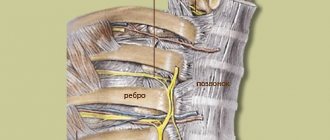
The concept of “intercostal neuralgia” is collective. It is used to denote a condition that is expressed by pain in the chest area. This pathology occurs due to changes occurring in the intercostal nerves.
Diagnosis and treatment of thoracic intercostal neuralgia is one of the areas of activity of the CELT Pain Clinic. If you suffer from this disease, contact us, and our doctors will develop an individual treatment plan that is sure to bring the desired relief.
Symptoms of intercostal neuralgia
The main symptom of the disease is excruciating pain in the chest, spreading along the nerve. Unpleasant sensations last for hours or even days, not leaving the person day or night. The pain can be acute, shooting or burning, the intensity is high or medium. It gets worse with coughing, sneezing and movement.
Sometimes the pain may resemble damage to the heart, stomach or spine. However, unlike intercostal neuralgia, cardiac pain goes away after taking nitroglycerin, and gastric pain goes away after antispasmodics.
Other signs of the disease:
- muscle tension;
- numbness of the affected area;
- tingling, sensation of goosebumps;
- sensitivity disorder;
- sleep disturbance;
- tearfulness;
- increased sweating.
The temperature with intercostal neuralgia may also rise. The skin in the outbreak turns red or white. If the cause of the disease is herpes zoster, characteristic rashes appear along the nerve.
Clinical manifestations
With intercostal neuralgia, pain can be concentrated in the right or left side of the chest. The pain may have a girdling nature and become stronger with a deep breath, coughing or turning the body. There are frequent cases in which pain symptoms lead to overstrain of the shoulder, shoulder blade or pectoral muscles. This is the reason for the increase in pain when trying to bend forward or move the arm.
Painful symptoms of intercostal neuralgia are also often accompanied by:
- projections of pain in the lumbar and dorsal region, as well as in the heart area;
- a burning sensation or numbness along the nerve trunk and its branches.
Pain can be felt in the area of the xiphoid process and be similar to pain with gastritis - such clinical manifestations are characteristic of pathologies of the nerves emerging from the 5th, 6th and 7th vertebrae. If they cover the nerves of the 10th, 11th, 12th vertebrae, the pain symptoms resemble those observed with appendicitis.
Cases in which the upper parts of the sternum are affected are characterized by the sensation of a foreign body behind the sternum and in the pharynx, which can cause swallowing problems.
At CELT you can get advice from a specialist algologist.
- Initial consultation – 4,000
- Initial consultation with the head of the Pain Clinic - 4,500
Make an appointment
Treatment of intercostal neuralgia
In case of severe pain, a person needs bed rest. It is necessary to limit mobility as much as possible to reduce pain.
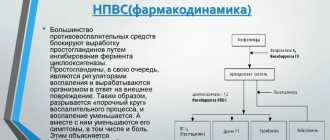
The disease is treated by a neurologist. The specialist prescribes drugs from the following groups:
- painkillers (analgin) in injections and tablets;
- novocaine and lidocaine blockades. Injections of these drugs along the nerves are also effective in relieving pain;
- anti-inflammatory drugs (Voltaren);
- muscle relaxants. Relieves pain caused by muscle spasm;
- B vitamins. Normal functioning of nervous tissue is restored.
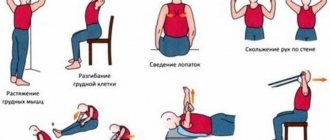
In the subacute stage, doctors recommend the following methods for treatment:
- UHF;
- electrophoresis with novocaine;
- laser therapy;
- magnetic therapy;
- acupuncture.
In complex therapy, the doctor also prescribes creams and ointments: painkillers, anti-inflammatory, warming.
Causes of intercostal neuralgia
The main causes of intercostal neuralgia are as follows:
- a number of diseases of the nervous system: multiple sclerosis, polyradiculoneuritis;
- diseases of the thoracic spine: deforming spondylosis, osteochondrosis, herniated disc, scoliosis;
- hypothermia of the body;
- intoxication of the body with alcohol, medications, salts of heavy metals;
- back and sternum injuries;
- weakening of the immune system;
- lungs' cancer.
Intercostal neuralgia of the chest during pregnancy
The main reasons for this condition in a pregnant woman are hormonal changes, an enlarging uterus and a large amount of fluid in the body. In some cases, the disease develops against the background of pinched nerve endings in the spine, poor posture and a lack of B vitamins. Intercostal neuralgia of the chest during pregnancy is manifested by a pain syndrome that intensifies with active movements. In addition, discomfort may appear in the area of the liver, spleen, stomach and shoulder blades.
Read also
Encopresis
Encopresis is a condition in which a person does not control or feel the urge to defecate, and also cannot control the act of defecation itself;
Fecal incontinence significantly worsens the patient’s quality of life,… Read more
Perinatal encephalopathy
Perinatal encephalopathy is a frequently encountered concept in the practice of pediatricians and pediatric neurologists! What it is? Literally, “perinatal encephalopathy” means “damage to the brain in the perinatal...
More details
Chiari malformation
What is Chiari Malformation? Chiari malformation (formerly Arnold-Chiari malformation) is a congenital defect of brain development that involves the dislocation of the cerebellar tonsils into the spinal canal through the large…
More details
Rehabilitation after stroke
It is very important to begin rehabilitation after a stroke as early as possible, since further recovery and the ability to avoid disability depend on this. For rehabilitation after a stroke in the clinic “First...
More details
Clubfoot
Clubfoot should not be understood as just one foot disorder. This is a group of deformities of the foot and ankle joint with their pathological setting. Clubfoot is a deformity in which...
More details
Diagnosis of intercostal neuralgia
Diagnosis of intercostal neuralgia is quite difficult, since it must be differentiated from a number of diseases that have similar symptoms. A cardiologist or pulmonologist may be involved in the diagnostic process. Specialists at the CELT Pain Clinic conduct an examination and collect anamnesis, and also determine the presence or absence of the disease in the following ways:
- chest x-ray;
- CT scan;
- myelography;
- Magnetic resonance imaging;
- spondylography;
- electro- and echocardiography;
- examination of the gastrointestinal tract.
If diagnostic studies do not reveal diseases of the lungs, gastrointestinal tract and cardiovascular system, the patient is referred to a neurologist who develops a treatment plan.
What is intercostal neuralgia?
Let's start with the fact that intercostal neuralgia is not a disease.
This is the name for pain that occurs when the intercostal nerves are exposed to various pathological factors, for example, herpetic infection, tumors, injuries, disc herniation, protrusion, osteochondrosis, etc. In other words, thoracic intercostal neuralgia can be called not all chest pain, but only that where intercostal nerves are involved. And this needs to be clearly understood so that the confusion that you often encounter at the everyday level does not arise when you hear people using the term intercostal neuralgia, but at the same time they mean a completely different pathology. By the way, even some doctors sometimes make the diagnosis of intercostal neuralgia erroneously, while in reality it most often turns out to be myofascial syndrome. Intercostal neuralgia, myalgia, myositis, myofascial syndrome, osteochondrosis, disc herniation, protrusion and many other terms are not synonymous. These are the names of specific pathologies that have their own characteristics and differences. And, since they are different, it means that the approach to them must also be different, otherwise there will be no sense in the treatment.
In general, the term intercostal neuralgia should not be used haphazardly, and it is not worth calling all pain in this area that way.
Temperature with vegetative-vascular dystonia
What to do if you feel a “temperature condition”, but without signs of a cold? You should take your temperature to see if there is any cause for concern.
What temperature is considered low-grade?
If it exceeds 37, then action should be taken, and if not, then it can be ignored. Most people's idea of elevated and normal temperature differs from the medical norm. A temperature several tenths higher than 37 degrees is considered low-grade and is a common symptom of VSD.
Should I be concerned if my temperature is slightly elevated?
The presence of elevated temperature cannot be left without attempts to find out the cause. If it does not exceed 37C, then this is considered normal, but if it is slightly higher than this figure, then it is considered low-grade. In “dystonics” it is a frequent occurrence and varies from 37.1 to 37.5C. Higher numbers indicate that this symptom is no longer related to the above disease.
Causes of elevated temperature during VSD
With VSD, temperature instability occurs, and the figure can change quite often during the day. The cause of this disorder is a deviation from the normal functioning of the thermoregulatory zone in the brain. Ensuring the same body temperature depends on it, that is, independent of external conditions. The failure occurs due to increased production of the hormone adrenaline, and there are frequent surges of its off-scale level, occurring due to little things that cause ordinary people to not have such amounts of this hormone. This is just one aspect of the pathologies of the autonomic system in VSD.
However, to more accurately identify the cause of this disease, you should undergo an examination and take tests that a specialist will prescribe. Based on their results, he will make a diagnosis, which will clarify the situation by confirming or denying the presence of other diseases that cause an increase in body temperature. If no such diseases were identified, then most likely the cause is vegetative-vascular dystonia.
Features of temperature during VSD
It should be borne in mind that this phenomenon in vegetative-vascular dystonia has its own distinctive features. One of them is her promotion, as some would say, because of all sorts of nonsense. For example, this could be physical activity, or even a state of rest. It is curious that it can return to normal if you just lie down or fall asleep, with a short rest being enough. Most likely, this is because in sleep it decreases a little for everyone.
Abnormal temperature with vegetative-vascular dystonia may not disappear for years. It usually appears in the morning and decreases at night. If it increases after any type of physical activity, then this indicates the presence of VSD. You should not overuse antipyretic drugs, as this does not eliminate the underlying cause, but it is quite possible to “earn” gastritis. At times it may fall below normal, but this is not a cause for concern as it will later rise to normal.
Is low-grade fever dangerous during VSD?
In general, no, but all these fluctuations are by no means healthy. This instability leads to two more violations. One of them is hyperhidrosis, that is, excessive sweating that occurs in a calm state, for no reason. The second consequence is that a person feels cold all the time, even in the warm season, not to mention the cold season. This is especially true for limbs, which get cold even with gloves and insulated shoes.
Is it possible to get rid of this trouble, which is one of the symptoms of vegetative-vascular dystonia?
In principle, there is no particular cause for concern. If this really bothers you, then you can take medications from time to time, but not antipyretics, but sedatives. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Occipital neuralgia
The article was prepared by a neurologist, the chief physician of our clinic, Pavel Dmitrievich Kovzelev. In this article, in addition to a description of occipital neuralgia and the principles of treatment, you can watch a video with a clinical case from our patient, as well as a video of how an occipital nerve block is performed - one of the most effective methods of treating this pathology.
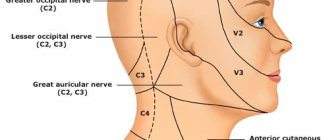
Anatomy of nerves.
The occipital nerves, 3 in number, are formed at the level of the 2-3 cervical vertebrae, then exit to the posterior surface of the spine and are located between the deep and superficial muscles of the neck.
At the level of the occipital bone, the nerves pierce the superficial muscles and exit under the skin, breaking up into small terminal branches that innervate the skin of the occipital region.
It's best to look at the picture.
Causes of neuralgia/neuropathy of the occipital nerve.
Why occipital neuralgia (also known as neuropathy) occurs is not completely clear.
The most popular hypothesis is that the nerve becomes trapped between the muscle and the fibrous tissue at the exit site and is pinched.
In people who have undergone surgery on the cervical/occipital region, people with Arnold-Chiari malformation, problems in the cervical spine, as well as those who have recently suffered a whiplash injury to the neck, NLDs are more common, which, in principle, fits into the “trap” hypothesis.
Symptoms of occipital neuralgia.
- The pain is severe, shooting, like electric shocks.
- Has a paroxysmal character: from several seconds to several minutes.
— The pain is localized in the back of the head, usually on one side and rarely on both sides.
- Between attacks, a dull, low-intensity pain may persist.
An attack can be provoked by touching certain points of the head, turning the head and any mechanical stimuli.
Sometimes patients note a decrease in sensitivity in these areas, and sometimes patients note dizziness and nausea.
IMPORTANT: Pain with occipital neuralgia can reach the fronto-ocular region through the connections of the occipital nerve with the trigeminal nerve at the level of the spinal cord.
The clinical picture may vary among patients. There are diagnostic criteria that I took from the 3rd International Classification of Headaches.
Let's look at them, but they are more important to me or your doctor.
- Unilateral or bilateral pain in the distribution of the greater, lesser and/or third occipital nerves and fulfillment of BD criteria
- Pain has at least two of the following three characteristics:
- repeated paroxysmal attacks lasting from several seconds to minutes
- heavy in intensity
- shooting, stabbing, or sharp pain
- Pain is associated with both of the following:
- dysesthesia and/or allodynia, manifested during painless stimulation of the scalp and/or hair (this is when normal touch is perceived as painful)
- one or both of the following: a) tenderness when pressing over the affected nerve branches
- b) trigger points at the origin of the greater occipital nerve or in the distribution of the C2 root.
- Pain is temporarily reduced by applying local anesthesia to the affected nerves. (i.e. when performing a blockade).
- Does not fit other diagnoses of the 3rd International Classification of Headaches.
Diagnosis of neuropathy of the occipital nerves. The diagnosis of NMN is made clinically (i.e., upon examination by a doctor), but for this it is necessary to exclude other causes. Taking into account the fact that many pathological processes in the posterior part of the brain and skull, as well as in the cervical spine, can produce similar pain in the occipital region, it is necessary to carry out:
- MRI of the brain
- MRI of the cervical spine, ultrasound examination of the vertebral arteries.
- In our clinic, ultrasound of the vessels of the head and neck is performed by a doctor with extensive experience, Irina Alekseevna Romadova, using an expert-level ultrasound device.
Treatment of neuralgia of the occipital nerves Treatment usually begins with a diagnostic blockade, which often gives a lasting positive result. I prefer to perform this block under ultrasound guidance for more precise and, more importantly, safe insertion. If necessary, the blockade can be repeated, but not more than once every three months. This is what it looks like schematically
This is how everything is visible with ultrasound navigation. I circled the nerve itself and its signature in red. It is very small, it literally looks like a dot. (Image clickable)
Drug therapy (standard drugs for neuropathic pain): gabapentin, tricyclic antidepressants, pregabalin, baclofen, carbamazepine.
of reflexology has proven itself well , which in this case is additional to stabilize and consolidate the effect.
If all of the above methods do not help, then you can: try botulinum toxin.
Also, one of my patients noted the effect of using Cefaly , a device for the treatment of migraines, which can be rented at our clinic to evaluate its effectiveness.
Summary : neuralgia of the occipital nerves is an uncommon, but extremely painful pathology. Sometimes people suffer for decades without a diagnosis or adequate treatment. At the same time, neuralgia has relatively clear diagnostic criteria and treatment approaches.
Preventive measures and treatment of neuralgia
Prevention is very simple - avoid hypothermia and colds. It is possible to use acupuncture and manual therapy. Acupuncture is carried out in several courses with a break of 2 months. Manual therapy affects the cervical and thoracic spine, relieving tension and pain. In case of exacerbation, the following is necessary: bed rest, taking sedatives, painkillers, therapeutic massage.
Symptoms of intercostal neuralgia and its treatment belong to the field of activity of a neurologist. SM-Clinic treats many diseases of the nervous system, of which osteochondrosis is only a small part.
Since often the symptoms of neurological diseases are actually signs of other diseases, the specialist will examine the entire body. If symptoms of intercostal neuralgia are detected, it is better to begin treatment immediately.