- When is Morton's neuroma surgery performed?
- Diagnosis and preparation for surgery for Morton's neuroma
- How does the surgical treatment of Morton's neuroma proceed at the Gelenk Clinic?
- Which surgeon operates on Morton's neuroma?
- What type of anesthesia is offered to the patient before Morton's neuroma surgery?
- Postoperative period, rehabilitation treatment and aids after surgery for Morton's neuroma
- Will I feel pain after Morton's neuroma surgery?
- What are the conditions of stay at the Gelenk Clinic?
- What should you pay attention to after surgical treatment of Morton's neuroma?
- What is the cost of foot surgery?
- How to make an appointment with a doctor and surgery for Morton's neuroma?
Morton's neuroma (red) as swelling between the metatarsal bones (blue).
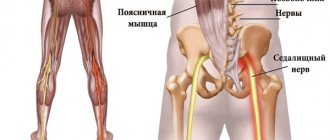
Irritation of the nerve (yellow) develops a burning and stabbing pain throughout the area of its supply. © Dr. med. Thomas Schneider Morton's neuroma is a benign thickening of the nerves in the metatarsal area. The consequence of the disease is shooting, burning and stabbing pain in the plantar region, as well as in the toes (metatarsalgia). The pain is so severe that the patient experiences relief and improvement in general condition only when he sits down and takes off his shoes. Thus, when the patient is not wearing shoes, the pain goes away much faster. In addition, characteristic symptoms of Morton's neuroma are tingling or numbness in the toes. Morton's neuroma is a common consequence of transverse flatfoot, sometimes accompanied by hallux valgus. Women suffer from Morton's neuroma much more often than men. The reason for this is most likely due to different fashions for shoes: High heels, as well as shoes with pointed toes, put strong pressure on the front arch of the foot and can provoke the appearance of transverse flat feet. As a result of this pathology, the position of the metatarsal bone changes in the patient and the pressure on the nerves passing along the plantar region of the foot increases.
Morton's neuroma is also diagnosed in men, most often in those who engage in high-volume running sports. Morton's neuroma is often observed between the 3rd and 4th toes, and less commonly between the 2nd and 3rd toes.
send a request
When is Morton's neuroma surgery performed?
In order to correctly assess the patient’s condition and prescribe the correct treatment, Gelenk Clinic specialists will need to provide current MRI results. Based on the MRI images, the doctor determines the degree of need for surgical treatment of Morton's neuroma. If there are certain indications, the patient is prescribed the best surgical technique for him.
In the early stages, treatment of the disease is carried out using conservative methods, namely special insoles and gymnastic exercises for the feet. If the quality of life is significantly limited, and if the patient experiences severe pain despite conservative treatment, the doctor will refer him for surgery. If the thickening is 0.8 cm in size, a nerve-sparing operation (neurolysis) is performed. If the swelling of Morton's neuroma is greater than normal, the nerve is removed through neurectomy.
Neuralgia of the foot - treatment
The following approaches may help relieve leg pain:
- using hot or cold compresses
- taking painkillers such as ibuprofen
- foot massage
- wearing a splint for support
Also, try to avoid prolonged sitting or standing. Some people find that wearing shoes with wide, soft soles and low heels helps relieve pressure on their feet and nerves. However, for some people with neuralgia, a hard sole may be more beneficial than a soft one.
Drug treatment
Treatment will depend on the cause of the neuralgia in the feet. To treat peripheral or diabetic neuropathy, your doctor may prescribe:
- painkillers
- antidepressants
- anticonvulsants
In some situations, your doctor may recommend deep tissue massage and corticosteroid injections to help manage symptoms, especially if sciatica is the cause. If sciatica occurs as a result of a hernia, abscess, or tumor, the doctor may refer the person for surgery. Doctors may also recommend exercise therapy (PT) because stretching and strengthening the legs and feet can help manage symptoms, including pain. Patients with neuralgia caused by problems other than sciatica may also benefit from surgical treatment. For example, if a patient has tarsal tunnel syndrome, treatment may include surgery to release the nerve—a success rate of up to 96%.
Diagnosis and preparation for surgery for Morton's neuroma
Clinical examination of Morton's Neuroma using a provocative test (Mulder test): A foot specialist diagnoses the disease by compressing the heads of the metatarsal bones and simultaneously palpating the intermetatarsal spaces, which causes pressing pain. © joint-surgeon
Alternative Causes of Forefoot Pain
- Inflammation of the joint located between the bones of the metatarsal and proximal phalanges
- Nerve damage
- Stress (stress fractures) of the metatarsals
- Changes in soft tissue structure, including scars, warts and tumors
- Incorrect weight distribution, as in the case of severe flat feet
Before starting treatment for Morton's neuroma, the doctor conducts a full clinical and imaging diagnosis, which includes a preliminary conversation, physical examination, and MRI with contrast. During magnetic resonance imaging, the patient is in the “lying on his stomach” position, and during the x-ray in the “standing position”. In order to determine how the pressure is distributed under the plantar part of the foot, a podometric study (pedobarography) is carried out at the Gelenk Clinic. Based on the results obtained, the doctor discusses the upcoming operation with the patient.
If the patient’s health condition does not prevent surgical treatment, the operating doctor tells the patient in detail about the course of the operation and also explains possible complications. In addition, you will be referred to an appointment with an anesthesiologist, who will re-analyze the results of the studies and determine whether your condition allows the administration of anesthetics. As a rule, Morton's neuroma surgery takes place the next day after agreement with the operating surgeon and anesthesiologist.
Types of neuralgia
Medical professionals divide neuralgia into categories based on the areas of the body that it affects. The following are some common types of neuralgia :
Trigeminal neuralgia
TN can cause shooting pain in the face.
Trigeminal neuralgia (TN) involves the trigeminal nerve in the head. It has three branches that send signals from the brain to the face, mouth, teeth and nose.
TN is divided into two divisions: type 1 and type 2.
Type 1 TN causes a painful burning or electric shock sensation in some parts of the face. People with type 1 TN experience irregular episodes that come on suddenly.
The duration of these episodes varies among individuals, but can last up to 2 minutes, according to the National Institute of Neurological Disorders and Stroke.
Type 2 TN produces a constant, dull, aching sensation on the face.
The exact cause of TN remains unclear. However, pressure from the enlarged blood vessel can irritate or even damage the trigeminal nerve.
Multiple sclerosis (MS) can lead to TN. MS is a neurological disorder that causes inflammation that damages the myelin sheath surrounding nerve fibers in the central nervous system.
Postherpetic neuralgia
Postherpetic neuralgia (PHN) is a painful condition that affects the nerves of the skin.
According to the Centers for Disease Control and Prevention (CDC), PHN is the most common complication of shingles, affecting about 10–13% of people who develop it.
Shingles is a viral infection that causes blisters and a painful skin rash. The varicella zoster virus, which causes chickenpox, remains dormant in the nervous system and becomes active later in life, causing shingles.
When the virus is reactivated, it can cause inflammation of nerve fibers. This inflammation can lead to permanent nerve damage, which causes pain even after the infection subsides.
Occipital neuralgia
This form of neuralgia affects the occipital nerves, which originate in the neck and send signals to the back of the head.
Occipital neuralgia causes throbbing or shooting pain that begins at the base of the skull and spreads along the scalp. Pain in occipital neuralgia may flow to the back of the eyes.
Occipital neuralgia has many potential causes, including:
- sudden head movements
- tense neck muscles
- lesions or tumors in the neck
- inflamed blood vessels
- infections
- gout
- diabetes
- neck injuries
Peripheral neuralgia
Peripheral neuralgia, or peripheral neuropathy, refers to pain that occurs due to nerve damage in the peripheral nervous system. This includes all nerve fibers outside the brain and spinal cord.
Peripheral neuralgia can affect one nerve or entire nerve groups.
Sustained damage to the peripheral nervous system can affect the nerves that control muscle movement, transmit sensory information, and regulate internal organs.
Peripheral neuralgia can cause pain or numbness in the arms, legs, arms and legs. Other symptoms may include:
- involuntary muscle twitching or spasms
- loss of coordination
- difficulty performing complex motor tasks such as buttoning a shirt or tying shoelaces
- hypersensitivity to touch or temperature
- excessive sweating
- gastrointestinal problems
- difficulty eating or swallowing
- it's hard to talk
Intercostal neuralgia
Intercostal neuralgia affects the nerves that sit just below the ribs. Doctors call the muscles in this area the intercostal muscles.
Several potential factors may contribute to intercostal neuralgia, such as:
- injuries or surgical procedures involving the chest
- pressure on the nerves
- shingles or other viral infections
Intercostal neuralgia causes sharp, burning pain that affects the chest wall, upper abdomen, and upper back. Certain physical movements, such as breathing, coughing, or laughing, can make the pain worse.
Additional symptoms may include:
- tightness or pressure that envelops the chest
- tingling or numbness in the upper chest or upper back
- muscle twitching
- loss of appetite
Diabetic neuropathy
Diabetic neuropathy is the most common complication of diabetes. Because diabetes affects so many people, rates of peripheral neuropathy are now starting to rise.
Symptoms include loss of balance and numbness, tingling and pain. The best way to prevent diabetic neuropathy is to keep your blood sugar levels within an acceptable range.
How does the surgical treatment of Morton's neuroma proceed at the Gelenk Clinic?
Surgery makes sense if conservative treatment, for example, orthopedic insoles, special shoes with butterfly soles, foot exercises, as well as injections of local anesthetics and self-massage do not help relieve pain for a long time. Gelenk Clinic mainly uses two treatment methods: nerve-sparing neurolysis and nerve removal. Each operation lasts about 30 minutes.
Ventral view of the foot: Morton's neuroma is located between the 2nd and 3rd toes. Most often, pathology occurs between the 3rd and 4th fingers. © Viewmedica
Nerve-sparing minimally invasive surgery for Morton's neuroma
Mechanical pressure on the plantar area of the foot leads to pinched nerves. Due to nerve irritation, the connective tissue sheath of the plantar nerve swells and forms scar tissue. There is an accumulation of fluid.
As a result of the swelling, ischemia occurs and the nerves of the foot are no longer supplied with nutrients. Because of this, the patient develops such characteristic complaints as a feeling of numbness, shooting pain and itching (pins and needles) in the foot. Relieving mechanical pressure on the nerve may relieve these symptoms to a certain extent.
The optimal treatment for many compression syndromes (eg, carpal tunnel syndrome) is nerve decompression. If the Morton's neuroma is less than 0.8 cm in size, nerve-sparing surgery is performed
Using the technique of stress relief and, if necessary, decompression of the nerve by repositioning the metatarsal bone, the specialists of our clinic have been achieving excellent results for several years. In particular, Gelenk Clinic has a good record in preventing relapses. Recurrence of the pathology is more likely after nerve amputation (neurectomy), since this operation does not correct the original violation of the arch of the foot. Despite this, neurectomy is the standard treatment for Morton's neuralgia. Too often, for Morton's neuralgia, the plantar nerve is removed without first testing the effectiveness of nerve-sparing treatment.
Advantages of nerve-sparing surgery:
Nerve-sparing endoscopic treatment of Morton's neuroma with a superior approach instead of the conventional plantar approach has the following advantages:
- less scarring and therefore little irritation of the foot nerves
- the risk of hematomas is reduced
- preservation of the plantar nerve, which after complications will stop hurting and return to its original functions
- reduction in relapse rate: due to the reappearance of painful swelling, relapse is not uncommon
- decreased tendency to form painful scars in the area of the metatarsal nerves
Neuroctomy - removal of the inflamed nerve
During this surgery, diseased nerve tissue from the tibial nerve is removed. At the Gelenk Clinic, neurectomy is performed in cases of severe swelling of Morton's neuroma. That is why this surgical treatment requires a preliminary MRI examination, which helps doctors determine the size of the disease. Since slice-by-slice images obtained using magnetic resonance imaging sometimes do not provide complete information about the size and location of Morton's neuroma, the exact technique is chosen directly during surgery after analyzing and examining the thickening.
With surgical access to Morton's neuroma through the head of the metatarsal bone, decompression can be relatively performed, that is, the degree of compression can be reduced. This method of treatment is an appropriate accompanying surgical procedure, since reducing compression reduces the likelihood of relapse, that is, secondary rupture of the stump of the damaged nerve, resulting in swelling of the connective tissue. Surgery for Morton's neuroma with a superior approach avoids scarring on the sole of the foot. This speeds up the wound healing process, and the patient can resume putting weight on the foot a little earlier.
Causes
Neuralgia is caused by pathologies:
- diseases of the nervous system: various nerve lesions, for example, polyradiculoneuritis;
- infectious diseases;
- injuries, pathologies of the spine: spondyloarthritis, spondylosis;
- allergies, drug intoxication;
- hazardous industrial production;
- malignant tumors;
- compression of the nerve during a forced position (professional).
At risk are people who work physically hard or work in the same position: porters, jewelers, watchmakers, programmers, dentists, professional drivers, etc. Due to intoxication, neuralgia can occur in workers in chemical production, paint shops, pharmaceutical plants, etc. The disease can provoke a large number of medical procedures in one area of the body.
Which surgeon operates on Morton's neuroma?
One of the features of the Gelenk Clinic is the trusting relationship between doctors and patients. That is why your attending physician will take care of you from the first examination until the operation itself. This way you will have a specialist whom you can contact at any time convenient for you. The Gelenk Clinic's highly qualified experts in the field of foot and ankle surgery are Dr. Thomas Schneider and Dr. Martin Rinio. Also, Dr. Schneider and Dr. Rinio are certified specialists who are annually audited by the independent German Association of Foot and Ankle Surgeons (German DAF) for advanced training, diagnostics and quality of operative activities. That is why the Gelenk Clinic Orthopedic Medical Center has the honor of being called the Specialized Center for Foot and Ankle Surgery (ZFS).
What type of anesthesia is offered to the patient before surgery?
Typically, surgical treatment of Morton's neuroma is performed under general anesthesia. If the patient refuses this method for personal reasons, there is the possibility of using spinal anesthesia. To do this, the surgeon injects an anesthetic into the spinal canal of the lumbar spine. In this case, the patient is fully conscious. What type of anesthesia is most suitable for the patient is determined during a conversation with the anesthesiologist. Our anesthesiologists are true masters of their craft, who during your appointment will offer you the best method that meets all the indicators of previous examinations.
Neuropathy (neuropathy, neuritis) of the tibial nerve
Neuropathy (neuropathy, neuritis) of the tibial nerve is a disease that leads to the fact that a person cannot bend the fingers normally and also control the foot. In this case, the patient feels extremely painful sensations, since a serious violation of sensitivity occurs. The tibial nerve is a continuation of the sacral plexus nerve, passes between the medial and lateral muscles and further along the foot. The many similarities between tibial nerve neuropathy and other traumatic and inflammatory processes are a topic of discussion among leading experts.
Will I feel pain after Morton's neuroma surgery?
Every operation is associated with some pain—and Morton's neuroma surgery is no exception. As a rule, we try to reduce pain after Morton's neuroma surgery to a minimum. That is why pain treatment begins already during the operation. In most cases, the anesthesiologist will administer a special injection that will numb the foot for about 30 hours. After this, the pain decreases significantly and the patient’s treatment continues with conventional medications. The main thing for us is to ensure a painless postoperative period.
Causes of neuropathy of the lower extremities
The development of the disease may be associated with the following factors:
- long-term exposure to toxic substances (drugs, alcohol, arsenic, lead, mercury, etc.);
- metabolic disorders (diabetes mellitus, thyroid dysfunction, chronic renal failure);
- long-term hypovitaminosis;
- injuries;
- taking certain medications;
- infections (chickenpox, diphtheria, mumps, HIV infection);
- autoimmune diseases (for example, Guillain-Baré syndrome);
- burdened by heredity (genetically determined pathologies, for example, Charcot-Marie-Tooth amyotrophy).
What are the conditions of stay at the Gelenk Clinic?
Private ward at the Gelenk Clinic in Gundelfingen, Germany.
© joint-surgeon During your stay at the Gelenk Clinic, you are usually in a separate room, which has a shower and toilet. In addition, we provide towels, bathrobes and slippers. You can also use a safe and minibar. All rooms are equipped with TV. You only need to take medications, comfortable clothes and nightwear with you. Patient care is provided around the clock. The medical staff and physiotherapists at Gelenk Clinic will always answer all your questions. Generally, the length of hospital stay is 3 days. Your relatives can stay at a nearby hotel. Our staff will be happy to take care of your room reservation.
What should you pay attention to after surgical treatment of Morton's neuroma?
Immediately after surgery, the foot should be elevated. To avoid pain and swelling, apply a cooling compress to the foot. After about 10 days, the stitches are removed. After this you can take a shower again.
You also receive special shoes that take the load off the forefoot and transfer the body weight to the heel. If you are planning long walks, you should also take elbow crutches. Prevention of thrombosis during the impossibility of full weight bearing on the foot is necessary. This will prevent dangerous blood clots from forming. Physiotherapy and lymphatic drainage prevent muscle loss and swelling of the forefoot. The duration of forefoot swelling often depends on the age of the patient.
- Inpatient treatment: 2 days
- Recommended length of stay in the clinic: 5-6 days
- When can you fly home: 3 days after surgery
- When is it recommended to buy a return ticket: 5 days after surgical treatment
- When is it permissible to shower: after 10 days
- Length of stay on sick leave: 5 days
- When is it recommended to remove stitches: after 10 days
- Outpatient physical therapy
- When can you drive again: in 4-5 weeks
- Sports activity: at least 6 weeks after surgery
Herpes zoster and herpes-associated pain
Herpes zoster (HZ) is a sporadic disease that is the reactivation of a latent viral infection caused by the herpes virus type 3 (Varicella zoster virus (VZV)). The disease occurs with primary damage to the skin and nervous system.
VZV is the etiological agent of two clinical forms of the disease - primary infection (varicella) and its recurrence (herpes zoster). After a primary infection (chickenpox), usually in childhood or adolescence, the virus enters a latent state, localizing in the sensory ganglia of the spinal nerves. The commonality of the causative agent of chickenpox and herpes zoster was established even before the isolation of the virus using serological reactions in which liquid obtained from blisters on the skin of patients was used as an antigen. Later, using genomic hybridization, it was proven that in the acute period of herpes zoster, the detection rate of VZV is 70–80%, and in individuals without clinical manifestations, but with antibodies, viral DNA is detected in 5–30% of neurons and glial cells.
The prevalence of herpes zoster in different countries of the world ranges from 0.4 to 1.6 cases per 1000 patients/year in people under 20 years of age and from 4.5 to 11.8 cases per 1000 patients/year in older age groups. The lifetime risk of contracting herpes zoster is up to 20%. The main risk factor for its occurrence is a decrease in specific immunity to VZV, which occurs against the background of various immunosuppressive conditions.
Clinical picture of OH
The clinical picture of OH consists of skin manifestations and neurological disorders. Along with this, most patients experience general infectious symptoms: hyperthermia, enlarged regional lymph nodes, changes in the cerebrospinal fluid (in the form of lymphocytosis and monocytosis). Approximately 70–80% of patients with OH in the prodromal period complain of pain in the affected dermatome, which subsequently develops skin rashes. The prodromal period usually lasts 2–3 days, but often exceeds a week. Rashes with OH have a short erythematous phase, often completely absent, after which papules quickly appear. Within 1-2 days, these papules turn into vesicles, which continue to appear for 3-4 days - the vesicular form of herpes zoster. At this stage, elements of all types may be present on the skin. Elements tend to merge. Pustulation of vesicles begins a week or even earlier after the appearance of the first rash. After 3–5 days, erosions appear at the site of the vesicles and crusts form. If the period of appearance of new vesicles lasts more than one week, this indicates the possibility of an immunodeficiency state. The crusts usually disappear by the end of the 3rd or 4th week. However, peeling and hypo- or hyperpigmentation may remain for a long time after the resolution of OH.
Pain syndrome is the most painful manifestation of OH. While some patients experience rash and pain of relatively short duration, 10–20% of patients experience postherpetic neuralgia (PHN), which can last months or years, significantly reduces quality of life, causes great distress, can lead to loss of independence, and is associated with significant financial costs . Effective treatment of pain associated with OH is an important clinical goal.
Herpes-associated pain
According to modern concepts, pain syndrome in OH has three phases: acute, subacute and chronic. If in the acute phase the pain syndrome is mixed (inflammatory and neuropathic) in nature, then in the chronic phase it is typical neuropathic pain (Fig.). Each of the listed phases has its own treatment features, based on the pathogenetic mechanisms of pain and confirmed by controlled clinical studies.
Acute herpetic neuralgia
Pain in acute herpetic neuralgia usually occurs in the prodromal phase and lasts for 30 days - this is the time required for the rash to resolve. In most patients, the appearance of a rash is preceded by a burning sensation or itching in a specific dermatome, as well as pain, which can be stabbing, pulsating, shooting, paroxysmal or constant. In a number of patients, the pain syndrome is accompanied by general systemic inflammatory manifestations: fever, malaise, myalgia, headache. Determining the cause of pain at this stage is extremely difficult. Depending on its location, differential diagnosis should be made with angina pectoris, intercostal neuralgia, acute attack of cholecystitis, pancreatitis, appendicitis, pleurisy, intestinal colic, etc. The cause of the pain syndrome becomes obvious after the appearance of characteristic rashes. In typical cases, the prodromal period lasts 2–4 days, no more than a week. The interval between the onset of the prodrome and the onset of rash is the time required for reactivated VZV to replicate in the ganglion and be transported along the cutaneous nerve to nerve terminals at the dermoepidermal junction. The replication of the virus in the skin takes some more time, followed by the formation of inflammatory reactions. The immediate cause of prodromal pain is subclinical reactivation and replication of VZV in neural tissue. Experimental studies on animals have shown that at sites of VZV replication, the concentration of neuropeptide Y in nervous tissue, which is a marker of neuropathic pain, increases [1]. The presence of severe pain in the prodromal period increases the risk of more severe acute herpetic neuralgia and the likelihood of subsequently developing postherpetic neuralgia.
In most immunocompetent patients (60–90%), severe, acute pain accompanies the appearance of a skin rash. The severity of acute pain syndrome increases with age. Severe pain is also observed more often in women and in the presence of a prodrome. A characteristic feature of acute herpetic neuralgia is allodynia - pain caused by a non-painful stimulus, such as the touch of clothing. It is allodynia in the acute period that is a predictor of the occurrence of postherpetic neuralgia [2, 3]. The absence of allodynia, on the contrary, is a good prognostic sign and may suggest recovery within three months.
Subacute herpetic neuralgia
The subacute phase of herpetic neuralgia begins after the end of the acute phase and lasts until the onset of postherpetic neuralgia. In other words, this is pain that lasts more than 30 days from the beginning of the prodrome and ends no later than 120 days (Fig.). Subacute herpetic neuralgia can develop into postherpetic neuralgia. Factors predisposing to the continuation of pain include: older age, female gender, the presence of a prodrome, massive skin rashes, localization of rashes in the area of innervation of the trigeminal nerve (especially the eye area) or brachial plexus, severe acute pain, the presence of immunodeficiency [3, 4 ].
Postherpetic neuralgia
The International Herpes Treatment Forum defines PHN as pain lasting more than four months (120 days) after the onset of the prodrome. PHN, especially in older patients, can last for many months or years after the rash has healed. With PHN, three types of pain can be distinguished: 1) constant, deep, dull, pressing or burning pain; 2) spontaneous, periodic, stabbing, shooting, similar to an “electric shock”; 3) pain when dressing or lightly touching in 90%.
Pain syndrome is usually accompanied by sleep disturbances, loss of appetite and weight loss, chronic fatigue, and depression, which leads to social isolation of patients.
PHN is considered to be a typical neuropathic pain resulting from damage or dysfunction of the somatosensory system. Several mechanisms are involved in its pathogenesis.
- Nerve damage disrupts the transmission of pain signals, which leads to increased activity of higher order neurons (deafferentation hyperalgesia) [6–8].
- Nerve fibers damaged by VZV may generate spontaneous activity at the site of injury or other sites along the nerve (spontaneous ectopic activity of injured axons).
- Damage or inflammation of the nerve as a result of virus reactivation leads to a decrease in the threshold for activation of nociceptors, activation of urinary nociceptors—peripheral sensitization [5, 9].
- As a result of these changes in the peripheral parts of the somatosensory system, the activity of central nociceptive neurons increases and new connections are formed between them, provided that the pain continues—central sensitization [10–12]. The systems for recognizing pain and temperature stimuli are characterized by increased sensitivity to minor mechanical stimuli, causing severe pain (allodynia).
In most patients, pain associated with PHN improves within the first year. However, in some patients it can persist for years and even throughout the rest of their lives, causing considerable suffering. PHN has a significant negative impact on the quality of life and functional status of patients, who may develop anxiety and depression.
How to reduce the risk of PHN?
This issue is the most important for any doctor treating a patient with OH, and includes early initiation of etiotropic (antiviral) therapy and adequate pain relief in the acute stage.
Antiviral therapy. The results of many clinical studies have shown that the administration of antiviral drugs reduces the period of viral shedding and the formation of new lesions, accelerates the resolution of the rash and reduces the severity and duration of acute pain in patients with OH. Thus, in controlled studies using recommended dosages, the time to complete cessation of pain when prescribing famciclovir was 63 days, and when prescribing placebo - 119 days. Another study showed greater effectiveness of valacyclovir compared to acyclovir: pain syndrome when prescribed valacyclovir (Valavir) disappeared completely after 38 days, and when prescribed acyclovir after 51 days. Valacyclovir and famciclovir have similar effects on herpes-associated pain in immunocompetent patients [13, 23]. Thus, antiviral therapy is indicated not only for the rapid relief of skin manifestations, but also for the acute phase of the pain syndrome.
In all controlled clinical trials of antiviral therapy (
) it is recommended to start therapy within 72 hours of the onset of rash [1, 14].
The effectiveness of the anti-pain effect of antiviral therapy started at a later date has not been systematically studied, however, numerous clinical data suggest that late-started therapy can also affect the duration and severity of acute pain.
Antipain therapy. Effective relief of acute pain syndrome in OH is the most important stage in the prevention of PHN. It is advisable to stage-by-stage treatment of zoster-associated pain syndrome in all its phases. Thus, in the treatment of acute and subacute herpetic neuralgia, pain therapy consists of three main stages:
- Stage 1: Aspirin, paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs);
- Stage 2: opioid analgesics, including tramadol;
- Stage 3: drugs with a central analgesic effect (tricyclic antidepressants, anticonvulsants).
Considering that in our country there are known organizational difficulties in prescribing opioid analgesics, if simple analgesics and NSAIDs are insufficiently effective, it is necessary to move on to prescribing drugs with central action.
Treatment of postherpetic neuralgia
Currently, there are 5 main groups of medications: anticonvulsants, tricyclic antidepressants, lidocaine patch, capsaicin, opioid analgesics [21].
Anticonvulsants: Gabapentin and pregabalin are the two most commonly used anticonvulsants for the management of neuropathic pain associated with PHN. Drugs are more often used at the beginning of the development of PHN to reduce the acute component of neuropathic pain. In one study [15], in patients taking gabapentin, 43.2% had a decrease in pain perception, compared with 12.1% in the placebo group. In a similar trial [16], pregabalin also reduced the number of patients with PHN, especially in those aged 65 years and older. Gabapentin and pregabalin appear to be equally effective in reducing neuropathic pain [17]. Gabapentin is the drug of first choice for the treatment of any type of neuropathic pain; it is one of the most well-studied and widely used drugs in neurologist practice for the relief of pain in PHN. It is a structural analogue of gamma-aminobutyric acid (GABA). Gabapentin enhances the synthesis of GABA by stimulating the activity of glutamate decarboxylase; modulates the activity of NMDA receptors; blocks a-2-d-subunits of voltage-dependent calcium channels and inhibits the entry of Ca2+ into neurons; reduces monoamine release and sodium channel activity; reduces the synthesis and transport of the excitatory neurotransmitter glutamate; helps reduce the frequency of action potentials in peripheral nerves. The concentration of gabapentin in the blood plasma reaches its peak 2–3 hours after administration, the half-life is 5–7 hours. The dosing interval should not exceed 12 hours, bioavailability is 60%. Eating does not affect the pharmacokinetics of the drug; antacids reduce its concentration in the blood, so gabapentin should be taken no earlier than 2 hours after taking antacids. Excreted in breast milk; The effect of the drug on the child’s body has not been studied. Adverse reactions develop extremely rarely: slight dizziness, drowsiness. Gabapentin enhances the effect of lidocaine and antidepressants. You should refrain from combining it with alcohol, tranquilizers, antihistamines, barbiturates, sleeping pills, and drugs. The drug has important advantages in the treatment of neuropathic pain: safety, low potential for interaction with other drugs, good tolerability, and is not metabolized in the liver. Gabapentin is the drug of choice for the treatment of elderly people during polypharmacotherapy; it is convenient to use and has been proven to be highly effective.
Gabapentin dosage regimen. Initial dose: 1st day 300 mg in the evening; 2nd day 300 mg 2 times (day and evening); Day 3: 300 mg 3 times. Titration: days 4–6 300/300/600 mg; 7–10 days 300/600/600 mg; Days 11–14 600/600/600 mg. Daily therapeutic dose 1800–3600 mg, maintenance dose 600–1200 mg/day.
Pregabalin has a mechanism of action similar to gabapentin, but does not require slow titration and is therefore more convenient for clinical use. The drug is prescribed twice a day. The initial dose is 75 mg twice, the daily therapeutic dose is 300–600 mg. Several randomized clinical studies of the effectiveness of pregabalin in postherpetic neuralgia have been conducted, which showed the rapid development of an analgesic effect (during the first week of administration), good tolerability, ease of use and a reduction in sleep disturbances associated with pain [22].
Antidepressants. Drugs in this group, especially tricyclics (nortriptyline and amitriptyline), are important components in the treatment of pain in PHN. Due to the activation of descending serotonin and norepinephrine antinociceptive systems and the ability to block sodium channels, antidepressants block the perception of pain. In clinical trials of the effectiveness of tricyclic antidepressants in reducing pain in PHN, 47% to 67% of patients reported “moderate to excellent” pain relief, with equivalent effects reported for amitriptyline and nortriptyline [17]. However, nortriptyline does not cause many anticholinergic effects and may therefore be preferable to amitriptyline.
A patch with 5% lidocaine is applied to the affected area at the beginning of chronic pain or immediately after the diagnosis of PHN is made. The patch is applied to intact, dry, non-inflamed skin. It is not used on inflamed or damaged skin (i.e. during active herpetic eruptions). Lidocaine is an antagonist of sodium ion channels, the analgesic effect develops as a result of preventing the generation and conduction of neuronal activity potentials, by binding sodium channels of overactive and damaged nociceptors. A patch with 5% lidocaine has a local effect and has almost no systemic effects. Several studies have shown that the lidocaine patch reduces pain compared with placebo [18]. Comparative studies of the effectiveness of 5% lidocaine and pregabalin showed their equal effectiveness [19]. Capsaicin, which is made from red peppers and is an irritant, is used as an ointment or patch. When applied to the skin, it depletes peptidergic neurotransmitters (eg, substance P) in primary nociceptive afferents. The drug should be applied to the affected area 3-5 times a day to maintain a long-term effect. Despite the fact that a number of studies have shown the effectiveness of capsaicin against PHN, many patients often experienced significant adverse reactions: for example, a third of patients reported the development of an “unbearable” irritant effect of the drug, which significantly limits its clinical use in PHN.
Opioid analgesics (oxycodone, methadone, morphine) can also be used in the treatment of PHN. They reduce neuropathic pain by binding to opioid receptors in the central nervous system or inhibiting the reuptake of serotonin or norepinephrine at peripheral nerve endings - nerve synapses. According to research results, oxycodone, compared with placebo, provides greater pain relief and reduces the severity of allodynia, but causes the development of adverse reactions such as nausea, constipation, drowsiness, loss of appetite, and drug dependence [20]. Comparative studies of the effectiveness of opioids and tricyclic antidepressants have demonstrated their equivalent effectiveness.
In the section “Treatment of postherpetic neuralgia” in the 2009 European guidelines [21] for the treatment of neuropathic pain, first-line therapy is distinguished (drugs with proven effectiveness - class A): pregabalin, gabapentin, lidocaine 5%. Second-line drugs (class B): opioids, capsaicin.
When treating patients with PHN, it is advisable to follow certain steps.
Initially, first-line drugs are prescribed: gabapentin (pregabalin), or TCAs, or local anesthetics (plates with 5% lidocaine). If it is possible to achieve good pain reduction (VAS pain score – 3/10) with acceptable side effects, then treatment is continued. If pain relief is not sufficient, another first-line drug is added. If first-line drugs are ineffective, second-line drugs can be prescribed: tramadol or opioids, capsaicin, non-pharmacological therapy. In the complex therapy of postherpetic neuralgia, non-pharmacological therapy is also used: acupuncture, TENS anesthetic device, the most promising and effective method is neurostimulation.
Treatment of PHN is extremely challenging. Even with the use of various pain medications and referral to a specialist algologist, it is not always possible to achieve the disappearance of the pain syndrome.
Literature
- Dworkin RH Johnson RW, Breuer J., Gnann JW, Levin MJ Recommendation for management of herpes zostritis // Cln Infec Dis. 2007; 44: (Supl 1): S1–S26.
- Dworkin RH, Nagasako EV, Johson RW, Griffin DR Acute pain in herpes zoster: tue famciclovir database project // Pain. 2001; 94: 113–119.
- Hope-Simpson RE Postherpetic neuralgia // JR Coll Gen. Pract. 1975; 157:571–675.
- Choo P., Galil K., Donahue JG Walker et al. Risk factors for postherpetic neuralgia // Arch. Intern. Med. 1997; 157:1217–1224.
- Garry EM, Delaney A, Anderson HA et al. Varicella oster virus induces neuropathic changes in rat dorsal root ganglia and behavior reflex sensitization that is attenuated by gabapentin or sodium channel blocking drugs // Pain. 2005; 118:97–111.
- Yung BF, Johnson RW, Griffin DR, Dworkin RH Risk factors for postherpetic neuralgia in patients with herpes zoster // Neurology. 2004; 62:1545–1551.
- Jonson RW Zoster-associated pain: what is know, who is at risk and how can it be managed? // Herpes. 2001, 14 Supplement; 2:31A–34A.
- Tal. M., Bennett GJ Extra territoiral pain in rats with a peripheral mononeuropathy: mechano-hyperalgesia and mechano-allodenia in the territory of an uninjured nerve // Pain. 1994; 57:375–382.
- Oaklander AL The density of remaining nerve endings in human skin with and without postherpetic neuralgia after shingles // Pain. 2001; 92: 139–145.
- Rowbotham MC, Yosipovitch G., Connoly MK, Finlay D., Forde G., Fields HL Cutaneus innervation density in allodynic from postherpetic neuralgia // Neurobiol. Dis. 1996; 3:205–214.
- Rowbotham MC, Fields HL The relationship of pan, allodynia and thermal sensation in post-herpetic neuralgia // Brain. 1996; 119(Pt2):347–354.
- Scholz J., Broom DC, Youn DH, Mills CD, Kohno T. et al. Blocking caspase activity prevents transsynaptic neuronal apoptosis and the loss of inhibition in lamina 11 of dorsal horn afer peripheral nerve injury // J Neurosci. 205; 25:7317–7323.
- Tyring SK, Beutner KR, Tucker BA et al. Antiviral therapy for herpes zoster. Randomized, controlled clinical trial of vlacyclovir, and farmavir therapy in immunocompetent patients of 50 years and older // Arch Farm Med. 2000; 9:863–869.
- Gross G., Schofer H. et al. Herpes zoster guideline of German Dermatology Society (DDG) // J of Clinical Virology. 2003; 26:277–289.
- Rowbotham M., Harden N., Stacey B. et al. Gabapentin for the treatment of postherpetic neuralgia: a randomized controlled trial // JAMA. 1998. Vol. 280. P. 1837–1842.
- Dworkin R., Young J., Sharma U. et al. Pregabalin for the treatment of postherpetic neuralgia: a randomized, placebocontrolled trial // Neurology. 2003. Vol. 60. P. 1274–1283.
- Stankus S., Dlugopolski M., Packer D. Management of herpes zoster (shingles) and postherpetic neuralgia // Am Fam Physician. 2000. Vol. 61. P. 2437–2444.
- Karly P. Garnock-Jones, Gillin M. Keating/Lidocain 5% Medical Plaster. A review of its use in hjsterpetic neuralgia // Drugs. 2009; 69(15):2149–2165.
- Rehm S., Binder A., Baron R. Post-herpetic neuralgia: 5% lidocain medicated plaster? Pregadflin, or a combination both? A randomized, open/clinical effectiveness study // Cur. Med. Reas. 2010, v. 26, no. 7.
- Watson C., Babul N. Efficacy of oxycodone in neuropathic pain: a randomized trial in postherpetic neuralgia // Neurology. 1998. Vol. 50. P. 1837–1841.
- Attal N. et al. EFNS guidelines of the pharmacological treatment of neuropathic pain: 2009 revision // European Journal of Neurology. 2010.
- Seventer R., Feister H. et al. Efficacy and tolerance of twice-daily pregabalin for treating pain and related sleep interference in postherpetic neuralgia: a 13-week, randomized trial // Curr Med Res Opin. 2006; 22 (2): 375–384.
- Beutner KR et al. Valaciclovir compared with acyclovir from improved therapy for herpes zoster in immunocompetent adults // Antimicrobal agents and chemotherapy. 1995, July, vol. 37, no. 7, p. 1546–1553.
E. G. Filatova, Doctor of Medical Sciences, Professor First Moscow State Medical University named after. I. M. Sechenova, Moscow
Contact information about the author for correspondence
Table.
What is the cost of foot surgery?
In addition to the cost of surgical treatment for Morton's neuroma, it is worth considering the additional costs for diagnostics, doctor's appointments and aids (eg elbow crutches), amounting to approximately 1,500 to 2,00 euros. If you plan to undergo outpatient physical therapy treatment after surgery, we will be happy to provide you with an estimate of the costs. Information regarding the cost of hotel accommodation and possible additional treatment at a rehabilitation center can be found on the corresponding website.
Treatment of plantar nerve damage
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist. Symptomatic treatment is carried out (decongestants, analgesics). Physiotherapy, massage, novocaine and hydrocortisone blockades, orthopedic correction are indicated. Surgical intervention is required if conservative treatment is ineffective.
Essential drugs
There are contraindications. Specialist consultation is required.
- Tramadol (analgesic). Dosage regimen: IV, IM, SC in a single dose of 50-100 mg, possible repeated administration of the drug after 4-6 hours. The maximum daily dose is 400 mg.
- Voltaren (non-steroidal anti-inflammatory drug). Dosage regimen: IM at a dose of 75 mg (contents of 1 ampoule) 1 time/day.
- Ketoprofen (non-steroidal anti-inflammatory drug). Dosage regimen: IM: 100 mg 1-2 times a day; after pain relief, it is prescribed orally in a daily dose of 300 mg in 2-3 doses, a maintenance dose of 150-200 mg/day.
- Diacarb (diuretic). Dosage regimen: 0.25 g orally 2 times a day (morning, afternoon) for 5-7 days.
- Milgamma (B complex of vitamins). Dosage regimen: therapy begins with 2 ml intramuscularly 1 time per day for 5-10 days. Maintenance therapy - 2 ml IM two or three times a week.
How to make an appointment with a doctor and surgery for Morton's neuroma?
First of all, to determine the size of Morton's neuroma, as well as to diagnose possible other diseases, foot specialists in Germany will need current MRI images of the foot and X-ray results. Once we receive all the necessary documents, within 1-2 business days we will email you information for patients, as well as a preliminary cost estimate for treatment of Morton's neuroma.
Foreign patients can make an appointment for Morton's neuroma surgery in a short time. We will be happy to assist in obtaining a visa after the advance payment indicated in the estimate has been received into our account. If a visa is not issued, the amount received is returned to you in full.
Due to sometimes long flights, we try to keep the time between the first examination and surgery to a minimum. During outpatient and inpatient treatment of Morton's neuroma, you will be able to use the services of qualified medical personnel who speak several foreign languages (eg English, Russian, Spanish, Portuguese). Payment for a translator (for example, into Arabic) is carried out separately. We also organize transfers, we can book a hotel room, and we will tell you how to spend time in Germany for you and your relatives.
send a request
Risk group: who is “at risk”?
- You wear tight high-heeled shoes
- You have had transverse flatfoot for a long time
- Have you suffered a sports injury or sprain?
Tight high-heeled shoes with a narrow toe are the first associate of Morton's neuroma. In such shoes, the toes suffer from increased load and pressure from the shoe walls. And between the bones of the pressed fingers, inflammation of the nerve occurs.
The second “catalyst” for the appearance of Morton’s neuroma is advanced transverse flatfoot. If the transverse arch of the foot “sags,” its bones move apart, and the joints, on the contrary, “sag” and put pressure on the nerve.
Foot injuries after playing sports can also lead to neuroma. The bones and joints of a deformed foot assume a physiologically incorrect position and can compress the nerves between the third and fourth joints.