projecting segments of the spinal cord onto the vertebrae, it is necessary to take into account the discrepancy between the lengths of the spinal cord and the spine. In the cervical region, the segments are located 1 vertebra higher than the corresponding vertebra; upper thoracic - by 2, lower thoracic - by 3 (example: the V cervical segment is located at the level of the IV cervical vertebra, the V thoracic - at the level of the III thoracic vertebra, the XI thoracic - at the level of the VIII thoracic vertebra, etc.). The lumbar and sacral segments and vertebrae are in great disparity: the lumbar segments are at the level of the X, XI, and XII thoracic vertebrae; sacral – XII thoracic and I lumbar. There are no morphological boundaries between the segments of the spinal cord, therefore the division into segments is functional and is determined by the distribution zone of the dorsal root fibers in the segment and the zone of cells that form the anterior root. The part of the body innervated by the fibers of one segment is called the metamer (the area of the skin innervated by the sensory fibers of the segment is called the dermatome). Each segment innervates through its own metamer. This is the segmental principle of the spinal cord. The intersegmental principle of the spinal cord is that each segment of the spinal cord innervates not only its own metamer, but also the metameres of the upper and lower adjacent segments. As a result of the overlap of nerve fibers, each metamer of the body is innervated by three segments and transmits signals to 3 segments of the spinal cord, which increases the reliability of regulatory mechanisms.
Structural organization and functions of the medulla oblongata
The medulla oblongata is a continuation of the spinal cord and is about 25 mm long. Unlike the spinal cord, its gray matter is located not in the center, but on the periphery in the form of nuclei.
In the medulla oblongata there are nuclei of the VIII-XII pairs of cranial nerves through which the regulation of sensitive (sensory), motor (somatic) and autonomic (parasympathetic) functions is carried out: sensory nuclei of the vestibular-cochlear nerve (n.vestibulocochlearis, VIII), nuclei of the glossopharyngeal nerve (n. glossopharyngeus, IX), nuclei of the vagus nerve (n. vagus, X), motor nucleus of the accessory nerve (n. accessorius, XI), motor nucleus of the hypoglossal nerve (n. hypoglossus, XII). In addition, in the RF of the medulla oblongata there are vestibular nuclei (medial - Schwalbe's nucleus, superior - Bekhterev's nucleus, lateral - Deiters' nucleus and inferior - Roller's nucleus), which receive impulses from the receptors of the semicircular canals.
Functions of the medulla oblongata
The medulla oblongata performs sensory, conductive and reflex functions.
— Touch functions
are carried out due to the receipt of afferent information into the medulla oblongata from taste receptors, auditory and vestibular receptors along sensory fibers to the nuclei of the corresponding cranial nerves and from receptors of the thoracic and abdominal organs (see above). At the level of the medulla oblongata, a primary analysis of the strength and quality of the stimulus is performed.
— Conductor functions
. All ascending and descending tracts of the spinal cord pass through the medulla oblongata. Here are the intersections of the descending pyramidal paths and the ascending tract of Gaulle and Burdach.
— Reflex functions
.
The centers of numerous reflexes are localized in the medulla oblongata. For example, a number of protective reflexes: gag reflex
(from the receptors of the root of the tongue, pharynx, stomach, intestines, peritoneum, vestibular apparatus → along the fibers of the glossopharyngeal, vagus or vestibular nerve → to the vomiting center of the medulla oblongata → along the efferent fiber of the vagus nerve to the esophagus, stomach, intestines and through the spinal motor centers to the diaphragm and abdominal wall muscles);
cough reflex
(from the receptors of the larynx, trachea and bronchi → along the sensory fibers of the vagus nerve → to the cough center of the medulla oblongata → efferent impulses to the spinal centers of the respiratory muscles);
sneezing reflex
(from the receptors of the nasal cavity → to the sneezing center of the medulla oblongata → efferent impulses to the spinal centers of the respiratory muscles), as well as
reflexes of lacrimation and eyelid closure.
Also, the medulla oblongata, together with other structures of the brain stem, is involved in the implementation of
postural maintenance reflexes (vestibular postural-tonic reflexes).
In the medulla oblongata, in addition to the centers of protective reflexes, in the area of the reticular formation there are vital centers - the vasomotor and respiratory centers.
Features of the structural organization of the reticular formation
brain stem
The reticular formation (RF) is located in the gray matter of the medulla oblongata, midbrain, diencephalon, and partly the spinal cord and regulates the level of activity of the cerebral cortex, cerebellum, thalamus, and spinal cord. The RF is formed by neurons that have long, poorly branched dendrites and a short, well-branched axon. The morphological structure of the reticular formation is very reminiscent of a mesh, and it is on this basis that the German anatomist Otto Deiters called this structure “reticular formation” (Latin reticulum - mesh, formatio - formation) (1865). RF neurons receive information from different receptors. These are multimodal neurons that have large receptive fields, have spontaneous activity, increased excitability, high lability (up to 1000 pulses/sec), and high sensitivity to metabolites, hormones, barbiturates and other pharmacological drugs.
Neurophysiology of sensory pathways of the spinal cord
1. The dorsal (posterior) columns of the spinal cord are a powerful system of fibers of various origins (Fig. 6.21). In evolution, the posterior columns of terrestrial mammals are formed in connection with the development of the limbs, when the need arises for a subtle analysis of information from the joints and skin, without which walking, running, jumping, maintaining balance and body position in space are impossible. The progressive development of the dorsal columns in the evolution of vertebrates is closely related to the development of the somatosensory cortex of the cerebral hemispheres.
The fibers of the dorsal roots, entering the spinal cord, are divided into two branches: long (ascending) and short (descending). The nuclei of the dorsal columns (grass and cuneate) in the medulla oblongata reach only about a quarter of the myelinated fibers; the remaining axons end on interneurons of the spinal cord.
Diagram of the main ascending tracts of the spinal cord
The axons of the neurons of the dorsal column nuclei (grass and cuneate) cross and form the medial lemnisci, which go to the nuclei of the ventrobasal thalamus. The fibers that make up the posterior columns in the spinal cord gradually become thinner, since along the way they send a large number of collaterals to the interneurons of the spinal cord, so the speed of impulses decreases from 90-120 m/s - at the point of entry into the spinal cord to 20-40 m/s c at the level of the cervical upper segments of the spinal cord.
The fiber system of the dorsal columns contains afferents from many types of receptors, in particular in animals - from receptors on hair follicles, joints, paw pads, bases of claws and other formations. Muscle afferents from the limbs also ascend as part of the dorsal columns and end on neurons of the nuclei of the medulla oblongata, as well as on neurons of the dorsal horn of the cervical upper segments of the spinal cord. The axons of these 2nd order neurons cross and join the fibers of the medial lemniscus, which, switching through the nuclei of the ventrobasal complex, are projected onto the cerebral cortex at the border of the sensory and motor zones (area 3, according to Brodmann). A significant part of the afferent fibers from muscle and tendon receptors is not part of the posterior columns. These fibers, starting from the lumbar segments of the spinal cord and above, switch on neurons of the clark columns, the axons of which form powerful sensory tracts to the cerebellum.
The joint capsules and joint surfaces have a variety of receptors, which are collectively called articular receptors. According to modern data, two types of responses are distinguished in the articular nerve: rapidly adapting and slowly adapting, the latter being more numerous. Accordingly, two types of receptors are distinguished. Slow adapting receptors, being the most typical joint receptors, report the position of the bones that form a given joint. In the articular nerves, fibers are found in which discharges occur both during flexion and extension of the joint. Fibers were also discovered, the discharge of which, depending on the flexion or extension of the joint, increases or decreases (direction-sensitive responses). The same joint movement can cause a decrease in impulses in one afferent fiber and an increase in another fiber. Information from articular receptors to the supraspinal centers is carried out through the system of fibers of the posterior columns.
The fibers of the posterior columns also conduct afferent signals from internal organs. Impulses from the pelvic nerve reach the suprasegmental structures not only along the dorsal cords (posterior columns), but also along the ventrolateral cords, part of the spinothalamic tracts of the spinal cord. The speed of impulses from internal organs in the posterior columns, for example, of a cat, is 35-75 m/s, in the ventral columns - 21-38 m/s and lateral - 17-32 m/s.
2. The spinocervical tract is formed by the axons of neurons, the bodies of which are located at the base of the gray matter of the dorsal horn of the spinal cord (see Fig. 6.21). Next, the fibers of the tract pass ipsilaterally as part of the lateral funiculus and end on the neurons of the cervical lateral nucleus, localized in the upper segments of the cervical gray matter of the dorsal horns of the spinal cord. At the same level, the axons of the neurons of this nucleus intersect and, as part of a special portion of the medial lemniscus, are sent to the ventrobasal complex of the thalamic nuclei.
It is known that the cervical lateral nucleus in humans is represented by scattered cells in the cervical segments of the spinal cord. In cats, dogs, and lower monkeys, this nucleus is very well developed. Excitation from low-threshold skin receptors, including hair follicle receptors, converges on the neurons of the spinocervical tract. A number of neurons are excited when the skin is pinched or pressed; the size of their receptive fields can be large and even occupy the entire ipsilateral half of the body. Despite the greater number of switches (spinal level, cervical lateral nucleus, ventrobasal thalamus, cerebral cortex), excitation along the spinocervical tract arrives in the cerebral cortex 2-5 ms faster than along the fibers of the dorsal columns. This is explained by the fact that the conduction speed along the fibers of the posterior columns is less than through the fibers of the spinocervical tract.
In mammals (including humans), the projection of the entire body is organized along the dorsal columns and spinocervical tract (in humans, mainly along the dorsal columns) in the postcentral cortex of the cerebral hemispheres (Fig. 6.22). In this case, the following principle is observed: the higher the density of receptors in the skin covering the corresponding part of the body, the larger the area this projection is represented in the cerebral cortex. Please note that the hands, especially the thumb, the oral region, including the tongue, vocal cords, etc., are represented in particular detail in the human cerebral cortex.
Sensory representation of the body in the sensory fields of the cerebral cortex
3. The spinothalamic tract consists of the thinnest myelinated afferents (up to 6 µm in diameter), as well as unmyelinated fibers of the dorsal roots. They enter the gray matter of the spinal cord and end at the neurons of the base of the gray matter of the dorsal horn. In the gray matter of the spinal cord, the axons of some of these neurons cross, and the other part goes ipsilaterally, forming the spinothalamic tract. Thus, the spinothalamic tract projects to the nuclei of the thalamus (ventral posterolateral, parafascicular and central lateral nuclei) bilaterally. Part of the nerve fibers of the tract switches to the neurons of the brain stem, the axons of some of these neurons move to the contralateral side and also go to the thalamus.
The fibers of the spinothalamic tract transmit information about pain, pressure and temperature. The neurons of this tract have extensive cutaneous receptive fields, located bilaterally in some neurons, covering both hind or both forelimbs, and sometimes even the entire surface of the body. Neurons activated by stimulation of one limb tend to be inhibited by stimulation of the other, whereas neurons with limited cutaneous receptive fields are often inhibited by the surrounding skin surface. Currently, it is believed that this tract conducts generalized sensations and transmits information only about the quality of the stimulus and its rough localization.
Thus, two systems are projected into the thalamus: the dorsal columns (in a number of mammalian species there is also the spinocervical system) and the spinothalamic tract. These two systems differ functionally: the first carries information about the location and modality of the stimulus (protopathic sensitivity), while the second provides generalized forms of sensation (epicritic sensitivity).