Radicular syndrome (radiculopathy)
Spine C1.
The pain is localized in the back of the head, often accompanied by dizziness and possible nausea. The head is tilted to the affected side. Tension of the suboccipital muscles and their palpation pain are noted.
Spine C2.
Pain in the occipital and parietal region on the affected side. Head turns and tilts are limited. Hypoesthesia of the skin of the back of the head is observed.
Spine C3.
The pain covers the back of the head, the lateral surface of the neck, the mastoid region, and radiates to the tongue, orbit, and forehead. In these same areas, paresthesia is localized and hypoesthesia is observed. Radicular syndrome includes difficulty bending and straightening the head, pain in the paravertebral points and points above the spinous process of C3.
Spine C4.
Pain in the shoulder girdle extending to the front surface of the chest, reaching the 4th rib. Distributes along the posterolateral surface of the neck to its middle 1/3. Reflex transmission of pathological impulses to the phrenic nerve can lead to hiccups and phonation disorders.
Spine C5.
Radicular syndrome of this localization is manifested by pain in the shoulder girdle and along the lateral surface of the shoulder, where sensory disturbances are also observed. Shoulder abduction is impaired, deltoid muscle hypotrophy is noted, and the biceps reflex is reduced.
Spine C6.
Pain from the neck spreads through the biceps area to the outer surface of the forearm and reaches the thumb. Hypoesthesia of the last and outer surface of the lower 1/3 of the forearm is detected. Paresis of the biceps, brachialis, supinators and pronators of the forearm is observed. Reduced wrist reflex.
Spine C7.
The pain goes from the neck along the back of the shoulder and forearm, reaching the middle finger of the hand. Due to the fact that the C7 root innervates the periosteum, this radicular syndrome is distinguished by the deep nature of the pain. Decreased muscle strength is noted in the triceps, pectoralis major and latissimus muscles, flexors and extensors of the wrist. Decreased triceps reflex.
Spine C8.
Radicular syndrome at this level is quite rare. Pain, hypoesthesia and paresthesia spread to the inner surface of the forearm, ring finger and little finger. Characterized by weakness of the flexors and extensors of the wrist, and the finger extensor muscles.
Roots T1-T2.
The pain is limited to the shoulder joint and armpit area, and can spread under the collarbone and to the medial surface of the shoulder. Accompanied by weakness and hypotrophy of the hand muscles and numbness. Horner's syndrome is typical, homolateral to the affected root. Dysphagia and peristaltic dysfunction of the esophagus are possible.
Roots T3-T6.
The pain has a girdling character and goes along the corresponding intercostal space. It may cause pain in the mammary gland, and if localized on the left, it can simulate an angina attack.
Spines T7-T8.
The pain starts from the spine below the scapula and along the intercostal space reaches the epigastrium. Radicular syndrome can cause dyspepsia, gastralgia, and pancreatic enzyme deficiency. The upper abdominal reflex may be reduced.
Spines T9-T10.
Pain from the intercostal space spreads to the upper abdomen. Sometimes radicular syndrome has to be differentiated from an acute abdomen. There is a weakening of the mid-abdominal reflex.
Spines T11-T12.
Pain may radiate to the suprapubic and inguinal areas. The inferior abdominal reflex is reduced. Radicular syndrome at this level can cause intestinal dyskinesia.
Spine L1.
Pain and hypoesthesia in the groin area. The pain spreads to the upper outer quadrant of the buttock.
Spine L2.
The pain affects the front and inner thighs. There is weakness in hip flexion.
Spine L3.
The pain goes through the iliac spine and greater trochanter to the anterior surface of the thigh and reaches the lower 1/3 of the medial part of the thigh. Hypesthesia is limited to the area of the inner thigh located above the knee. The paresis that accompanies this radicular syndrome is localized in the quadriceps muscle and adductors of the thigh.
Spine L4.
The pain spreads along the front of the thigh, knee joint, medial surface of the leg to the medial ankle. Hypotrophy of the quadriceps muscle. Paresis of the tibial muscles leads to external rotation of the foot and its “slapping” when walking. Decreased knee reflex.
Spine L5.
The pain radiates from the lower back through the buttock along the lateral surface of the thigh and lower leg to the first 2 toes. The pain zone coincides with the area of sensory disorders. Tibialis muscle hypotrophy. Paresis of the extensors of the big toe, and sometimes the entire foot.
Spine S1.
Pain in the lower back and sacrum, radiating along the posterolateral thigh and lower leg to the foot and 3rd-5th toes. Hypo- and paresthesia are localized in the area of the lateral edge of the foot. Radicular syndrome is accompanied by hypotension and hypotrophy of the gastrocnemius muscle. Rotation and plantar flexion of the foot are weakened. Decreased Achilles reflex.
Spine S2.
Pain and paresthesia begin in the sacrum, covering the back of the thigh and lower leg, sole and big toe. Cramps in the hip adductors are often observed. The Achilles reflex is usually unchanged.
Roots S3-S5.
Sacral caudopathy. As a rule, polyradicular syndrome is observed with damage to 3 roots at once. Pain and anesthesia in the sacrum and perineum. Radicular syndrome occurs with dysfunction of the sphincters of the pelvic organs.
Pain due to spinal hernia
So, the sources that cause pain during a herniated disc can be:
Nerve root.
This is a nerve formation emerging from the spinal cord in the form of two separate roots - the anterior (motor) one, which innervates the muscles and is responsible for the preservation of their characteristics such as strength and tone, and the posterior (sensitive) one, which is responsible for the superficial (sensations of pain, touch, heat, cold) and deep (sensations of position, movement of a body part in space, its weight, feelings of pressure, vibration) sensitivity. These (intradural) sections of the root are extremely rarely affected by a disc herniation. Much more often, the hernia compresses the extradural part of the root, located outside the dura mater, namely the Nageotte radicular nerve (the area from the dura mater to the dorsal ganglion) or the ganglioradicular segment (the spinal ganglion and the corresponding length of the anterior root).
Radicular pain with a spinal hernia can be caused by the following mechanisms of its damage:
1) compression (squeezing) of the root. It can be carried out:
- directly by the hernia itself or by bone growths (osteophytes), thickened (hypertrophied) ligaments and capsules of the intervertebral joints, which often accompany a herniated disc;
- enlarged due to impaired blood outflow by the epidural venous plexuses located in close proximity to the disc herniation;
- edema that develops around the hernia as a result of venous stagnation, leading to increased permeability of the vein walls, or as a result of contact of the part of the nucleus pulposus that has fallen into the epidural space with vascular structures and cells of the immune system.
2) traction (stretching) of the root. Sometimes the location or side of the hernia may not coincide with the area of radicular damage. For example, damage to the L5 root can occur with a LI-II hernia, which cannot be explained by a compression mechanism, since the L1 and L2 roots can be compressed at the level of the LI-II disc, but the L5 root cannot be compressed, since this can only happen at the level LIV-V or LV-SI disks. The mechanism of such a lesion is explained precisely by the stretching of the L5 root due to compression of the dural sac by a hernia, at a higher level LI-II, with its displacement and, as a consequence, stretching of the root. Similarly, due to stretching, damage to the roots on the right side is sometimes observed with a left-sided hernia and vice versa.
3) intraradicular edema of the root. Swelling can be localized not only around the root at the point of its contact with the hernia, but also inside the root itself, leading to mechanical irritation of its fibers and the appearance of pain impulses due to this.
4) chemical irritation of the root. At the point of contact of the root with the disc herniation, as well as inside the root itself, an inflammatory reaction is usually present in the acute phase. It represents not only swelling, but also the presence of cells of the immune system, as well as chemicals involved in starting and maintaining inflammation. Some of them function as algogens, that is, substances capable of stimulating the appearance of pain impulses in them when in direct contact with the fibers of the root.
Radicular pain is not the only type of pain that occurs in patients with disc herniation, however, as can be seen from the previous description, it has many triggering mechanisms. Moreover, in different clinical cases one or another mechanism may predominate.
So, for example, with subligamentous (subglottic) hernias, the nucleus pulposus does not come into contact with the vessels of the epidural tissue. It is closed from it by the posterior longitudinal ligament in subligamentous extrusions and by the posterior longitudinal ligament along with the unruptured part of the fibrous ring in protrusions. As a result of the absence of such contact, a massive autoimmune inflammatory reaction usually does not develop. At the same time, at the first deep ruptures of the fibrous ring, an autoimmune inflammatory reaction is still possible, since the outer third of the fibrous ring contains vessels that are injured during tears. As a result, cells of the immune system can come into contact with the tissue of the nucleus pulposus, which is embedded in the site of the rupture, which triggers an inflammatory reaction. The nucleus pulposus itself, protruding into the site of rupture, edema, which forms in parallel with the accumulation of pro-inflammatory cytokines, irritate the pain receptors of the outer third of the fibrous ring (with protrusions) and the outer third of the fibrous ring and the posterior longitudinal ligament (with subligamentary extrusions) mechanically, and algogens (substances which, upon contact with nerve endings, lead to the occurrence of a pain impulse) cause chemical stimulation of these receptors. However, this inflammatory reaction cannot lead to radicular pain, since it occurs subglottically and does not affect the root. After relief of inflammation, chemical irritation is leveled out, mechanical irritation is reduced due to regression of edema and, as a result, a decrease in pressure on nerve receptors. Gradually, the receptor apparatus of the outer third of the fibrous ring and the posterior longitudinal ligament adapt to the mechanical pressure exerted by the nucleus pulposus embedded in the rupture site and the pain regresses.
Moreover, the development of radicular pain during an exacerbation due to swelling, inflammation and venous stagnation at the site of contact of the hernia with the root and inside the root itself with subglottic hernias, especially extrusions, is not uncommon. In this case, another mechanism for the development of these disorders is triggered. So, if the tear in the annulus fibrosus is deep enough or there is a complete rupture, then the hernia zone becomes a source of stimulation from the receptors of the outer third of the annulus fibrosus and the posterior longitudinal ligament. If the irritation is only mechanical due to the tissue of the nucleus pulposus and there is no additional mechanical (edema) and chemical (inflammatory substances) stimulation, then there may be no pain manifestations at all. This usually happens in the initial stages of development of a disc herniation, when after stopping the exacerbation, usually through medication, the pain usually regresses completely. However, regular mechanical stimulation by the nucleus pulposus of the receptor apparatus of the fibrous ring and the posterior longitudinal ligament leads to the emergence of a chronic muscular-tonic reaction at the level of the hernia and nearby segments, which gradually changes the muscles structurally, leading them not only to spasm, but also to dystrophy and fibrosis. As a result, despite the absence of acute spasm, the muscles become shortened and tightened. This changes the relative position of their fixation points on the vertebrae, which creates an asymmetrical installation of the herniated spinal motion segment. The muscles thus become more prone to developing acute spastic reactions as a result of exposure to various provoking factors. They can be heavy lifting, unsuccessful, uncoordinated movement, stress, hypothermia, draft, infectious disease and many other, sometimes seemingly unimportant, factors. They essentially represent the last straw, which further shortens the muscles, leading to the development of more pronounced asymmetry of the vertebrae at the level of the hernia. This leads to a change in the position of the hernia in the spinal canal. It begins to compress the epidural venous plexuses, blocking the blood outflow pathways from the canal at this level. As a result, the veins increase in volume, their walls stretch and become more permeable, swelling develops and blood cells leave the vascular bed, with the development of an inflammatory reaction. The root begins to be compressed by a conglomerate consisting of a hernia, enlarged veins and edematous fluid, which leads to mechanical compression of its fibers and vessels with the development of edema, inflammation and cellular infiltration of the root itself.
The change in the position of the vertebrae described above and, as a consequence, the hernia in the spinal canal, can lead not only to compression of the veins with a subsequent cascade of the described reactions, but also to the movement of the hernia closer to the root, leading to its mechanical compression by the hernia itself. Along with a change in the spatial location of the hernia, the localization can also be changed by other structures - osteophytes, thickened ligaments and joint capsules, which can also lead to a compressive effect on the roots.
The described mechanism for the development of radicular pain is predominant, since it is characteristic of subligamentary (subglottic) hernias, and they are found in practice much more often than transligamentous (transligamentous) hernias. Subglottic hernias, as a rule, form slowly, increasing gradually, so most of them are quite dense. As the nucleus pulposus moves beyond the fibrous ring into the subglottic space, its ability to receive nutrients and moisture from somewhere is gradually lost, it turns into a fairly dense cartilaginous mass, which, as the hernia grows, is filled with more and more dehydrated cartilaginous masses. In this case, exacerbations of subglottic hernias, however, occur in most cases quite acutely, which is explained by the muscle reactions described above with the development of vertebral asymmetry with subsequent relocation of the hernia towards the radicular nerve.
With transligamentous hernias, the mechanism of radicular pain is somewhat different. These hernias usually form against the background of subligamentous hernias. Initially, a subligamentous hernia gradually develops, which then simultaneously, as a result of rupture of the posterior longitudinal ligament, enlarges and becomes transligamentous. A fragment of the nucleus pulposus suddenly appears in the epidural space, coming into contact with a large abundance of vessels located here. It is regarded by the immune system as foreign because it has not previously come into contact with it, which triggers a powerful autoimmune inflammatory response. Also, a fallen fragment of the nucleus pulposus can mechanically compress the root itself. At the same time, by compressing the veins, it can cause stagnation of venous blood in the epidural space, exacerbating swelling and inflammation around and inside the root. The muscular-tonic reaction here, as a rule, is secondary and develops as a result of intense irritation of the root, although it can further enhance the asymmetry of the vertebrae and the narrowing of the canal, bringing the hernia even closer to the root, thereby aggravating its compression.
Having described in detail the radicular version of pain, we can move on to other sources of pain that cause pain during a spinal hernia. The next, and most common, source of pain during a hernia is:
Muscles and fascia.
Pain from a herniated spine, the source of which is these structures, is called myofascial. The source of pain manifestations in myofascial disorders are muscle pain receptors (nociceptors). The main mechanism of their activation is mechanical irritation by spasmed and compacted muscle fibers and fascia (connective tissue membranes surrounding muscle fibers and muscles). This irritation can occur due to diffuse shortening of the muscles or the formation of local compactions in them, called trigger points (trigger points). The peculiarity of muscle disorders in patients with hernias is that due to the presence of a persistent source of mechanical irritation in the structures of the fibrous ring and the posterior longitudinal ligament, regular impulses are maintained, causing chronic spasm of the muscles of the hernial and nearby segments. It leads to disruption of the blood supply to muscle fibers and, as a consequence, to their dystrophy, and subsequently atrophy and fibrosis. Dystrophic-atrophic reactions are aggravated by a decrease in the size of the intervertebral foramen, which traditionally accompanies disc herniation. In the narrowed foramen, regular trauma to the radicular nerve occurs, the fibers of which, outside the intervertebral foramen, become part of the spinal nerve, and its posterior branch provides innervation to the paravertebral muscles. As a result, not only a deficiency in the supply of nutrients to the muscles develops, but also a disruption in the processes of their absorption, since it is the nerves that are responsible for trophism, that is, the consumption of nutrients in accordance with needs. When innervation disorders develop as a result of trauma to the nerve root, the ability of muscles to absorb the required amount of nutrients is reduced. As a result, the muscle fibers fall into a state of contracture, their atrophy develops, and the layers of connective tissue between the muscle fibers thicken. All this gradually increases the irritation of muscle pain receptors, creating impulses from them, and when its severity exceeds the pain threshold, that is, the ability of spinal cord cells to resist the entry of pain impulses, myofascial pain occurs. Increased impulses from the muscles can occur smoothly as their compaction increases, or acutely due to the additional layering of spasm. It can be triggered by various factors, from heavy lifting, awkward movements and uncomfortable positions, to hypothermia, drafts, stress, infectious diseases and other factors that can cause weakening of the body.
The described sequence of processes in the muscles is valid not only for the paravertebral muscles of the spinal motion segment affected by a hernia, but also for distant muscles included in the zone of innervation of the root, which is subject to periodic trauma due to the narrowing of the canal at the level of the hernia localization. The fact is that each root innervates not only the skin and muscles along the spine, but also remote areas: cervical roots - the shoulder girdle and arm, pectoral roots - the torso, lumbar roots - the pelvis and legs. As a result, myofascial disorders can develop in these areas, gradually leading to the development of pain in them. Thus, a person without signs of gross compression of the root may experience pain associated with tightening and spasm of muscles in the arm, shoulder girdle, shoulder blade with a cervical hernia, in the buttock, groin, lower limb - with a lumbar hernia.
Myofascial pain during a spinal hernia cannot always be explained by the localization of the hernia, since to a certain extent they are always present even before the hernia appears, both at the level of the part of the spine in which the hernia subsequently formed, and at the level of other areas of the spine. Myofascial disorders are an important component of biomechanical disorders that develop for various reasons before the appearance of a hernia, often from childhood, accumulating over the years and gradually leading to overload of the most vulnerable regions of the spine with the subsequent development of osteochondrosis and hernias. These disorders, against the background of the addition of myofascial disorders caused by the hernia itself, can be aggravated, leading to the appearance of pain in other regions of the spine not associated with the hernia.
In addition to the nerve root, muscle and fascial structures, pain from a spinal hernia can also be caused by:
Ligaments.
Most often, the posterior longitudinal ligament is involved in the pathological process. Pain with a spinal hernia that occurs when it is involved in the process may be associated with mechanical irritation due to compression by the nucleus pulposus. In the acute phase, mechanical compression can be aggravated due to the addition of edema; also, as a result of the development of the inflammatory reaction, chemical irritation of the receptors appears.
When a hernia appears, a violation of the stability of the spinal motion segment often develops due to the deterioration of the fixation of the vertebral bodies by the weakened disc. This may involve other ligaments of the spinal motion segment in the pathological process, leading to irritation of their receptors due to overstretching as a result of increased mobility of the vertebrae. Irritation of the receptor apparatus of the ligaments usually produces fairly local pain, at the level of the location of the ligament involved in the pathological process, but so-called sclerotomal pain can also occur, the source of which is the spinal ligaments, and the pain is localized at a distance in the extremities.
Disks.
Pain receptors of the discs, as mentioned above, are localized in the outer third of the fibrous ring, therefore discogenic pain occurs during a spinal hernia, this is associated with a complete or almost complete rupture of the ring, reaching the indicated sections of the disc. The mechanism of irritation of receptors in the acute stage is associated with their mechanical compression by the nucleus pulposus and edema, as well as with the influence of proinflammatory cytokines that irritate them chemically. As the exacerbation subsides, the role of edematous and chemical factors is significantly reduced or disappears. The factor of compression of receptors by the nucleus pulposus persists, which can lead to chronic pain in the affected part of the spine. Adaptation of receptors to mechanical stress may develop with gradual relief of pain. A significant role is played by therapeutic effects that reduce the load on the hernial disc, which leads to a more uniform distribution of intradiscal pressure and a decrease in the degree of compression of the receptors in the zone of rupture of the fibrous ring.
Joints.
The asymmetrical position of the intervertebral joints is a frequent companion to herniated intervertebral discs, which is caused by the development of changes in the paravertebral muscle structures. Densified and spasmed muscles, attaching to the vertebrae, create asymmetrical traction, removing the vertebrae and their joints from a state of stable equilibrium into asymmetrical positions. This can cause mechanical pressure on the cartilaginous structures of the joints with irritation of their receptors, as well as stretching or compression of the joint capsules, leading to joint pain in a spinal hernia.
All the mechanisms described above can lead to two types of pain when a disc herniation occurs - nociceptive and neuropathic. Nociceptive pain is associated with irritation of nociceptors (pain receptors), and neuropathic pain is associated with nerve trunks, that is, roots. Nociceptive pain includes myofascial, ligamentous, discogenic and arthrogenic (articular) pain, and neuropathic pain includes radicular pain. Wherever pain impulses arise, in pain receptors or a root, they then enter the spinal cord, and then along pathways into the subcortical structures and cerebral cortex, where awareness of the presence of pain and all its characteristics occurs. When pain impulses reach brain structures, certain areas of the brain are also activated, which are involved in the fight against pain due to a number of chemicals - serotonin and norepinephrine. The nerve fibers of the analgesic system are directed in the opposite direction to the paths of the pain system, that is, from top to bottom, from the brain to the spinal cord and end on the pain cells of the posterior horn, inhibiting them by increasing the pain threshold. The higher the level of serotonin and norepinephrine acting on the neurons of the dorsal horn, the higher their pain threshold and the fewer pain impulses enter the brain.
At the initial stages, in most patients, the activity of the analgesic system is quite high and the success of pain relief is determined by the speed of elimination of all the sources of pain impulses described above, which directly depends on the correctness and timeliness of therapeutic measures. If treatment measures are carried out correctly and as quickly as possible, increasing the activity of the analgesic system allows for faster recovery. If the timing of correct therapeutic measures aimed at eliminating all sources of pain is delayed, then the anti-pain system begins to gradually deplete due to a decrease in the reserves of serotonin and norepinephrine in the central nervous system. This lowers the pain threshold of dorsal horn cells that transmit pain impulses to the brain, making them easier to pass. The lack of adequate therapeutic measures over time makes these cells so excitable that they not only cease to prevent pain impulses from entering the brain, but also begin to generate them themselves. Plus, the number of cells conducting pain impulses increases. All this leads to a gradual chronicization of pain, as well as the development of depressive states, since a decrease in the level of serotonin and norepinephrine in the structures of the central nervous system is also responsible for the development of emotional and affective disorders, in particular depression.
Having considered the importance of timely and correct pain relief for spinal hernia, we should indicate the main areas in which pain manifestations in this disease can be localized.
Pain due to a spinal hernia may have a deep, unclear localization or, conversely, a superficial pain, occurring in one or more of the following areas:
For cervical hernias:
- cervical spine;
- head;
- lateral, anterolateral surface of the neck;
- shoulder girdle, interscapular region;
- areas of the scapula, shoulder, elbow, wrist joints;
- arm (shoulder, forearm, hand);
- supra- or subclavian region;
- anterior surface of the chest.
For hernias of the thoracic spine:
- thoracic spine;
- posterior, lateral, anterior surface of the chest;
- epigastric region.
For hernias of the lumbar spine:
- lumbar spine;
- sacrum;
- coccyx;
- buttocks;
- areas of the hip, knee, ankle joints;
- leg (thigh, lower leg, foot);
- groin area;
- area of the anterior abdominal wall.
The nature of the pain can be:
- pulling;
- aching;
- aching;
- twisting;
- piercing;
- shooting.
A man in cross-section. Nervous system. Spinal cord and spinal nerves
The nervous system plays the main role in regulating the activities of all organs and systems of the body, combining them into a single whole and communicating the body with the environment. The nervous system includes the brain and spinal cord, as well as nerves, ganglia, plexuses, etc. All these formations are predominantly built from nervous tissue, which is capable of being excited under the influence of irritation from the environment internal or external to the body and conducting excitation in the form of a nerve impulse to various nerve centers for analysis, and then transmitting the generated one to the executive organs to obtain a response from the body in the form movement (movement in space) or changes in the function of internal organs. Irritation is perceived by the nervous system through the sensory organs (eye, ear, organs of smell and taste) and special sensitive nerve endings - receptors located in the skin, internal organs, blood vessels, skeletal muscles and joints.
The nervous system is usually divided into central and peripheral. The central nervous system includes the brain and spinal cord. The peripheral nervous system is formed by nerves that arise from the spinal cord and brain, which are called spinal and cranial, respectively. The peripheral nervous system communicates the brain and spinal cord with all organs of the human body (Fig. 1).
The anatomical and functional unit of the nervous system is the nerve cell - neuron (Fig. 2). The number of neurons reaches 1012. Neurons have processes with which they connect with each other and with innervated formations (muscle fibers, blood vessels, glands). The processes of a nerve cell are functionally unequal: some of them conduct stimulation to the neuron body - these are dendrites, and only one process - the axon - from the nerve cell body to other neurons or organs.
The functioning of the nervous system is based on reflex activity. A reflex is the body’s response to external or internal stimulation with the participation of the nervous system. The reflex pathway in the body is a chain of sequentially interconnected neurons that transmit irritation from the receptor to the spinal cord or brain, and from there to the working organ (muscle, gland). This is called a reflex arc (Figure 3).
Each neuron in the reflex arc performs its own function. Among the neurons, three types can be distinguished: the one that perceives irritation - the sensitive (afferent) neuron, which transmits irritation to the working organ - the motor (efferent) neuron, which connects the sensory and motor neurons - the intercalary (associative neuron). In this case, excitation is always carried out in one direction: from the sensitive to the motor neuron. The processes of neurons are surrounded by membranes and combined into bundles, which form nerves. The membranes isolate the processes of different neurons from each other and contribute to the conduction of excitation. The sheathed processes of nerve cells are called nerve fibers. The number of nerve fibers in different nerves ranges from 102 to 105. Most nerves contain processes of both sensory and motor neurons. Interneurons are predominantly located in the spinal cord and brain, their processes form the pathways of the central nervous system.
The spinal cord is located in the spinal canal along the length from the first cervical to the second lumbar vertebra (see Fig. 1). Externally, the spinal cord resembles a cylindrical cord. 31 pairs of spinal nerves depart from the spinal cord, which leave the spinal canal through the corresponding intervertebral foramina and branch symmetrically in the right and left halves of the body. The spinal cord is divided into cervical, thoracic, lumbar, sacral and coccygeal sections, respectively; among the spinal nerves, 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and 1-3 coccygeal nerves are considered. The section of the spinal cord corresponding to a pair (right and left) of the spinal nerves is called a spinal cord segment.
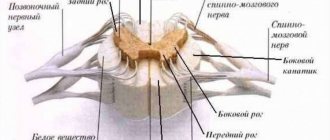
Each spinal nerve is formed as a result of the fusion of the anterior and posterior roots extending from the spinal cord (see Fig. 3, 4). On the dorsal root there is a thickening - the spinal ganglion, where the bodies of sensory neurons are located. The processes of sensory neurons carry excitation from the receptors to the spinal cord. The anterior roots of the spinal nerves are formed by processes of motor neurons, which transmit commands from the central nervous system to skeletal muscles and internal organs.
In connection with the development of the limbs, the areas of the spinal cord that innervate the limbs have received the greatest development. Therefore, there are thickenings in the cervical and lumbar parts of the spinal cord. In the area of thickenings of the spinal cord, the roots of the spinal nerves contain the largest number of nerve fibers and have the greatest thickness.
Internally, the spinal cord consists of gray matter - a collection of cell bodies of neurons - and white matter formed by the processes of neurons. In a cross-section of the spinal cord, the gray matter appears as centrally located paired anterior, posterior and lateral horns (the latter are present only in the thoracic spinal cord), surrounded by white matter (see Fig. 4). In the thickness of the gray matter (the brain, throughout its entire length there is a narrow central canal filled with cerebrospinal fluid.
In the gray matter of the spinal cord, nuclei are distinguished, which are clusters of nerve cells that perform a specific function. The nuclei of the dorsal horns of the spinal cord are sensitive; they transmit nerve impulses from sensory neurons to intercalary neurons. The nuclei of the anterior horns - motor - are represented by the bodies of motor neurons that innervate the muscles of the trunk and limbs. The nuclei of the lateral horns take part in the innervation of internal organs.
The white matter of the spinal cord contains paired anterior, posterior and lateral cords. They are a collection of nerve cell processes that connect various parts of the spinal cord and brain. These are the so-called pathways of the central nervous system.
At the level of the spinal cord, reflex arcs close, providing the simplest reflex reactions, such as tendon reflexes (for example, the knee reflex), flexion reflexes when irritating pain receptors in the skin, muscles and internal organs. An example of a simple spinal reflex is the withdrawal of a hand when it touches a hot object. The reflex activity of the spinal cord is associated with maintaining posture, maintaining a stable body position when turning and tilting the head, alternating flexion and extension of paired limbs when walking, running, etc. In addition, the spinal cord plays an important role in regulating the activity of internal organs, in particular the intestines, bladder, and blood vessels.
Rice. 5 - Posterior coda zones, innervated by spinal nerves. C - cervical nerves D - thoracic nerves L - lumbar nerves S - sacral nerves.
The activity of the spinal cord is controlled by the nerve centers of the brain. Therefore, damage to the spinal cord disrupts the activity of those parts of it that are located below the site of injury, and this is primarily due to the interruption of connections with the brain. For example, if the spinal cord is damaged, urination and defecation may be impaired. With unilateral damage to the spinal cord as a result of injury or disease, muscle paralysis, pain and muscle sensitivity disorders, and vascular disorders develop on the affected side. On the opposite side, voluntary movements are preserved, but pain and temperature sensitivity disappears. This nature of skin sensitivity disorders is explained by the crossover of the conductive pathways, that is, the transition of nerve fibers from one half of the brain to the opposite side. Restoration of reflex activity occurs very slowly, and begins with the simplest reflexes.
spinal nerves,
as already indicated, 31 pairs depart from the spinal cord and innervate the trunk and limbs.
Upon exiting the intervertebral foramen, each spinal nerve divides into branches; two of them are long - anterior and posterior, they are directed to the skin and muscles of the trunk and limbs.
The posterior branches of the spinal nerves are distributed evenly in all parts of the body. Each of the posterior branches is divided into smaller branches that innervate the deep back muscles located along the spine, as well as the skin of the back of the head, neck, back, lower back, and sacral region.
The anterior branches remain evenly distributed only in the thoracic region, where they form the intercostal nerves. The latter, in the amount of 12 pairs, pass in the intercostal spaces along with the vessels. The six lower nerves, reaching the anterior end of the intercostal spaces, continue to the anterior wall of the abdomen. These nerves innervate the intercostal muscles, abdominal muscles, as well as the skin of the chest and abdomen.
In other parts of the body, the anterior branches of the spinal nerves, connecting with each other, form the cervical, brachial, lumbar and sacral plexuses (see Fig. 1). The loss of the uniform course of most of the anterior branches of the spinal nerves is associated with the development of complex muscles of the limbs.
Cervical plexus
formed by the anterior rami of the four superior cervical spinal nerves and lies on the deep muscles of the neck lateral to the transverse processes of the vertebrae. Cutaneous, muscle nerves and the phrenic nerve depart from the plexus. Cutaneous nerves innervate the skin of the lateral parts of the head, auricle, neck and upper chest. Muscle nerves travel to the neck muscles. The phrenic nerve enters the chest cavity and reaches the diaphragm. The innervation of the diaphragm from the cervical plexus is explained by the development of this muscle in the prenatal period in the neck area.
Rice. 6 - Anterior cutaneous zones innervated by spinal nerves. C - cervical nerves D - thoracic nerves L - lumbar nerves S - sacral nerves.
Brachial plexus
formed by the anterior branches of the four lower cervical spinal nerves and a branch from the first thoracic nerve. It is located behind the collarbone and in the armpit. Short and long nerves extend from the brachial plexus. Short nerves emerge from the plexus above the collarbone and innervate the muscles of the shoulder girdle. The largest of them, the axillary nerve, gives branches to the deltoid muscle, shoulder joint and skin of the shoulder. The long nerves of the brachial plexus innervate the muscles, joints and skin of the free upper limb. Among them are the median, ulnar and radial nerves.
Lumbar plexus
formed by the anterior branches of the three upper lumbar spinal nerves, as well as branches from the twelfth thoracic and fourth lumbar nerves. The lumbar plexus lies deep within the psoas muscle. The nerves of this plexus innervate the skin and muscles of the lower abdominal wall, as well as the external genitalia, skin and muscles of the thigh. The femoral nerve is the largest nerve of the lumbar plexus. It enters the thigh under the inguinal ligament and innervates the muscles of the front of the thigh (quadriceps femoris and sartorius), the skin above them, as well as the skin of the inner surface of the leg and foot. The obturator nerve leaves the pelvic cavity on the inner side of the thigh, where it innervates the adductor muscles and skin located here. The femoral and obturator nerves give branches to the hip joint.
Sacral plexus
formed by the anterior branches of the fourth and fifth lumbar, all sacral and coccygeal spinal nerves. The sacral plexus is located in the small pelvis, from the cavity of which the plexus nerves exit through the greater sciatic foramen. Short nerves branch in the pelvic muscles (gluteal muscles, etc.), in the skin and muscles of the perineum and in the external genitalia. Long nerves travel to the back of the thigh. The sciatic nerve - the largest in the human body - innervates the muscles of the back of the thigh, and in the region of the popliteal fossa it is divided into two branches that innervate the knee joint, muscles, skin and joints of the lower leg and foot.
The branches of the spinal nerves also contain autonomic nerve fibers that innervate the vessels and glands of the skin, regulate metabolism in the skeletal muscles, and also go to the internal organs.
From a practical point of view, you should know that each dorsal root of the spinal nerve is related to the innervation of that segment of the skin that is associated with it during development. In the same way, each anterior root innervates those muscles that developed along with it. Therefore, all skin and muscles can be divided into a number of successive radicular zones, or belts, which have innervation from a specific spinal nerve (see Fig. 5, 6). That is why, when the posterior root of a spinal nerve becomes inflamed, girdle pain appears, exactly corresponding to the given radicular girdle of the skin.
Most nerves in the human body are mixed, meaning they contain both sensory and motor nerve fibers. That is why, when nerves are damaged, sensory disorders are almost always combined with motor disorders. However, the zones of innervation of neighboring nerves partially overlap, so complete loss of sensitivity of the skin area, as a rule, does not occur. Changes in the spine with age (for example, with osteochondrosis) and various injuries can affect the condition of the spinal cord and the nerves extending from it. Over the years, intervertebral discs lose elasticity and become flattened. At a certain point, often due to unsuccessful loading movement, nerve roots or nerves are injured in the narrowed intervertebral space. If they are affected, a diagnosis of “radiculitis” is made (Latin radix - root, spine, suffix “it” - indicates the inflammatory nature of the disease).
Source: Quality of Life. Prevention. No. 6, 2003