1.What are neuromas?
Neuromas
are a type of benign tumors formed from Schwann cells of the tissues of the auditory and cranial nerves (VIII pairs).
Schwann cells are auxiliary cells of nerve trunks, named after their discoverer, the German physiologist Theodor Schwann. Otherwise, these tumors are also called vestibular schwannomas or acoustic neuromas (schwannomas). This pathology is quite rare and accounts for approximately 10% of the total number of CNS (central nervous system) tumors. These neoplasms affect women more often than men; the main age range of patients is from 30 to 40 years.
The main function of the auditory nerves is the function of transmitting sounds
to the appropriate brain centers for subsequent processing.
In addition, a certain segment of these nerves is responsible for the functioning of the human vestibular apparatus
- a special, important device that allows you to control the position of the body in space.
A must read! Help with treatment and hospitalization!
Alternating syndromes (Cross syndromes)
The clinical picture is based on alternating neurological symptoms: signs of cranial nerve dysfunction on the affected side, sensory and/or motor disorders on the opposite side. Nerve damage is peripheral in nature, which is manifested by hypotonicity, atrophy, and fibrillation of the innervated muscles. Motor disorders are central spastic hemiparesis with hyperreflexia and pathological foot signs. Depending on the etiology, alternating symptoms have a sudden or gradual development, accompanied by general cerebral symptoms, signs of intoxication, and intracranial hypertension.
Bulbar group
Jackson syndrome is formed when the nucleus of the XII (hypoglossal) nerve and pyramidal tracts are damaged. It manifests itself as peripheral paralysis of half the tongue: the protruding tongue deviates towards the lesion, atrophy, fasciculations, and difficulty pronouncing difficult to articulate words are noted. In the contralateral limbs, hemiparesis is observed, and sometimes there is loss of deep sensitivity.
Avellis syndrome is characterized by paresis of the muscles of the larynx, pharynx, and vocal cords due to dysfunction of the nuclei of the glossopharyngeal (IX) and vagus (X) nerves. Clinically, choking, voice disorders (dysphonia), speech disorders (dysarthria) with hemiparesis, hemihypesthesia of the opposite limbs are observed. Damage to the nuclei of all caudal cranial nerves (IX-XII pairs) causes the Schmidt variant, which differs from the previous form by paresis of the sternocleidomastoid and trapezius muscles of the neck. On the affected side, there is a drooping of the shoulder and limitation in raising the arm above the horizontal level. It is difficult to turn the head towards the paretic limbs.
The Babinski-Nageotte form includes cerebellar ataxia, nystagmus, Horner's triad, cross-paresis and superficial sensitivity disorder. With the Wallenberg-Zakharchenko variant, a similar clinical picture is revealed, dysfunction of the IX, X and V nerves. It can occur without paresis of the limbs.
Pontine group
Millard-Gübler syndrome appears with pathology in the area of the nucleus of the VII pair and the fibers of the pyramidal tract; it is a combination of facial paresis with hemiparesis of the opposite side. A similar localization of the focus, accompanied by irritation of the nerve nucleus, causes the Brissot-Sicard form, in which instead of facial paresis, facial hemispasm is observed. The Fauville variant is distinguished by the presence of peripheral paresis of the VI cranial nerve, giving the clinic of convergent strabismus.
Gasperini syndrome - damage to the nuclei of the V-VIII pairs and sensitive tract. Facial paresis, convergent strabismus, facial hypoesthesia, hearing loss are noted, and nystagmus is possible. On the contralateral side, conduction-type hemihypesthesia is observed, motor skills are not impaired. The Raymond-Sestan form is caused by damage to the motor and sensory pathways and the middle cerebellar peduncle. Dyssynergia, discoordination, hypermetria are found on the side of the lesion, hemiparesis and hemianesthesia are found on the contralateral side.
Peduncular group
Weber's syndrome is a dysfunction of the nucleus of the third pair. It is manifested by drooping of the eyelid, dilation of the pupil, rotation of the eyeball towards the outer corner of the eye, cross hemiparesis or hemihypesthesia. The spread of pathological changes to the geniculate body adds visual disturbances (hemianopia) to the indicated symptoms. Benedict's variant - pathology of the oculomotor nerve is combined with dysfunction of the red nucleus, which is clinically manifested by intention tremor and athetosis of the opposite limbs. Sometimes accompanied by hemianesthesia. With the Nothnagel variant, oculomotor dysfunction, cerebellar ataxia, hearing impairment, contralateral hemiparesis are observed, and hyperkinesis is possible.
Extra-brain alternating syndromes
Hemodynamic disturbances in the subclavian artery system cause the appearance of the vertigohemiplegic form: symptoms of dysfunction of the vestibulo-cochlear nerve (tinnitus, dizziness, loss of hearing) and cross hemiparesis. The opticohemiplegic variant develops when there is discirculation in the ophthalmic and middle cerebral arteries simultaneously. It is characterized by a combination of optic nerve dysfunction and crossed hemiparesis. Asphymohemiplegic syndrome occurs when the carotid artery is occluded. Hemispasm of the facial muscles, opposite to hemiparesis, is observed. A pathognomonic sign is the absence of pulsation of the carotid and radial arteries.
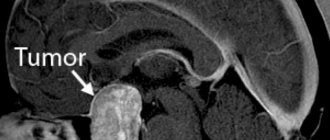
2.Symptoms of neuroma of the cranial nerves
The symptomatic picture of a tumor of the auditory nerve is determined by the factor of compression of certain nerve fibers. The larger the size of the tumor, the brighter its manifestations will be. So, among the initial symptoms we can identify the following:
- hearing impairment (decreased hearing acuity, noise or ringing in the ears);
- numbness of areas of the face, taste changes;
- difficulty maintaining balance, dizziness and a feeling of uncertainty when walking.
These symptoms are caused by compression of the small tumor on the facial and auditory nerves, including its vestibular part.
With further growth of the tumor, the following symptoms may be added to the above symptoms:
- nystagmus (frequent involuntary movements of the eyeballs);
- decreased sensitivity of the cornea, tongue, mucous membranes of the nasal passages;
- pain on the side of the tumor caused by compression of the facial trigeminal nerve;
- violation of movement coordination.
These disorders are caused by compression of the most important centers of the brain stem. If the growth of the tumor is not further prevented, the clinical picture will be complemented by:
- mental disorders;
- loss of vision and hearing;
- violation of the act of chewing and swallowing;
- increased intracranial pressure.
These negative changes occur due to impaired circulation of the cerebrospinal fluid (CSF) and the resulting development of hydrocephalus and compression of the vagus nerve centers, leading to paresis (paralysis) of the larynx.
Visit our Neurosurgery page
What is abducens nerve palsy?
Paresis of the abducens nerve of the left eye and the right eye occurs with the same frequency. In most cases, the disease affects one side, rarely both. Paresis of the abducens nerve can be suspected by characteristic features: the patient has difficulty turning his eye towards the affected nerve. Paresis of the abducens nerve impairs the function of the rectus lateralis muscle, and the patient cannot fully avert the eye to the side. The patient experiences diplopia when looking straight ahead, which intensifies when the eye is turned towards the affected side. Other symptoms of abducens nerve palsy include:
- forced position of the head (impaired vision leads to an attempt to adapt to the changes that have arisen, which provokes the occurrence of involuntary positions);
- uneven gait (also associated with visual impairment);
- loss of orientation;
- dizziness.
Causes of cranial nerve damage
Damage to the cranial nerves is caused by a variety of causes, among which pathologies of the musculoskeletal system are leading. Most often, compression occurs due to the following diseases:
- curvature of the spinal column in the cervical and thoracic region (including scoliosis);
- injuries to the neck and collar area, leading to dislocation and subluxation, fracture or crack of the bone tissue of the vertebral bodies, occipital bone, spinal processes, stretching and rupture of ligamentous and tendon fibers, hematomas inside the muscles, etc.;
- unstable position of the vertebral bodies, their periodic displacement relative to the central axis and each other such as retrolisthesis, antelisthesis, laterolisthesis, etc.;
- absorption of the body of the first vertebra by the occipital bone (assimilation of the atlas);
- subluxation or dislocation of the first cervical vertebra;
- cicatricial deformation of the anterior or posterior longitudinal ligament of the spine (they begin in the area of the coccyx and are attached to the occipital bone;
- formation of osteophytes of the cervical vertebral bodies;
- cerebrovascular accident due to the development of posterior vertebral artery syndrome;
- destruction of the joint between the first and second cervical vertebrae;
- degenerative dystrophic disease of the cartilage tissue of the intervertebral discs (osteochondrosis) and its complications, such as protrusion, extrusion and intervertebral hernia;
- rheumatic pathologies such as multiple sclerosis, ankylosing spondylitis, systemic lupus erythematosus, etc.
- Only an experienced doctor can identify the exact cause of damage to the paired cranial nerves. Therefore, it is strongly recommended that if characteristic signs appear, you contact a specialist.
At home, you can only eliminate all possible risk factors. Their presence in a person’s life significantly increases the likelihood of developing those pathological processes that cause damage to the cranial nerves.
Here are the main risk factors that should be eliminated from your daily life if possible:
- maintaining a sedentary lifestyle with predominantly sedentary work - the processes of microcirculation of blood and lymphatic fluid are disrupted, muscle fibers undergo dystrophy, and the process of destruction of tissues of the musculoskeletal system and the spinal column begins;
- frequent injury to the neck and collar area (usually the risk group includes car drivers who, while driving, are forced to frequently brake urgently while driving, this provokes tilting of the skull and injury to the upper parts of the neck);
- incorrect posture and curvature of the spinal column in any part (compensatory displacement of the vertebral bodies occurs, including in the area of attachment to the occipital bone);
- excess body weight - significantly increases all shock absorption and mechanical loads on the spinal column, accelerates the process of its destruction;
- incorrect placement of the foot when walking and running in the form of flat feet and club feet;
- labor associated with prolonged static tension of the muscles of the neck and collar area;
- smoking and drinking alcohol (spasms of small blood vessels occur and blood supply to tissues deteriorates);
- incorrect organization of the sleeping and working space from an ergonomic point of view.
All potential causes should be addressed before treatment is started. During the initial consultation, an experienced vertebrologist or neurologist collects medical history data in order to identify all the negative influence factors that are present in the life of a particular patient. He then gives practical, personalized advice. Compliance with them allows you to stop the destructive process and prepare the body for the recovery process.
Prevention
The main method is the complete cure of infections that we consider banal and habitual. Guillain-Barré syndrome often develops with a slight weakening of the immune system, which is possible in every person.
The easiest way to protect yourself is to check your current immune status. This will only take a few days, and any abnormalities detected can be treated in time.
Doctors at the CELT clinic have at their disposal not only the latest diagnostic equipment, but also the latest treatment techniques that have received worldwide recognition. The main role in prevention belongs to the patient who seeks examination and treatment in a timely manner.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Treatment rules
Today, two main pathogenetic methods of treating Guillain-Barré syndrome are known, and both are successfully used by CELT specialists. These are plasmapheresis and intravenous immunotherapy. These methods can be used in isolation or used in combination, it all depends on the specific clinical situation. Treatment is aimed at removing or neutralizing immune complexes circulating in the patient’s blood. Both treatment methods are equivalent and almost always lead to recovery. Treatment stops the process of destruction of peripheral nerves, shortens the recovery period, and helps reduce neurological deficits.
Plasmapheresis is a blood purification operation. Most often, hardware plasmapheresis is used on continuous separators, during which the blood taken from the body is divided into formed elements (or blood cells) and plasma (or serum). All toxic substances are in the plasma, so it is removed. The person is given back his own blood cells, diluted, if necessary, with plasma-substituting solutions or donor plasma. The duration of the procedure is about one and a half hours, the entire course consists of 3 or 5 sessions. No more than 50 ml/kg of plasma body weight is removed at a time.
During treatment, blood parameters are monitored: electrolytes, hematocrit, clotting time and others.
Intravenous immunotherapy is the administration of a human immunoglobulin class G drug. These immunoglobulins stop the production of antibodies to one’s own nerves, simultaneously reducing the production of substances that support inflammation. These drugs are indicated for the pathogenetic treatment of Guillain-Barré syndrome in both adults and children.
Simultaneously with specific treatment, careful patient care is provided, including the prevention of bedsores, pneumonia, and contractures. Treatment of concomitant infections is often required. Venous thrombosis is prevented, tube feeding is carried out, and excretory function is monitored. Bedridden patients undergo passive exercises, as well as early verticalization to avoid blood flow disorders. If there is a threat of developing contacture (immobility of joints), paraffin procedures are possible. If necessary, motor simulators based on biofeedback are used.
Patients with damage to myelin sheaths recover faster, while axonal damage requires a longer period of rehabilitation. Axonal lesions often leave behind neurological deficits that are difficult to correct.