Definition
“Tethered spinal cord syndrome” is an adaptation of the English term “the tethered spinal cord syndrome” (Yamada S., 1981). “tether” in the original name , which literally means a leash for pets , is associated with the desire to most accurately reflect the essence of the pathological process it describes. It is the stretching of the spinal cord, which develops as a result of restriction of its mobility, that is, fixation, that leads to the negative impact and development of clinical manifestations of FSM.
Yamada, S. (Ed.). (2010). 3 Pathophysiology of Tethered Cord Syndrome. Tethered Cord Syndrome in Children and Adults. doi:10.1055/b-0034-80501
“tethered spinal cord” first used by Hoffman to describe the results of treatment of 31 patients suffering from pelvic disorders in combination with motor disorders and decreased sensitivity in the lower extremities. Symptoms in all patients regressed after excision of the thickened filum terminale. Based on the data obtained, the authors concluded that the pathological process develops as a result of stretching of the caudal parts of the spinal cord (Hoffman HJ, 1976).
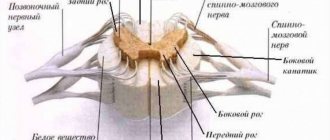
Thickenings and grooves
In the part of the nervous system under consideration, two thickenings are distinguished:
- cervical thickening;
- lumbosacral thickening.
The dividing boundaries are considered to be the anterior median fissure and the posterior sulcus. These boundaries are located between the halves of the spinal cord, which are symmetrically located.
The median fissure is surrounded on both sides by the anterior lateral groove. The motor root originates from the anterior lateral sulcus.
The organ has lateral and anterior cords. The anterior lateral groove separates these cords from each other. The role of the posterior lateral sulcus is also important. At the back it plays the role of a kind of border.
Pathogenesis
It is known that the spinal cord is protected from excessive stretching by the so-called “dentate ligaments” , which fix the spinal cord in the lumen of the spinal canal (Tunituri AR, 1977). While at the level of the cervical and thoracic spine they are significantly developed (Breig A., 1970; Tubbs RS, 2001), at the level of the lumbar spine they are not , and stretching of the caudal parts of the spinal cord is prevented only by the elastic properties of the terminal filament (Tani S., 1991 ).
Yamada, S. (Ed.). (2010). 3 Pathophysiology of Tethered Cord Syndrome. Tethered Cord Syndrome in Children and Adults. doi:10.1055/b-0034-80501
When the terminal filament was stretched in patients with FSM, its elongation was observed by no more than 10%, while normally it elongates by 50% or more (De Vloo P., 2016). Light microscopy of a section of a pathologically altered filament terminale in patients with FSM revealed a predominance of fibrous tissue; when stained for elastin, its content was minimal (Hendson G., 2016). Based on the data obtained, it was hypothesized that SFSM develops as a result of tension in the caudal parts of the spinal cord between the last pair of odontoid ligaments and any inelastic structure that fixes it caudally (Yamada S., 1981).
Yamada, S. (Ed.). (2010). 3 Pathophysiology of Tethered Cord Syndrome. Tethered Cord Syndrome in Children and Adults. doi:10.1055/b-0034-80501
In 1981, S. Yamada, in an experiment on cats, demonstrated a slowdown in metabolism in the tissues of the caudal parts of the spinal cord during stretching and its subsequent restoration when the tension was removed. A few years later, in 1987, it was officially proposed that “tethered spinal cord syndrome” be considered a scientifically based clinical diagnosis (McLone D., 1987), from which point this term began to appear more and more often in the literature.
Currently, most domestic and foreign specialists characterize FMS as a combination of motor, sensory, trophic disorders in the lower extremities, as well as pelvic disorders and musculoskeletal deformities that develop as a result of immobilization and stretching of the caudal parts of the spinal cord in pathologies of the filum terminale (“tight filum”) terminale” – inelastic filum terminale, filum terminale lipoma, etc.), myelodysplasias (MMC, spinal lipomas), complex spinal dysraphisms (diastematomyelia, dermoid, epidermoid, enteric cysts, dermal sinus), as well as post-inflammatory and postoperative scar-proliferative changes terminal cistern (leptopachine meningitis, arachnoid cysts, etc.) (McLone DG, 1997; Iskandar BJ, 1998; Tortori–Donati P., 2000;).
The reasons for the development of FSM are most often the consequences of correction of spina bifida, as well as Spina Bifida Occulta
How bone marrow donation works: myths, fears, side effects
For transplantation, compatibility of blood groups and Rh factors is not necessary; genetic compatibility is more important. Among an ideally suitable unrelated donor and a related donor who does not match on all points, doctors will most likely choose the latter, because with it there is a lower probability of refusal to donate.
Sometimes 50-70 donors are suitable for a patient at once, but it happens that the “genetic twin” is not in the registry at all. In the latter case, you can try to organize donor campaigns so that more people undergo typing, but in any case, if a suitable donor is not in the bank, it will not be possible to help the patient. Every year at least three thousand people die because they could not find a suitable donor.
A patient and donor with the same ethnic background are more likely to be a match. The more people undergo typing, the more different genetic data there are in the registries, which means the higher the likelihood of patient and donor compatibility.
According to the American company Be The Match, the people who have the most problems finding a bone marrow donor are people of color, Indians, Alaska Natives, Asians, Native Hawaiians and other Pacific Islanders, Hispanics and mestizo. The American Institute of Justice reports that African Americans who do not have a related donor find a match only 25% of the time, and that if a donor is found, 80% of the time it is the only option on the registry. For Asians this figure is 40%, for Latin Americans - 45%, for Europeans - 75%. The specific percentage for mestizos is not given in the statistics, but the institute clarifies that for them the situation is much worse.
Why are bone marrow donors needed?
More than 5 thousand Russians require bone marrow transplantation annually, of which 4,214 are needed for adults and 900 for children. In Russia there is no general data register for donors; each bank counts its donors itself. According to oncologist-hematologist Sergei Semochkin, the largest stem cell bank in Russia is located in Kirov. There are 35,787 people registered there.
Another large registry of bone marrow donors in our country is managed by Rusfond - the National Register of Bone Marrow Donors named after Vasya Perevoshchikov. It has existed since 2013 and unites 12 regional Russian registers and one Kazakh one. As of October 31, 2021, there were 29,178 bone marrow donors.
There are 35.6 million people registered in the world bone marrow bank (Bone Marrow Donors Worldwide). However, it is difficult to find a donor compatible with a Russian there - in our country there are many nationalities and genetic combinations that are not found anywhere else in the world. The likelihood that a Russian person will find a suitable donor in the domestic registry is higher than in foreign ones.
Semochkin gives an example that often Caucasians cannot find their “genetic twin” in the European database. But they have more children in the family, so the likelihood of finding a related donor is higher. Small ethnic groups, for example, residents of the Far North, also have a huge problem with finding donors. As a rule, they fail to find a donor.
The only solution to the problem is for as many people of different nationalities as possible to join the national register. As Semochkin explains, the cost of cell transplantation and all other procedures for a Russian patient with a Russian donor does not exceed 160,000 rubles. At the same time, procedures and transplantation with a donor from a European bank require about 20,000 euros. The state cannot allocate that kind of money, and patients, as a rule, do not have it either - funding falls on charitable foundations.
How to become a donor?
In Russia, any healthy citizen of the Russian Federation without chronic diseases aged 18 to 45 years, and in some cases up to 50 years, can become a donor. Age matters: the younger the donor, the higher the concentration of cells in the transplant and their “quality”.
MGIMO master's student Irina became a bone marrow donor at the end of October this year. Before that, from the age of 18, she regularly donated blood and platelets to donor organizations. Three years ago, she read Valery Panyushkin’s column “Meeting” about how the donor and recipient met, and finally decided to donate bone marrow.
The first step is donating blood for typing. This can be done in any of the large private medical laboratories or in the laboratories of some medical centers or registries. You can view the full list of centers that allow you to get to Rusfond Bank here.
Irina chose the National Medical Research Center for Hematology. There she donated about 10 milliliters of blood for typing and signed an agreement to join the register. It does not oblige the donor to anything - you can refuse at any time. But this is important for the recipient - 10 days before the stem cell transplant, high-dose chemotherapy is carried out, which completely destroys the hematopoietic and immune systems. Therefore, a last-minute refusal can be disastrous for someone waiting for a transplant.
A month and a half after typing, Irina received a message by email that everything was fine with the tests and she was included in the register.
Classification
It is obvious that a significant contribution to the development of clinical symptoms in spinal dysraphism , in addition to stretching, can be made by volumetric effects (compression), deformation, as well as congenital disorders of cyto- and angiomyeloarchitecture (Kumar R., 2010). Based on the concept of FSM as a reversible pathological condition, S. Yamada and DJ Won proposed to separate processes caused by limited mobility of the spinal cord (true FSM) and conditions that have clinical manifestations similar to FSM, which include in their pathogenesis, in addition to stretching, other unfavorable factors effects (compression, deformation, etc.), as well as pathologies that are not at all related to SFSM, caused mainly by disruption of the formation of the spinal cord and having an unfavorable prognosis for surgery aimed at eliminating the fixation of the spinal cord (Yamada S., 2007). The first category included patients with anomalies of the filum terminale , hernias of the sacral localization and small caudal lipomas, in which the main contribution to the pathogenesis of clinical manifestations is made by longitudinal stretch of the spinal cord. The second category includes patients with myelomeningocele of the lumbar spine, lipomyelocele and repeated scar fixation of the spinal cord. In these patients, obviously, only part of the symptoms presented relates to FMS and can regress after surgery. The third category of patients included children with spina bifida of the thoracic spine, accompanied by congenital paraplegia and incontinence (Yamada, 2007).
Classification of SFSM according to Yamada, Won 2007
In accordance with the described categories, expected results and indications for surgery were distributed. When fixation was eliminated in the first category of patients, a complete regression of symptoms , and patients from the third category have practically no chance of restoring lost functions (Liptak GS, 1995).
Meninges
- Hard shell. It is located immediately behind the periosteum of the spine, but does not adhere closely to it. The epidural space is located between the periosteum and the dura mater. The tissue of the hard shell is connective; it contains vessels, lymphatic and circulatory. The epidural space is filled with fatty tissue. Venous plexuses are also located here.
- The arachnoid membrane is a network of thin plates of connective tissue, similar in structure to a spider’s web. The plates are composed of collagen and elastic fibers. Between the arachnoid and soft membrane there is a subarochnoid space with cerebrospinal fluid, which ensures the exchange and nutrition of neurons.
- Soft shell. This is a vascular environment that has serrated ligaments for fixation and provides communication and nutrition between the cerebrospinal fluid and the brain.
Epidemiology
Despite the fact that the true incidence of FMS is unknown, and the number of patients with classic FMS caused by anomalies of the filum terminale, according to some data, does not exceed 0.1% in the pediatric population (Bademci G., 2006), only in the USA during the period From 1993 to 2002, more than 9,000 operations were performed to eliminate spinal cord tethering (Lad SP, 2007).
SFM manifests itself during periods of accelerated child growth
According to most authors, FMS is characterized by a progressive course , while the age at which deterioration of the condition may occur varies from 8 months to 16 years and does not always correspond to periods of accelerated growth. It is noted that at older ages, the manifestation of FMS may be associated with physical activity or injury (Pang D., 1982)
During the first year of life, a child grows by an average of 20 cm due to lengthening of the body
Experimental data suggest that timely removal of fixation can lead to restoration of spinal cord function (Yamada S., 1981; Schneider SJ, 1993). However, it has been shown that sudden excessive stretching of the spinal cord can lead to irreversible structural changes (Kocak A., 1997). In this case, in contrast to gradual long-term stretching (Pfister BJ, 2004), the formation of a persistent neurological deficit is most likely due to rupture of the spinal cord pathways (Yamada S., 2003).
In this regard, concern is raised by the fact that children suffering from FMS often remain under the supervision of orthopedists and urologists for a long time without receiving appropriate neurosurgical treatment. This can lead to the formation of irreversible neurological and orthopedic deficits, as well as persistent pelvic disorders
Main functions of bone marrow
The first and main task of the bone marrow is the production of blood elements, or hematopoiesis. Therefore, disturbances in the process of hematopoiesis are directly related to problems in the functioning of the bone marrow. If it does not work properly, a person’s well-being may deteriorate for seemingly no apparent reason.
Insufficient bone marrow activity can cause conditions such as:
- weakness and fatigue (due to lack of hemoglobin, which is responsible for transporting oxygen);
- fever (due to insufficient white blood cells);
- tendency to infectious diseases (due to a decrease in white blood cells, which are necessary to fight infections);
- uneven breathing (due to a lack of red blood cells and the resulting oxygen starvation);
- bruising or bleeding (due to platelet deficiency).
In addition, if we remember that it is thanks to the blood flow that all tissues and organs receive oxygen and nutrients, then it becomes clear: absolutely every cell of the human body depends on the bone marrow.
Bone marrow is also the core element of the lymphatic system. All lymphocytes originate in this tissue. And if we take into account that the immune system directly depends on the efficiency of the lymphatic system, it turns out that without bone marrow immunity would not exist. Most blood antibodies that protect the body from pathogens are synthesized in the bone marrow.
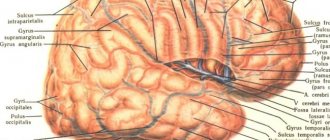
Clinical diagnosis
Timely detection of FSM at the stage of the disease when the pathological process is still reversible is facilitated by alertness regarding the presence of skin stigmas of dysembryogenesis and musculoskeletal deformities in newborns (Aldana PR, 2009).
Skin manifestations are detected in 40% of children with FSM. These include local hypertrichosis (“faun’s tail”), subcutaneous lipoma, cutaneous angioma, age spots, rudimentary skin growths in the lumbosacral region.
Skin “stigmas” of dysembryogenesis: hypertrichosis, subcutaneous lipoma, cutaneous angioma.
Congenital musculoskeletal deformities in the form of shortening, hypotrophy of the lower extremities, and foot deformities may attract attention Asymmetrical deformations are considered characteristic of FSM - “hollow”, equinovarus foot, “trigger-shaped” toes, etc. Although asymmetry of the lower extremities is often detected with FSM, pronounced hypotrophy of one of the lower extremities (“stork leg”) is rare (Lagae L., 1990 )
“External” manifestations of FSM in children
FSM is manifested by progressive pelvic disorders (incontinence or retention of urine and feces). Parents may experience constant leakage in the child, as well as frequent constipation or episodes of stool.
At an older age, you can find out whether the gait has changed, whether awkwardness has appeared when walking or running, whether the sole of the shoe has changed over time, in which direction it has become thinner (outward or inward) (Elikbaev G.M., 2008). There may be pain when turning the body, flexing or extending. In pre-adolescence, the main clinical manifestations of FMS are weakness in the legs, gait disturbances, urinary incontinence, and newly developed foot deformities (Yamada S., 2004).
Clinical symptoms of FSM
Adolescents with FSM are characterized by progressive scoliotic deformity of the spine, as well as urinary incontinence, mainly in the form of episodes of gelastic incontinence, often interpreted as a manifestation of a urinary tract infection.
During periods of accelerated growth, spinal deformity may be the main complaint (Trivedi J., 2002). In this case, the development of deformation of one of the feet (hollow foot, clubfoot) on the side opposite to the arch of scoliosis, with a high degree of probability, should be interpreted as a manifestation of FSM (Yamada S., 2001).
When assessing neurological examination data, it is noted that FMS most often occurs in the form of asymmetrical, uneven sensory and motor disturbances, accompanied by a decrease in tendon reflexes, as well as pelvic disorders of a mixed type (Yamada S., 2004). However, in some cases, gross trophic disorders may be detected, accompanied by a violation of the integrity of the skin - trophic ulcers (Nikolaev S.N., 1996; Brand N., 1996).
Disorders of the function of the pelvic organs are detected in 40% of patients with FMS, being its only clinical manifestation in 4% of cases (Prityko A.G., 1997; Metcalfe PD, 2006). The majority of patients with FMS show signs of bladder detrusor hypotension due to damage to the parasympathetic micturition center. Depending on the degree of preservation of urethral resistance, pelvic disorders in them occur in the form of constant or periodic urinary incontinence with the accumulation of varying volumes of residual urine, which in some cases requires catheterization of the bladder (Khachatryan V.A., 2009). Most often, such urodynamic disorders are accompanied by chronic constipation and stool loss due to decreased tone of the rectal sphincters (Kayaba H., 2003).
A decrease in the volume of filling of the bladder against the background of an increase in the tone of its muscles is observed less frequently and may be a consequence of damage to the spinal cord above the level of the conus. In this case, there is a disconnection of the structures of the segmental apparatus and supraspinal centers. Hyperexcitability of the detrusor, manifested clinically in the form of imperative, false urges, is caused by irritation of the bladder wall while maintaining a sufficient number of functioning neurons of the parasympathetic sacral center. Often, in children with FSM, against the background of urodynamic disorders signs of chronic urinary tract infection , vesicoureteral reflux and ureterohydronephrosis are revealed (Elikbaev G.M., 2008).
Thus, the clinical diagnosis of FSM is based on the identification of skin stigmas of dysembryogenesis, musculoskeletal deformities, weakness, sensory disturbances in the lower extremities, as well as pelvic disorders.
What is red bone marrow responsible for?
The main function performed by red bone marrow is the function of hematopoiesis or hematopoiesis. It is carried out constantly and extremely intensively - more than 300 million blood cells are formed in the hematopoietic organs per minute. The function of hematopoiesis is unique in that at the right time and in the right place a huge, but at the same time optimal, number of blood cells of the required type is produced. Bone marrow can speed up the production of any type of blood cell by 5-6 times if the body needs more of them. All blood cells develop from a single parent cell. It has the morphology of a small lymphocyte and is called a multipotent hematopoietic stem cell (HSC). Its descendants are all peripheral blood cells. During the process of division and differentiation of multipotent HSCs, all hematopoietic tissue is formed. It unites both precursor cells and maturing and mature blood cells: red blood cells, platelets and leukocytes, which make up human peripheral blood.
Hematopoiesis combines two large divisions of hematopoiesis: lymphopoiesis and myelopoiesis.
- Myelopoiesis (or myeloid hematopoiesis). Normally, the only place where this process occurs after birth is the red bone marrow. All the formed elements of blood are formed there, except lymphocytes (platelets, erythrocytes, monocytes and granulocytes), which then enter the peripheral blood.
- Lymphopoiesis (formation of T-lymphocytes and B-lymphocytes). After birth, it is realized in the central and peripheral lymphoid organs. The first includes red bone marrow, as well as the thymus (which retains the functions of a lymphoid organ only until the body reaches puberty); the second - lymph nodes, spleen and Peyer's patches of the gastrointestinal tract.
Erythrocytes, also called “red blood cells,” are cells that do not have a nucleus and are shaped like a biconcave disc. It is maintained in red blood cells by spectrin (a membrane stabilizing protein). The normal size of a red blood cell ranges between 7.5 microns and 8.3 microns, and the life expectancy is 90-120 days. The well-known main blood groups (I, II, III, IV) are distinguished based on the antigenic properties of red blood cells. The function of red blood cells is extremely important - they transport respiratory gases. The cytoplasm of an erythrocyte is filled with hemoglobin by 96%. This is a chromoprotein consisting of two parts: globin and heme. The first is protein, and the second is non-protein and is a complex of protoporphyrin IX and iron. Oxygen from the alveoli of the lungs is transported to the cells of the whole body precisely thanks to hemoglobin, and vice versa, from cells to the alveoli - with the help of carbon dioxide. Normally, each hemoglobin molecule contains two pairs of identical protein chains. They are designated by the letters α and β from the Greek alphabet. Depending on the composition of these chains, three types of hemoglobin are distinguished: embryonic, fetal and adult hemoglobin.
In addition to mature erythrocytes, young erythrocytes – reticulocytes – can be found in peripheral blood. These are cells without a nucleus, but contain a large amount of RNA and ribosomes, which have membrane receptors for transferrin. Reticulocyte RNA continues to produce hemoglobin. At this stage, it is possible to produce hemoglobin up to 30% of the total amount in the red blood cell. Most of it is synthesized at the pre-reticulocyte stages of cell differentiation - 70-80% of hemoglobin. When a reticulocyte develops into a mature red blood cell, it can no longer produce hemoglobin because it has lost RNA. In the bone marrow, the red blood cell remains at the reticulocyte stage for one day, and then for another day in the peripheral blood.
Leukocytes, in turn called white blood cells, are a heterogeneous group of peripheral blood cells that contain a nucleus. They perform the function of immunity and differ in several ways. By the shape of the nucleus - segmented or rounded, by the color and nature of the cytoplasm, as well as by granularity - its presence or absence.
If specific granularity is absent, the leukocytes are called agranulocytes, and if present, granulocytes. The first include lymphocytes and monocytes.
Granulocytes differ from each other in the nature of their specific granularity and come in three types:
- Neutrophils (contain abundant fine pale purple (“neutrophil”) granules).
- Basophils (with large and sparse dark purple (“basophilic”) granules).
- Eosinophils (distinguished by their granularity, occupying the entire cytoplasm of the cell).
Thanks to leukocytes, the body implements a protective function - immunity, which can be specific and nonspecific.
One of the manifestations of nonspecific immunity involves neutrophils, monocytes and tissue macrophages (monocytes turn into them after they leave the bloodstream). They phagocytose (capture) followed by lysis (dissolution) of microbes, toxins and cellular detritus (in other words, garbage). Eosinophils provide protection against parasites and are involved in allergic reactions (like basophils).
Lymphocytes carry out specific immune reactions, whether innate or acquired. Specific immunity, in turn, is humoral and cellular. Humoral immunity is realized due to the synthesis of immunoglobulins of classes A, M, G, E, D by B lymphocytes; and cellular - with the help of the diverse functions of T-lymphocytes. Acquired immunity can be formed naturally, as a result of various infectious diseases, or as a result of immunization of the body.
The sizes of leukocytes range from 6 microns (small lymphocytes) to 14 microns (monocytes).
Leukocytes differ from each other not only in appearance and function, but also in life expectancy. For example, the lifespan of lymphocytes varies between several hours and tens of years. Monocytes circulate in the blood for 72 hours and then enter the tissues, where they transform into fixed or migrating macrophages. Neutrophils remain in the blood for 4-10 hours, followed by release into the tissues.
Platelets are the third formed element of blood. They are equated to true cells, although they are not. In fact, these are particles of the shed cytoplasm of bone marrow megakaryocytes, the so-called blood platelets. Platelets are characterized by the properties of aggregation (gluing) and adhesion (sticking). Their participation in the mechanisms of blood coagulation and fibrinolysis is determined by the presence of special biologically active substances. They also help maintain normal microvascular resistance and function (angiotrophic function). The platelet size is 1-2 microns, and the life expectancy is 8 days.
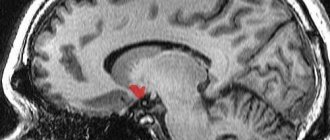
Instrumental diagnostics
Currently, MRI has almost completely replaced SCT myelography from the diagnosis of FMS, leaving ultrasound as a useful diagnostic method in newborns. Along with this, it is believed that the selection of candidates even for this non-invasive study should be based on a thorough clinical examination.
Previously, it was believed that all children with FSM have spina bifida (Boone D., 1985), but modern studies show that FSM also occurs in the absence of spina bifida (Ackerman LL, 2003). Thus, despite the fact that the occurrence of spina bifida occulta in the population is about 22%, only a small part of them have FSM (Nejat F., 2008).
It is known that during the period of intrauterine development, the growth of the spinal column outstrips the increase in the length of the spinal cord, forming a difference in length and a higher end of the spinal cord. The difference in their length increases most actively from the 12th to the 20th week of gestation, slowing down subsequently (Zalel Y., 2006).
It was previously believed that in newborns the spinal cord ends at the level of the L2-L3 vertebral disc, and then migrates cranially and reaches the level of the L1-L2 vertebrae by two months (Barson AJ, 1970). Subsequent studies showed that in most cases it ends at the level of the L2 vertebrae at birth (Wolf S., 1992; Robbin ML, 1994; Hill CA, 1995).
The level of the end of the spinal cord can normally vary from the middle of Th12 to the middle of the L3 vertebra, but in 94-98% of cases it is above the level of the L2-L3 vertebral disc (Reimann AF, 1944). Taking these data into account, the idea was formed that when the conus of the spinal cord is located below the level of the L2 vertebra, we can talk about radiological signs of SFSM. However, a low position of the conus spinal cord can be observed in some healthy newborns (Hughes JA, 2003; Thakur NH, 2011), and FSM can develop even with a normal position of the conus spinal cord (Warder DE, 1993).
Low location of the conus of the spinal cord in various forms of spinal dysraphism
End thread
Normally, the spinal cord ends in a filum terminale, which is a fibrovascular cord of parallel collagen bundles connected by a transverse network of collagen and elastin fibers and capillaries located between them (Fontes et al 2006). The diameter of the terminal filament normally ranges from 1.1 to 1.2 mm (Yundt KD, 1997). When its thickness is more than 2 mm, it was proposed to consider the diagnosis of FSM justified.
The filum terminale of the spinal cord is normal (left) and pathological (right)
However, thickening of the filum terminale, as it turned out later, is not a prerequisite for the development of FSM (Pinto FC, 2002), and its clinical manifestations can develop with a smaller diameter of the filum terminale (Nkhazar GB, 1995; Selden NR, 2006). Also, fatty infiltration of the filum terminale, which is normally detected in 5.8% of subjects (McLendon RE, 1988), is not a mandatory sign of the presence of FSM.
When fixing the spinal cord, the filum terminale is most often located behind the roots of the cauda equina, and the spinal cord is deviated posteriorly and adjacent to the arachnoid membrane (Fitz CR, 1975).
The tensioned final thread (indicated by the arrow) fits tightly from the inside to the thinned dura mater
As methods of additional differential diagnosis, MRI in the prone position, as well as standing with the torso flexed and extended (functional MRI), was proposed, but so far they have not become widespread (Levy LM, 1988; Zamani AA, 1998; Witkamp T.D., 2001; Niggemann P., 2011; Singh S., 2012).
In the prone position (image on the right), the dorsal deviation of the conus and filum terminale of the spinal cord remains.
The experience of performing DWI tractography in patients with FSM allowed us to assume its role in terms of differential diagnosis of spinal cord structures and scar tissue, and also allowed us to put forward the assumption that, based on the indicators of fractional anisotropy, one can judge the degree of preservation of the spinal cord conductors and evaluate the prognosis of surgical treatment of FSM (Filippi CG, 2010).
DWI tractography of the spinal cord and cauda equina roots (right)
Thus, none of the previously proposed neuroimaging criteria for diagnosing FMS is currently absolute.
Data from electrophysiological examination methods are also not believed to be of decisive importance in the diagnosis of FMS (Yamada S., 2007). In particular, the study of somatosensory evoked potentials (SSEPs) and motor evoked potentials (MEPs) in children is often uninformative, and the traditionally considered electroneuromyogram (ENMG) patterns, despite the identified clinical picture of SPS, may be within normal limits (Gusev A.R., 1990) . It is reported that registration of SSEPs from the tibial nerves can be used as a screening method of examination, as well as to assess the long-term results of surgical treatment of SSEP in adults (Li V., 1996; Kale SS, 1998).
It should be noted that many authors point to the importance of urodynamic examination data in diagnosing FMS, including in cases of relapse of spinal cord fixation (Meyrat BJ, 2003; Metcalfe PD, 2006; Rendeli C., 2007; Maher CO, 2009).
Anatomical features
The spinal cord is located in the cavity of the spinal canal, which is formed by the processes of the vertebrae and their bodies. The beginning of the structure of the spinal cord is the foramen magnum of the brain. Next, the spinal cord is located in the canal, representing a 40-centimeter “cord” surrounded by three membranes.
The internal organ ends with a cluster of nerve fibers at the level of the first vertebrae in the lumbar region, called the cauda equina. This is where the narrowing begins, and then the internal organ is “stretched” into a terminal (terminal, terminal) filament, the diameter of which is 1 mm. The filum terminale extends to the coccygeal region, where it fuses with the periosteum.
The lower part of the trailing thread is tightly wrapped in ponytail fibers. When pain occurs in the coccyx area, doctors talk about a syndrome with the same name. The structure of the human spinal cord is such that the medulla itself is under constant protection - this is provided by the membranes and the spinal column itself.
The external structure is the shells and the space between them.
Surgery
The polyetiology of FSM, according to a number of experts, often leads to an unreasonable expansion of indications for its surgical treatment (Kulkarni AV, 2004). In this regard, the indications for surgery were proposed to be considered justified with a combination of characteristic radiological and clinical manifestations of FMS and the progressive course of the disease (Drake JM, 2007; Wykes V., 2012). Along with this, most researchers note the predominantly reversible nature of the changes during early correction of SFM (Yamada S., 2007) and the rare improvement in condition after surgery in patients with long-term symptoms (McLone D., 1997; Iskandar BJ, 1998; Haro H., 2004; Hajnovic L., 2007). It should also be noted that in patients considered “asymptomatic”, signs of the development of FMS may include undiagnosed changes in gait, scoliosis, as well as urodynamic disorders that occur under the guise of a chronic urinary tract infection (Sanchez T., 2014).
Previously considered appropriate expectant management was apparently due to the risk of general anesthesia, as well as the conditions of manipulation on the relatively small and seemingly more vulnerable structures of the spinal cord in children. The development of anesthesia, microsurgical equipment and intraoperative neurophysiological monitoring, of course, made it possible to successfully perform surgical interventions at any age immediately after introscopic verification of pathology, even with an asymptomatic course of the disease (Hoffman HJ, 1985; Tamaki N., 1988; Kanev PN, 1990; Koyanagi I., 1997; Schoenmakers MA, 2003; George TM, 2005; Rinaldi F., 2005). Thus, at present, an idea has formed about the advisability of early preventive surgical treatment of FSM, aimed at preventing possible irreversible damage to the spinal cord. It seems especially relevant to eliminate fixation in adolescents before the onset of a period of accelerated growth.
Surgical treatment of FSM consists of eliminating caudally located fixation factors, in particular: pathologically altered filament terminalis (fatty degeneration, thickening, shortening, decreased elasticity), pathological formations of the spinal canal (lipoma, dermoid, dermal sinus, bone, fibrous, septum), and also cicatricial and arachnoid adhesions (Caldarelli M., 2013):
Transplantation of a pathologically altered filament terminale
Removal of conus lipoma
Dermoid cyst removal
Elimination of diastematomyelia
Preference is given to “organ-saving” techniques - laminotomy, microsurgical techniques. As additional options, a number of authors report the effectiveness of using a CO2 laser and an ultrasound aspirator for tissue dissection, indicating minimal energy dispersion and minor traumatic effects of laser and ultrasound compared to traditional methods (McLone DG, 1986; Browd SR, 2009), as well as the feasibility of intraoperative neurophysiological monitoring (Sala F., 2002).
Operating room view Operating microscope
The first stage is the isolation of PRP and BMAC
To obtain PRP, 60 ml of peripheral blood is taken from patients, 10 ml of the anticoagulant citrate dextrose is added and the resulting mixture is centrifuged, followed by concentration. This results in an average of 7–8 ml of platelet-rich plasma.
BMAC is obtained using a biopsy needle, which is inserted through the skin and subcutaneous tissue into the right iliac crest. Using slow aspiration, 2 syringes of 25 ml each are taken, to which 1000 units/ml of heparin are added. The resulting mixture is filtered and centrifuged for 10 minutes, resulting in 17 ml of BMAC.
After selection, PRP and BMAC are mixed in a 1:2 ratio. The last stage of this method is the administration of the resulting drug to the patient.
Seven people with various spinal cord injuries took part in the experiment; the average age of the patients was 43.7 ± 2.33 years. After injury, patients underwent at least two interventions (physical therapy and surgery) and were treated with a mixture of PRP and BMAC between 2.4 months and 6.2 years after injury.
ODI scores were tracked using a questionnaire based on the following categories: pain intensity, self-care, lifting, walking, sitting and standing, sleep, sex life, social life, and travel. Patients were asked to rate their condition from 0 (no discomfort due to injury) to 5 (maximum discomfort) in each category. All scores were added and divided by 50 to obtain the percentage of functional disability.
6 of 7 patients had significant functional disability at the start of the experiment. One patient stopped observing after the procedure, and the dynamics of the remaining five were depicted in the study. Two patients experienced changes from “severe disability” to “minimal disability” and regained the ability to perform all household activities independently. The third patient's performance improved by 40% over a year, and the fourth improved by 28% over two months of follow-up.
Side effects were observed in one out of seven patients. He could not receive the drug intravenously. The patient reported headaches and memory difficulties.
This treatment method helps to avoid additional trauma that occurs when injections are given into the affected area of the spinal cord. It is safe and effective for injury recovery. Patients experience positive dynamics and minimal side effects. The potential of such treatment is great, and it claims to occupy a leading position in the fight against spinal cord injuries.
Intraoperative neurophysiological monitoring
Due to the fact that the incidence of neurological loss during surgical treatment of FSM is on average 10.9% (Choux M., 1994), various methods of intraoperative neurophysiological monitoring aimed at identifying and assessing the function of excitable conductive structures ( roots) of the spinal cord . For this purpose, we combined registration of somatosensory, motor evoked potentials, bulbocavernosus reflex, as well as electromyography (free-run EMG) and stimulation electroneuromyography (DNS) from the muscles of the lower extremities and the external sphincter of the rectum. According to the literature, monitoring of evoked motor potentials in combination with stimulation electroneuromyography demonstrated the greatest information content (Paradiso G., 2006).
Multimodal intraoperative neurophysiological monitoring
Features of neurophysiological monitoring in children with FMS are due to impaired formation and immaturity of the spinal cord, as well as its stretching, deformation and ischemia. Against this background, registration of evoked potentials and the bulbocavity reflex is extremely difficult (Rodi Z., 2001), and the main method of neuromonitoring remains stimulation electroneuromyography, with the goal of electrical stimulation mapping of the spinal cord roots (ESC) (Deletis V., 1992).
Electrical stimulation mapping of the spinal cord roots
Despite the known threshold current values for the anterior and dorsal roots of the spinal cord, their values for functionally significant structures in conditions of spinal cord malformations have not yet been established. Analogies with the results of studies in which, when stimulating the filum terminale, the voltage required for a muscle response exceeded that when stimulating the motor root by 100 times (von Koch CS, 2002), it was not possible to draw, since when the root is involved in a mass of adipose tissue or scar the magnitude of the threshold irritation can increase significantly. This is believed to be due to excitation dissipation or partial loss of conductive properties by the spine.
Literature
- Mescher AL Junqueira's Basic Histology text and atlas. McGraw-Hill Education / Medical, 2021. - 576 p.;
- Sean J. Morrison, David T. Scadden. (2014). The bone marrow niche for haematopoietic stem cells. Nature
.
505 , 327-334; - Bykov V.L. Cytology and general histology. Functional morphology of human cells and tissues. St. Petersburg: Sotis, 2002;
- Shumakov V.I., Kazakov E.N., Onishchenko N.A., Gureev S.V., Ostroumov E.N., Chestukhin V.V. et al. (2003). The first experience of clinical use of autologous bone marrow mesenchymal stem cells to restore myocardial contractile function. "Russian Cardiology Journal". 5, 42–50;
- What does my bone marrow do? (2016). Myelodysplastic Syndromes Foundation;
- Gedro N.N. (2013). Modern bone marrow transplantation department. "Nurse". 2, 7–9;
- Subbotina N.N., Dolgopolov I.S., Popa A.V., Boyarshinov V.K., Pimenov R.I., Mentkevich G.L. (2014). Haploidentical hematopoietic stem cell transplantation in children with acute myeloid leukemia: evolution of the method and our own data. "Clinical oncohematology". 2, 131–136;
- OV Paina, NV Stancheva, Ye. V. Semenova, S.N. Bondarenko, O.A. Slesarchuk, et. al.. (2015). Haploidentical hematopoietic stem cell transplantation in the treatment of children and adolescents with resistant forms of acute leukemia. Ross.
ž. det. hematol. onkol. .
2 , 39-45; - EG Khamaganova, LA Kuzmina. (2019). ASSESSMENT OF HLA-COMPATIBILITY AND REQUIREMENTS FOR HLA-TYPING OF PATIENT AND DONOR IN ALLOGENEIC HEMATOPOIETIC STEM CELL TRANSPLANTATION. Gematologiâ i transfuziologiâ
.
64 , 175-187.
Latent tethered spinal cord syndrome
One of the pressing problems of pediatric neurosurgery is the choice of optimal treatment tactics for latent tethered spinal cord syndrome, in which, despite the characteristic clinical picture of FMS, there are no such criteria as low location of the spinal cord conus (below the level of the L2 vertebral body), as well as thickening ( more than 2mm in diameter) and/or shortening of the terminal thread
Patient with hidden SFM, conus spinal cord at the L1 vertebral level
Considering that the observational groups of latent FSM described in the literature are relatively small, to date there has been no consensus regarding the optimal treatment tactics for this pathology. Most experts point to the advisability of excision of the terminal filament and provide data on the high effectiveness of this manipulation, while a number of authors, on the contrary, express doubts about the existence of sufficient indications for surgical intervention. Their skepticism is based, among other things, on the fact that urinary disorders in children, which is considered the most characteristic sign of latent FMS, are associated with stretching of the conus of the spinal cord in no more than 1.5% of cases, and its true causes are other pathologies.
When the torso is flexed, the height of the spinal canal increases by more than 7%. In this case, damping of the longitudinal tension transmitted to the spinal cord is ensured due to the elastic properties of the final thread, caused by a balanced combination of elastin, collagen and reticular fibers. One of the possible reasons for the development of latent FSM is considered to be invasion of adipose tissue, sclerosis and dystrophic changes, as a result of which the elasticity of the terminal filament decreases. With insufficient compensation for stretching, it is transmitted to the caudal parts of the spinal cord, and with a further increase in vertebromedullary disproportion, it spreads to the higher segments of the spinal cord. The formation of a detailed clinical picture of FMS can take a long period of time and be remitting in nature against the background of periods of slowed growth and reflex limitation of motor activity, while some of the formed motor, sensory or orthopedic deficits may be irreversible. It is obvious that early diagnosis and timely correction of latent FSM has a significant impact on the prognosis of the disease. In the case of a combination of pelvic disorders and/or pain syndrome that are resistant to drug therapy, as well as in the presence of characteristic neurological and orthopedic disorders in children with spina bifida occulta, in our opinion, there are indications for excision of the filum terminale, even with a normal location of the caudal parts of the spinal cord.
Electrostimulation identification and intersection of the tense terminal filament with hidden SFSM
What is yellow bone marrow responsible for?
Yellow bone marrow is usually found in the diaphysis of long bones. It consists of reticular tissue and adipocyte cells, which contain a special lipochrome pigment in the center of the cavity of long bones, and on the outside it is surrounded by a layer of red bone marrow. Fat from adipocytes, in case of emergency, for example, after prolonged fasting, the body can use as an energy source. Under normal conditions, yellow bone marrow is not involved in hematopoiesis, but in exceptional cases, for example, after severe blood loss or acute anemia, part of the yellow bone marrow can turn red to speed up blood recovery.
Results and forecast
It is believed that surgical treatment of FSM allows to achieve improvement or stabilization of the condition of 70-80% of patients (Herman JM, 1993; Sarwark JF, 1996; Koyanagi I., 1997; Sharif S., 1997; Lee GY, 2006; Lad SP, 2007; Bowman RM, 2009; Ostling LR, 2012). According to various data, pain syndrome regresses in most cases (Maher CO, 2007; Bowman RM, 2009; Romagna A., 2013), while improvement in motor function is observed in no more than 80% of patients. According to JM Herman et al., within a period of up to 4 years after surgery, the condition of 93% of children operated on for MMC and 100% of children operated on for spinal lipomas improved or stabilized (Herman JM, 1993).
Short-term and long-term results of surgical treatment of children with FMS at the Pediatric Neurosurgery Clinic of the Russian Scientific Research Institute named after. prof. A.L. Polenova
A decrease in spinal deformity as a result of correction of the spinal spinal cord is observed in 20-50% of cases, and its stabilization in 10-20% (Herman JM, 1993; Bowman RM, 2001). At the same time, it has been noted that when the Cobb angle of deformation is more than 40°, eliminating fixation, as a rule, does not lead to improvement (Pierz K., 2000; McGirt MJ, 2009). There are also descriptions of observations in which scoliosis progresses in patients with MMC at the level of the thoracic spine, despite the elimination of fixation (Reigel DH, 1994).
Regarding the function of the pelvic organs, the authors’ data differ significantly. Their improvement is reported (in 30-60% of cases), including after repeated interventions (Herman JM, 1993; Bowman RM, 2001; Metcalfe PD, 2006; Tarcan T., 2006; Abrahamsson, K., 2007; Maher CO, 2009), and about the absence of changes compared to the preoperative level (Fone PD, 1997). Improvement in capacitance characteristics is most expected in patients with urodynamic disorders such as an “overactive” bladder (Khoury AE, 1990; Nogueira M., 2004; Guerra LA, 2006).
The development or increase in neurological deficit after surgery has been established, according to various sources, in 9.5-35% of cases, more often with repeated interventions (Herman JM, 1993; Albright AL, 1999; Wang B., 2002). We are mainly talking about urological complications (2.2%) (Lad SP, 2007). O are less common than other undesirable consequences of surgery (cerebrospinal fluid leak, meningitis, etc.) (Cochrane DD, 1998; Al-Holou WN, 2009; Bowman RM, 2009;) and are most expected during repeated interventions (Maher CO, 2007). The development of postoperative wound complications is most expected in patients operated on for myelomeningocele, which is apparently due to impaired soft tissue trophism and unsatisfactory wound consolidation. The likelihood of meningitis increases significantly with the formation of a cerebrospinal fluid fistula. When detecting liquorrhea in these patients, hydrocephalus or shunt dysfunction should first be excluded (Rostotskaya V.I., 1962; Orlov Yu.A., 1993; Khachatryan V.A., 1995; Hudgins RJ, 2004). Other complications include failure of the sutures and dehiscence of the surgical wound, which occur in 7-10% of cases (Bowman RM, 2009).
Treatment of radicular syndrome
In cases where radicular syndrome is caused by degenerative-dystrophic diseases of the spine, conservative therapy is used predominantly. In case of intense pain syndrome, rest, analgesic therapy (diclofenac, meloxicam, ibuprofen, ketorolac, lidocaine-hydrocortisone paravertebral blockades), relief of muscular-tonic syndrome (methyllycaconitine, tolperisone, baclofen, diazepam), decongestant treatment (furosemide, ethacrynic acid), neurometabolic products (vitamins B). In order to improve blood circulation and venous outflow, aminophylline, xanthinol nicotinate, pentoxifylline, troxerutin, and horse chestnut extract are prescribed. According to indications, chondroprotectors (cartilage and calf brain extract with vitamin C, chondroitin sulfate), absorbable treatment (hyaluronidase), and drugs to facilitate neuronal transmission (neostigmine) are additionally used.
Long-term radicular syndrome with chronic pain is an indication for the use of antidepressants (duloxetine, amitriptyline, desipramine), and when pain is combined with neurotrophic disorders, for the use of ganglion blockers (benzohexonium, ganglefen). For muscular atrophy, nandrolone decanoate with vitamin E is used. A good effect (in the absence of contraindications) is provided by traction therapy, which increases intervertebral distances and thereby reduces the negative impact on the spinal root. In the acute period, reflexology, UHF, and hydrocortisone ultraphonophoresis can be an additional means of pain relief. In the early stages they begin to use exercise therapy, during the rehabilitation period - massage, paraffin therapy, ozokerite therapy, therapeutic sulfide and radon baths, mud therapy.
The question of surgical treatment arises when conservative therapy is ineffective, prolapse symptoms progress, or the presence of a spinal tumor. The operation is performed by a neurosurgeon and aims to eliminate compression of the root, as well as remove its cause. For herniated intervertebral discs, discectomy or microdiscectomy is possible; for tumors, their removal is possible. If the cause of radicular syndrome is instability, then spinal fixation is performed.
Repeated (recurrent, scar) fixation of the spinal cord
Clinical manifestations of FSM, detected after surgery aimed at eliminating spinal cord fixation, are associated with its re-fixation (Inoue HK, 1994; Colak A., 1998; Ohe N., 2000; Blount JP, 2007; Al-Holou WN, 2009; Yong R.L., 2011; Caldarelli M., 2013). According to the literature, the clinical and neuroimaging (MRI) picture of relapse of spinal cord fixation can develop in 5-50% of operated patients, while reoperation may be required in 30% of them (Herman JM, 1993; Filler AG, 1995; Archibeck MJ, 1997 ; Kang JK, 2003; Morimoto K., 2005; Ogiwara H., 2011).
The main reason for the development of re-fixation is considered to be a local violation of the circulation of cerebrospinal fluid (Kang JK, 2003). This is indirectly confirmed by the high frequency of relapse of fixation after repair of spina bifida and lipomyelocele and relatively low for other anomalies (Caldarelli M., 2013). Apparently, the size and shape of the spinal cord (neural placode), the residual volume of tumor (fatty) tissue, as well as the narrowing of the spinal canal in the anteroposterior direction do not always allow restoration of the spinal cord membranes with the formation of a sufficient volume of subarachnoid spaces for adequate circulation of cerebrospinal fluid in the terminal cistern (Hudgins RJ, 2004), as a result of which the spinal cord fuses with the membranes, and sometimes with scarred soft tissues, spreading beyond the dural sac and even the spinal canal (Caldarelli M., 1995).
Relapse of spinal cord tethering is the second most common cause of deterioration in the condition of patients with myelomeningocele , with a progressive deterioration of 60% of them observed during a follow-up period of up to 5 years (Phuong LK, 2002; Talamonti G., 2007). It is noted that with incomplete elimination of fixation, the relapse rate can reach 80% (Huttmann S., 2001), while in 10% of cases three or more operations may be required to stabilize the condition of patients (Al-Holou WN, 2009; Maher CO, 2007, 2009). According to research results, an increase in the detection of relapse of FSM occurs at ages from 2 to 4 and from 8 to 11 years, regardless of the primary pathology (Herman JM, 1993; Caldarelli M., 1995).
Considering that surgical intervention at the initial stages of the pathological process, according to various authors, leads to improved treatment results, it was proposed to consider a progressive deterioration in the child’s condition or the appearance of new symptoms as indications for surgery . (Bowman RM, 2001; George TM, 2005). Along with this, making a decision about surgical treatment is extremely difficult in chronically “symptomatic” patients with persistent neurological deficits. At the same time, emphasis is placed on the need to exclude other causes of deterioration of the patient’s condition, such as shunt dysfunction, Chiari malformation, syringomyelia, etc. (Bowman RM, 2001; Talamonti G., 2007). It is emphasized that relapse of FMS can occur with erased, slowly progressing symptoms, which also complicates the recognition of the pathological process and is the reason for its late diagnosis . It is reported that the most common clinical manifestation in older age is progressive spinal deformity (Carstens C., 1996). However, other signs are fair to consider contractures of the lower extremities, deterioration of gait, and back pain (Herman JM, 1993; Bowman RM, 2009). Thus, the clinical picture of recurrent FSM is in many ways similar to that of primary FSM. At the same time, the onset of the disease is often associated with pain, and the deterioration of the condition with progressive spinal deformation (Caldarelli M., 1995).
Surgical treatment for re-fixation of the spinal cord is aimed at eliminating tension and deformation of the spinal cord and roots, as well as restoring cerebrospinal fluid circulation in the fixation area.
Elimination of scar fixation of the spinal cord
The area of scar adhesions during re-fixation may depend on the method of wound closure during primary intervention (Caldarelli M., 2013). In cases where neural tube reconstruction was performed during the primary operation, the scar is usually located in the midplane over a limited area (Caldarelli M., 2013).
Thus, the main measure to prevent re-fixation of the spinal cord during surgical correction of MMC and spinal lipomas is considered to be reconstruction of the neural placode (Pang D., 2010; Talamonti G., 2007). Expanding plastic surgery of the dura mater with various artificial substitutes is also used (Inoue HK, 1994; Ohe N., 2000). In addition, after surgery, bed rest in a prone position is recommended in order to avoid gravitational contact of the spinal cord with the dura mater.
Spine and spinal cord injury
Although methods for diagnosing and providing assistance for injuries of the spine and spinal cord were given in the Egyptian papyri and the works of Hippocrates, for a long time a spinal injury with neurological disorders was considered practically a death sentence. Back in the First World War, 80% of those wounded in the spine died within the first 2 weeks. Progress in the treatment of spinal cord injury (SCI), based on an improved understanding of its pathogenesis and the development of radically new treatment methods, began only during the Second World War and in the post-war years. Today, SCI remains a severe, but usually not fatal, type of injury, and a significant contribution to minimizing its consequences is made by the timely and adequate provision of first, qualified and specialized medical care to victims.
Traumatic injuries of the spine and spinal cord are much less common than TBI. In adults, the incidence of SMT is 5 per 100 thousand population per year, in children it is even lower (less than 1 per 100 thousand population per year), but in children SMT is more often associated with polytrauma and is more severe, with a worse prognosis. In Russia, approximately 80% of victims are men under 30 years of age. Since today the majority of victims, even with severe STS, survive, the number of people with consequences of STS in the population of developed countries is approximately 90 per 100 thousand population (for Russia today this is approximately 130 thousand people, of which 13 thousand are with paraplegia or tetraplegia) . The social significance of the problem is difficult to overestimate.
The main cause of SMT is road traffic accidents (50% of cases). This is followed by sports injuries and those associated with active recreation (25%, of which 2/3 are injuries to the cervical spine and spinal cord received while diving in a shallow place). Approximately 10% each are industrial injuries and those received as a result of illegal actions, and 5% are received from a fall from a height, in natural disasters, etc.
Most often the cervical spine is damaged (55%), less often - the thoracic (30%), even less often - the lumbosacral (15%).
Damage to the spinal cord and its roots occurs in approximately 20% of cases of SCI. Such injuries are called complicated.
The level of damage (damage) to the spinal cord is assessed by the lower segment, in the dermatome of which sensitivity and at least minimal voluntary movements are preserved. Often, but not always, this level corresponds to the established level of spinal injury. In assessing the level of spinal cord damage, one should not rely on pathological reflexes (Babinsky, Rossolimo, Oppenheim, defensive and synkinesis); their reflex arc may pass below the level of complete spinal cord damage.
There are complete and incomplete spinal cord injuries. With complete damage (group A on the Frankel scale), there is no sensitivity and voluntary movements below the level of the lesion. Usually in such a situation the spinal cord is anatomically destroyed. With incomplete damage (groups B, C, D on the Frankel scale), disturbances in sensitivity and movement are expressed to a greater or lesser extent; group E corresponds to the norm.
Injuries to the spine and spinal cord are divided into open, in which the integrity of the skin and underlying soft tissues is damaged, and closed, in which these injuries are absent. In peacetime, closed MMT prevails.
Table Spinal Cord Disability Rating Scale (Frankel)
Closed injuries of the spine and spinal cord
| Complete defeat | A | No voluntary movement or sensation below the level of the lesion |
| Only sensitivity is preserved | B | Below the level of the lesion there are no voluntary movements, sensitivity is preserved |
| Movements intact but non-functional | C | Below the level of the lesion there are voluntary movements, but without useful function. Sensitivity may or may not be preserved. |
| Movements are intact and functional | D | Useful voluntary movements below the level of the lesion are functional. Various sensitivity disorders |
| Normal motor function | E | Movements and sensitivity below the level of the lesion are preserved, pathological reflexes are possible |
Spinal injuries. Closed spinal injuries occur under the influence of excessive flexion, extension, rotation and axial compression. In many cases, a combination of these mechanisms is observed (for example, with the so-called whiplash injury of the cervical spine, when flexion of the spine is followed by its extension).
As a result of the influence of these mechanical forces, various changes in the spine are possible:
• sprain and rupture of ligaments;
• damage to intervertebral discs;
• subluxations and dislocations of the vertebrae;
• vertebral fractures;
• fracture-dislocations.
The following types of vertebral fractures are distinguished:
• fractures of vertebral bodies (compression, splintered, explosive);
• fractures of the posterior half ring;
• combined with simultaneous fracture of the bodies, arches, articular and transverse processes;
• isolated fractures of the transverse and spinous processes.
It is of fundamental importance to classify a spinal injury as stable or unstable. The stability of the spine is understood as the ability of its structures to limit their mutual displacement so that, under physiological loads, it does not lead to damage or irritation of the spinal cord and its roots. Unstable spinal injuries are usually associated with rupture of ligaments, fibrous ring, multiple destruction of bone structures and are fraught with additional trauma to the spinal cord even with minor movements in the affected segment.
It is easier to understand the causes of spinal instability if we turn to Denis’s concept, which identifies 3 support systems (columns) of the spine: the anterior support complex (column) includes the anterior longitudinal ligament and the anterior segment of the vertebral body; the middle column unites the posterior longitudinal ligament and the posterior segment of the vertebral body; posterior column - articular processes, arches with yellow ligaments and spinous processes with their ligamentous apparatus. Violation of the integrity of two of the mentioned supporting complexes (pillars), as a rule, leads to instability of the spine.
Spinal cord injuries. Denis’s diagram: the anterior, middle and posterior supporting complexes (pillars) of the spine are highlighted; instability of the spinal segment develops when two of them are affected in any combination
Based on the type of spinal cord injury, it can be classified as concussion, contusion, compression, and violation of anatomical integrity (partial or complete rupture of the spinal cord); often these mechanisms are combined (for example, a bruise with vascular rupture and hemorrhage - hematomyelia, causing direct damage to the axons and cells of the spinal cord). The most severe form of local damage to the spinal cord is its complete anatomical break with diastasis of the ends at the site of damage.
The degree of damage to the spinal cord and its roots is of primary importance for the fate of the patient. This damage can occur both at the time of injury (which is incurable) and in the subsequent period, when prevention of secondary spinal cord injuries is potentially possible.
Currently, there are no methods to restore the function of anatomically damaged neurons and cells of the spinal cord. The goal of treating STS is to minimize secondary damage to the spinal cord and provide optimal conditions for the restoration of neurons and axons caught in the zone of impaired blood supply—the “ischemic penumbra.”
A frequent and dangerous consequence of spinal cord injury is edema, caused both by an increase in tissue osmotic pressure during the destruction of cell membranes, and by disturbances in venous outflow due to compression of the spinal veins (hematomas, bone fragments, etc.) and their thrombosis. An increase in the volume of the spinal cord as a result of edema leads to an increase in local hypertension and a decrease in perfusion pressure, which, according to the principle of a vicious circle, leads to a further increase in edema, ischemia and can lead to irreversible damage to the entire diameter of the spinal cord.
Clinical picture of spinal injury. In addition to the listed morphological changes, functional disorders caused by disturbances at the cellular level are also possible. Such spinal cord dysfunctions regress, as a rule, within the first 24 hours after injury.
The main manifestation of a spinal fracture is local pain, which increases significantly with exertion (standing up, bending and even turning in bed). Spinal damage may also be indicated by:
• abrasions and hematomas;
• swelling and local tenderness of soft tissues in the paravertebral region;
• pain on palpation of the spinous processes;
• different distances between the apices of the spinous processes, displacement of one or more of them anteriorly, posteriorly or to the side from the midline;
• angular change in the spinal axis (traumatic scoliosis, kyphosis or lordosis).
With a fracture of the lower thoracic and lumbar spine, even without damage to the spinal cord, intestinal paresis may develop due to a retroperitoneal hematoma (compressing the vessels and nerves of the mesentery).
Clinical picture of spinal cord damage in spinal injury
The clinical symptoms of a complicated spinal fracture are determined by a number of reasons, primarily the level and degree of damage to the spinal cord.
There are syndromes of complete and partial transverse spinal cord lesions.
With the syndrome of complete transverse lesion of the spinal cord down from the level of the lesion, all voluntary movements are absent, flaccid paralysis is observed, deep and cutaneous reflexes are not evoked, all types of sensitivity are absent, control over the functions of the pelvic organs is lost (involuntary urination, defecation disorders, priapism); autonomic innervation suffers (sweating and temperature regulation are impaired). Over time, flaccid muscle paralysis can be replaced by spasticity, hyperreflexia, and automatisms in the functions of the pelvic organs are often formed.
Damage to the cervical enlargement of the spinal cord (CV-ThI at the level of the V-VII cervical vertebrae) leads to peripheral paraparesis of the upper extremities and spastic paraplegia of the lower extremities. Conduction disorders of all types of sensitivity occur below the level of the lesion. There may be radicular pain in the arms. Damage to the ciliospinal center causes the appearance of Horner's symptom, decreased blood pressure, and slowed pulse. Features of the clinical manifestations of spinal cord injury depend on the level of damage. If the upper cervical part of the spinal cord is damaged (CI-IV at the level of the I-IV cervical vertebrae), tetraparesis or spastic tetraplegia develops with the loss of all types of sensitivity from the corresponding level. If there is concomitant damage to the brain stem, bulbar disorders appear (dysphagia, aphonia, respiratory and cardiovascular disorders).
Injury to the thoracic part of the spinal cord (ThII-XII at the level of the I-IX thoracic vertebrae) leads to lower spastic paraplegia with the absence of all types of sensitivity, loss of abdominal reflexes: upper (ThVII-VIII), middle (ThIX-X) and lower (ThXI- XII).
If the lumbar enlargement is damaged (LI SII at the level of the X-XII thoracic and I lumbar vertebrae), peripheral paralysis of the lower extremities occurs, anesthesia of the perineum and legs downward from the inguinal (pupart) ligament occurs, and the cremasteric reflex falls out.
In case of injury to the conus of the spinal cord (SIII-V at the level of the I-II lumbar vertebrae), there is a “saddle-shaped” anesthesia in the perineal area.
Damage to the cauda equina is characterized by peripheral paralysis of the lower extremities, anesthesia of all types in the perineum and legs, and sharp radicular pain in them.
When the conus of the spinal cord and the roots of the cauda equina are damaged, the segmental apparatus of the spinal cord suffers and the syndrome of “hyporeflex neurogenic bladder” develops: characterized by urinary retention with paradoxical phenomena. Damage to the spinal cord at all levels is accompanied by disorders of urination, defecation and sexual function. With transverse damage to the spinal cord in the cervical and thoracic parts, dysfunction of the pelvic organs appears, such as the “hyper-reflex neurogenic bladder” syndrome. At first after the injury, urinary retention occurs, which can last for a very long time (months). The sensitivity of the bladder is lost. Then, as the segmental apparatus of the spinal cord disinhibits, urinary retention is replaced by spinal automaticity of urination. In this case, involuntary urination occurs when there is a slight accumulation of urine in the bladder.
noic ischuria - the bladder is full, but when the pressure in it begins to exceed the resistance of the sphincters, part of the urine flows out passively, which creates the illusion of intact urinary function.
Defecation disorders in the form of stool retention or fecal incontinence usually develop in parallel with urination disorders.
Damage to the spinal cord in any part is accompanied by pressure sores that occur in areas with impaired innervation, where bony protrusions are located under the soft tissues (sacrum, iliac crests, heels). Bedsores develop especially early and quickly with severe (transverse) damage to the spinal cord at the level of the cervical and thoracic regions. Bedsores quickly become infected and cause the development of sepsis.
When determining the level of spinal cord damage, the relative position of the vertebrae and spinal segments must be taken into account. It is easier to compare the location of the spinal cord segments with the spinous processes of the vertebrae (with the exception of the lower thoracic region). To determine the segment, add 2 to the vertebral number (so, at the level of the spinous process of the third thoracic vertebra the fifth thoracic segment will be located).
There are several syndromes of partial damage to the spinal cord. This pattern disappears in the lower thoracic and upper lumbar regions, where at the level of ThXI-XII and LI there are 11 segments of the spinal cord (5 lumbar, 5 sacral and 1 coccygeal).
Half-lesion syndrome of the spinal cord (Brown-Sequard syndrome) is paralysis of the limbs and impairment of deep types of sensitivity on the affected side with loss of pain and temperature sensitivity on the opposite side. It should be emphasized that this syndrome in its “pure” form is rare; its individual elements are usually identified.
Anterior spinal syndrome - bilateral paraplegia (or paraparesis) combined with decreased pain and temperature sensitivity. The reason for the development of this syndrome is a violation of blood flow in the anterior spinal artery, which is injured by a bone fragment or a prolapsed disc.
Central spinal cord syndrome (more often occurs with a sharp hyperextension of the spine) is characterized mainly by paresis of the arms, weakness in the legs is less pronounced; Sensory disturbances of varying severity below the level of the lesion and urinary retention are observed.
In some cases, mainly with trauma accompanied by sharp flexion of the spine, a syndrome of damage to the posterior cords of the spinal cord may develop - loss of deep types of sensitivity.
Damage to the spinal cord (especially when its diameter is completely damaged) is characterized by disturbances in the regulation of the functions of various internal organs: respiratory disorders with cervical damage, intestinal paresis, dysfunction of the pelvic organs, trophic disorders with the rapid development of bedsores.
In the acute stage of injury, the development of “spinal shock” is possible - a decrease in blood pressure (usually not lower than 80 mm Hg) in the absence of signs of polytrauma and internal or external bleeding. The pathogenesis of spinal shock is explained by the loss of sympathetic innervation below the site of injury while maintaining parasympathetic innervation (causes bradycardia) and atony of skeletal muscles below the level of injury (causes deposition of blood in the venous bed with a decrease in circulating blood volume).
Spinal cord concussions are very rare. It is characterized by damage to the spinal cord of a functional type in the absence of obvious structural damage. More often, paresthesia and sensory disturbances below the injury zone are observed, less often - paresis and paralysis, and dysfunction of the pelvic organs. Occasionally, clinical manifestations are severe, up to the picture of complete damage to the spinal cord; The differential diagnostic criterion is complete regression of symptoms within 24 hours. Clinical forms of spinal cord injury
The cerebrospinal fluid is not changed during a concussion of the spinal cord, the patency of the subarachnoid space is not impaired. Changes in the spinal cord are not detected by MRI.
Spinal cord contusion is the most common type of injury in closed and non-penetrating spinal cord injuries. A bruise occurs when a vertebra is fractured with its displacement, intervertebral disc prolapse, or vertebral subluxation. When the spinal cord is contused, structural changes always occur in the substance of the brain, roots, membranes, and vessels (focal necrosis, softening, hemorrhages).
The nature of motor and sensory disorders is determined by the location and extent of the injury. As a result of a spinal cord contusion, paralysis, changes in sensitivity, dysfunction of the pelvic organs, and autonomic disorders develop. Trauma often leads to the appearance of not one, but several areas of injury. Secondary disorders of the spinal circulation can cause the development of foci of softening of the spinal cord several hours or even days after the injury.
Spinal cord contusions are often accompanied by subarachnoid hemorrhage. In this case, an admixture of blood is detected in the cerebrospinal fluid. The patency of the subarachnoid space is usually not impaired.
Compression of the spinal cord occurs when a vertebra is fractured with displacement of the fragments or when there is a dislocation or herniation of an intervertebral disc. The clinical picture of spinal cord compression can develop immediately after injury or be dynamic (increasing with spinal movements) if it is unstable. As in other cases of SMT, the symptoms are determined by the level of damage, as well as the severity of compression. Depending on the severity of the injury, restoration of impaired functions occurs within 3-8 weeks. However, with severe bruises that cover the entire diameter of the spinal cord, the lost functions may not be restored.
There are acute and chronic compression of the spinal cord. The latter mechanism occurs when the compressing agent (bone fragment, prolapsed disc, calcified epidural hematoma, etc.) persists in the post-traumatic period. In some cases, with moderate compression, after the acute period of SMT has passed, a significant or complete regression of symptoms is possible, but their reappearance in the long term due to chronic trauma to the spinal cord and the development of a focus of myelopathy.
There is a so-called hyperextension injury of the cervical spine (whiplash injury), which occurs in car accidents (rear impact with incorrectly installed head restraints or their absence), diving, falling from a height. The mechanism of this spinal cord injury is a sharp hyperextension of the neck, exceeding the anatomical and functional capabilities of this section and leading to a sharp narrowing of the spinal canal with the development of short-term compression of the spinal cord. The morphological focus that forms in this case is similar to that of a bruise. Clinically, hyperextension injury is manifested by spinal cord lesion syndromes of varying severity - radicular, partial dysfunction of the spinal cord, complete transverse lesion, anterior spinal artery syndrome.
Hematomyelia, if not combined with other forms of structural damage to the spinal cord, is characterized by a favorable prognosis. Neurological symptoms begin to regress after 7-10 days. Restoration of impaired functions may be complete, but more often certain neurological disorders remain. Hemorrhage in the spinal cord. Most often, hemorrhage occurs when blood vessels rupture in the area of the central canal and posterior horns at the level of the lumbar and cervical thickenings. Clinical manifestations of hematomyelia are caused by compression of the posterior horns of the spinal cord by gushing blood, spreading to 3-4 segments. In accordance with this, segmental dissociated disturbances of sensitivity (temperature and pain) acutely occur, located on the body in the form of a jacket or half-jacket. When blood spreads to the area of the anterior horns, peripheral flaccid paresis with atrophy is detected, and when the lateral horns are affected, vegetative-trophic disorders occur. Very often in the acute period, not only segmental disorders are observed, but also conduction sensitivity disorders, pyramidal symptoms due to pressure on the lateral cords of the spinal cord. With extensive hemorrhages, a picture of complete transverse lesion of the spinal cord develops. The cerebrospinal fluid may contain blood.
Hemorrhage into the spaces surrounding the spinal cord can be either epidural or subarachnoid.
An epidural spinal hematoma, unlike an intracranial hematoma, usually occurs as a result of venous bleeding (from the venous plexuses surrounding the dura mater). Even if the source of bleeding is an artery passing through the periosteum or bone, its diameter is small and the bleeding quickly stops. Accordingly, spinal epidural hematomas rarely reach large sizes and do not cause severe compression of the spinal cord. The exception is hematomas caused by damage to the vertebral artery during a fracture of the cervical spine; such victims usually die from circulatory disorders in the brain stem. In general, epidural spinal hematomas are rare.
Clinical manifestations. Epidural hematomas are characterized by an asymptomatic interval. Then, a few hours after the injury, radicular pain appears with varying irradiation depending on the location of the hematoma. Later, symptoms of transverse compression of the spinal cord develop and begin to increase. The source of a subdural spinal hematoma can be both the vessels of the dura mater and spinal cord, and the epidural vessels located at the site of traumatic damage to the dura mater. Subdural spinal hematomas are also rare; usually bleeding inside the dural sac is not limited and is called spinal subarachnoid hemorrhage.
The clinical picture of intrathecal (subarachnoid) hemorrhage in spinal cord injury is characterized by acute or gradual development of symptoms of irritation of the membranes and spinal roots, including those located above the site of injury. Intense pain in the back and limbs, stiffness of the neck muscles, and Kernig's and Brudzinski's symptoms appear. Very often they are accompanied by paresis of the limbs, sensory conduction disturbances and pelvic disorders due to damage or compression of the spinal cord by gushing blood. The diagnosis of hemorrhachis is verified by lumbar puncture: the cerebrospinal fluid is intensely stained with blood or xanthochromic. The course of hemorrhachis is regressive, and complete recovery often occurs. However, hemorrhage in the cauda equina area can be complicated by the development of an adhesive process with severe neurological disorders.
Anatomical damage to the spinal cord occurs at the time of injury or during secondary trauma to the spinal cord with a wounding object, bone fragments, or when it is overstretched and ruptured. This is the most severe type of SMT, since restoration of anatomically damaged spinal cord structures never occurs. Occasionally, anatomical damage is partial, and Brown-Séquard syndrome or another of those described above develops, but more often such damage is complete. Symptoms are determined by the nature and level of the lesion.
Consultation with a neurosurgeon
neurosurgeon, leading researcher at the Department of Pediatric Neurosurgery, Ph.D. Sysoev Kirill Vladimirovich
author of FEDERAL CLINICAL GUIDELINES FOR THE TREATMENT OF SPINAL BIFIDAS AND FSM IN CHILDREN, approved by the decision of the XXXX Plenum of the Board of the Association of Neurosurgeons of Russia, St. Petersburg, 04/16/2015.
CONTACTS: e-mail
REVIEWS ON SITES: https://prodoctorov.ru/spb/vrach/144441-sysoev/ https://spb.napopravku.ru/doctor-profile/sysoev-kirill-vladimirovich/
The site is for informational purposes only, is not the site of a medical organization, and is not a public offer as defined by the provisions of Article 437 (clause 2) of the Civil Code of the Russian Federation. Interaction with a medical specialist is regulated by the rules of the clinic in which he works.
Hypoglossal nerve (XII) - Anterior branch
1.
HYPOGLOUS NERVE (XII)
, n. hypoglossus. Twelfth cranial nerve. It leaves the brain through numerous roots between the pyramid and the olive, passes through the canal of the same name and descends between the internal jugular vein and the internal carotid artery. Above the posterior edge, the m.mylohyoideus enters the muscles of the tongue. Rice. B.
2.
Lingual branches
, rami linguales. They arise from the trunk of the hypoglossal nerve and innervate the stylohyoid, hypoglossus and genioglossus muscles, as well as the muscles lying inside the tongue. Rice. B.
3.
Radicular threads
, fila radicularia. They emerge from the spinal cord and join into bundles that form the anterior and posterior roots of the spinal nerve. Rice. A.
5.
Anterior root (motor)
, radix anterior (motoria). Contains axons of neurons in the anterior and lateral columns of the gray matter of the spinal cord. Rice. A.
6.
Spinal (sensitive) node
, ganglion spinale (sensorium). Located in the intervertebral foramen as part of the dorsal root near the junction with the radix anterior. Consists of pseudounipolar neurons. Rice. A.
8.
Spinal nerve trunk
, truncus nervi spinalis. It starts from the junction of the anterior and posterior roots and continues to the level of origin of the first branch. Rice. A, Fig. IN.
9.
Anterior branch
, ramus anterior. The largest branch of the spinal nerve. Connecting with the anterior branches of adjacent spinal nerves it forms plexuses. The anterior branches of the thoracic nerves are called intercostal nerves. Rice. A.
From the editor: Causes and diagnosis of whistling in the ears
10.
, ramus posterior. A smaller branch of the spinal nerve, compared to the anterior one, which innervates the skin and autochthonous muscles of the back. Rice. A.
11.
Meningeal branch
, ramus meningeus. Contains sensory and sympathetic fibers. It passes in front of the spinal nerve, enters the spinal canal through the intervertebral foramen and, together with other meningeal branches, forms a plexus that innervates the membranes of the spinal cord. Rice. A.
13.
Ponytail
, cauda equina. It is formed by the roots of the caudal spinal nerves (starting from the 1st and 2nd lumbar) and the filum terminale. Rice. IN.
14.
Medial branch
, ramus medialis. Each of them begins from the posterior branch of the corresponding spinal nerve. Contains motor and sensory fibers. Rice. A.
17.
Suboccipital nerve
, n. suboccipitalis. Posterior branch of the 1st cervical spinal nerve. Passes between the vertebral artery and the posterior arch of the atlas, innervates the short suboccipital muscles. Rice. G.
19.
Greater occipital nerve
, n. occipitalis major. Posterior branch of the 2nd cervical spinal nerve. First it passes between the axial vertebra and the inferior oblique muscle of the capitis, then pierces the trapezius muscle and goes to the semispinalis capitis muscle and the skin of the back of the head. Rice. G.
20.
Third occipital nerve
, n. occipitalis tertius. Posterior branch of the 3rd cervical spinal nerve. Innervates the skin of the posterior neck near the midline. Rice. G.
21.
CERVICAL PLEXUS
, plexus cervicalis. Formed by the anterior branches of the first four cervical spinal nerves (C 1 - 4). Innervates the skin and muscles of the neck.
23.
Cervical (hyoid) loop
, ansa cervicalis (hypoglossi). It consists of fibers from the hypoglossal nerve and the first three cervical spinal nerves. Innervates the hypoglossal muscles. Rice. B.
24.
Anterior root
, radix anterior. It arises from the hypoglossal nerve and contains efferent fibers of the first to third segments of the spinal cord. Rice. B.
25.
Lesser occipital nerve
, n. occipitalis minor. The most superior cutaneous branch. It rises along the posterior edge of the sternocleidomastoid muscle to the skin of the back of the head, lateral to the n.occipitalis mayor. Rice. G.
28.
Greater auricular nerve
, n. auricularis magnus. It crosses vertically the middle of the sternocleidomastoid muscle and goes to the auricle. Rice. G.
29.
Anterior branch
, ramus anterior. Innervates the skin over the parotid gland between the anterior surface of the auricle and the angle of the lower jaw. Rice. G.