Indications for massage
- Massage is indicated for almost all types of neuralgia, manifested in the following symptoms.
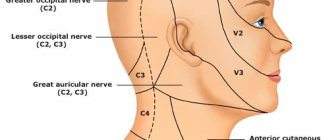
- Trigeminal neuralgia often occurs against the background of previous colds and inflammatory diseases or infections. It is expressed by repeated attacks of dull pain in the neck and head.
- Cutaneous neuralgia of the thigh is an unpleasant burning, stabbing pain or numbness in the outer thigh.
- Pterygopalatine neuralgia is constant severe pain in the area of the palate, temples, eyes or neck.
- Intercostal neuralgia - pain during sudden movements, coughing, sneezing.
- Occipital neuralgia is pain between the temples and the back of the head.
Massage technique
The massage is aimed at strengthening the facial muscles of the face, neck, shoulder girdle, eliminating swelling and stagnation in the nerve canal, improving blood and lymph circulation, excitability and nerve conductivity.
His main techniques include:
- soft vibrating movements in the cheek area;
- massaging the eyebrows, forehead, nasolabial triangle with fingertips;
- rubbing the neck, shoulders, arms;
- stroking the occipital region.
Movements should be without pressure; it is possible to use a vibration trainer. Facial massage for neuritis of the facial nerve is carried out in courses of 25 daily sessions lasting 2-5 minutes or 2 times a day for 15-20 minutes.
Before the procedure, you must wash and disinfect your hands. The patient should not feel pain; a change in skin tone indicates improper execution.
Massage movements are performed in different directions.
Forehead massage:
- Horizontal stroking of the forehead with the palm from the center to the sides (temples). Rubbing is done in the same direction with the fingertips.
- Vertical stroking with the palm from the eyebrows to the hairline, then massaging with fingers.
- Pressing your forehead with your fingers from the center to the sides. At the temples, press the entire length of your fingers.
- Repeat point 2.
- Vertical “tweezers”, horizontal “tweezers”: alternately lightly pinch the skin rolls between the thumb and forefinger.
- Repeat steps 1, 2.
- Vibration - tapping with fingertips.
- Repeat steps 1, 2.
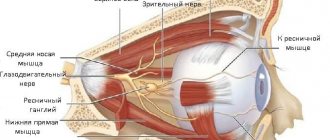
Eye socket massage:
- Move the third finger from the outer corner of the eye along the lower orbit to the inner one with the eyes closed. Movement of the middle finger in the inner corner with the second (index) on the eyebrow. Those. below - one finger, above - two.
- Trituration. With your index fingers pressed to the outer edge of the eyes, make pointed circular movements along the lower edge of the eye socket to the inner corner of the eye. The same is above the eyebrows.
- Repeat steps 1 and 2.
- Eyebrow tweezers.
- Stroking the eye sockets.
Features of massage for neuralgia
- In the first days of the disease, massage is carried out in a gentle manner with a gradual increase in load in each subsequent session. Carrying out a deep massage is allowed only after the acute symptoms have subsided and the attacks of pain have subsided.
- At elevated body temperatures, massage is contraindicated.
- The effectiveness of the massage increases if it is done immediately after taking a warm shower (bath) or visiting the bathhouse. Before the massage, it is advisable to apply a warming ointment or cream to painful areas.
- It is not recommended to go out into the cold immediately after the session.
How to relieve pain
The main method of treatment is medication. Drug therapy can be supplemented with traditional medicine. In especially severe cases, it is proposed to cure the pathology through surgery.
Medicines
Ibuprofen is a pain reliever for inflammation of the trigeminal nerve.
Medicines are prescribed to eliminate unpleasant symptoms and the root cause of the disease.
Anticonvulsants relieve acute pain and dull the sensitivity of the facial nerves to external irritations.
Antispasmodic drugs relax muscles, helping to relieve a secondary pain attack. As a rule, Baclofen is used in combination with anticonvulsants: Carbamazepine, Phenytoin, Lamotrigine, Gabapeptin. In some cases, drugs in this series have side effects: dizziness, diplopia, nausea and drowsiness.
The muscle relaxants Mydocalm, Sirdalud, Baklosan and the neuroprotectors Actovegin, Cerebrolysin, Neurox are used. B vitamins Benevron BF, Neuromultivit, Milgamma are used.
Surgical intervention
The operation involves eliminating compression of the nerve trunk by a blood vessel. In some cases, surgeons resort to destruction of the trigeminal nerve or its ganglion. Manipulation allows you to relieve pain.
Surgical methods of therapy are classified as minimally invasive. These include radiosurgery. The method is a bloodless intervention that does not involve incisions or sutures.
Trigeminal nerve pain relief at home
Traditional medicine offers many recipes that can relieve unpleasant symptoms. Healing tea has become widespread. Regular consumption of the drink can reduce or relieve pain.
- Lavender. Take 100 g of plant flowers and 150 g of St. John's wort. The ingredients are mixed and 500 ml of boiling water is poured. The mixture is infused for 30 minutes. Use 200 ml warm 2 times a day until the lumbago disappears completely.
- Chamomile. Take 1 tbsp. l. dried flowers. They are brewed with 250 ml of water. Before swallowing, hold the liquid in your mouth for a few seconds.
Pain can be relieved with compresses. The main condition is the regularity of their use and the combination of such treatment with medications.
- Alteiny. Take 4 tbsp. l. plant root. They are filled with 1 glass of boiling water. The mixture is infused for 12 hours. Cotton wool or gauze is moistened with the tincture and applied to the affected area. You can wrap your face in a wool scarf. Used regularly.
- Three-component. Includes chamomile, black elderberry and lilac flowers. The ingredients are mixed in equal proportions, 500 ml of water is poured in and boiled over low heat. The broth is filtered through cheesecloth. The cake is applied in a chintz bag.
- Bolotny. Take swamp duckweed. The grass is steamed and applied through the material to the temple area. The product helps eliminate swelling in the face area.
Geranium tincture has anti-inflammatory properties
To eliminate the inflammatory process, alcohol tinctures are often used. They have a quick effect
- Geranium. The leaves of the plant and the leaves of Kalanchoe are finely chopped in a 1:1 ratio. The resulting mixture is poured into a 500 ml jar and filled with alcohol. The mixture is infused for a week in a dark place. Painful areas on the face are lubricated with the tincture.
- Birch. Take 3 tbsp. l. birch buds. They are filled with 2 glasses of vodka and infused for 2 weeks. The mixture is used as a compress.
- Raspberry. Raspberry stems and leaves are mixed in equal proportions. The mixture is soaked with 1 glass of vodka. Infuses for 9 days. Taken for 3 months, 20-40 drops before meals.
Pathology can be treated with ointments. They also have an analgesic effect.
- Lilac. Lilac leaves are boiled until the water becomes richly colored. The broth is mixed with pork fat and cooled. The ointment is rubbed into painful areas. Stored in a dark and dry place.
- Ten days. The product eliminates pain within 10 days. Take 5 g of mumiyo. The tablet dissolves in water to a pasty state. The gruel is mixed with 70 g of pork fat. Apply to the gum area closer to the cheek once a day.
From the editor: Stages of depressive states
Treatment of the trigeminal nerve is carried out comprehensively. Home therapy complements medications.
Massage techniques and methods
Techniques and methods of therapeutic massage are prescribed depending on the diagnosis made by the doctor.
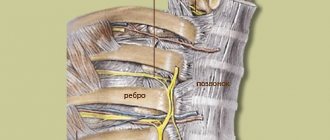
Intercostal neuralgia
The patient lies on his back. At the beginning of the session, it is necessary to warm up the body - the massage therapist strokes the back with normal movements. Then more sharp stroking and kneading of the back is done from the upper to the lower part with a gradual transition to the sore areas. The latissimus dorsi muscle is affected by alternately stroking and kneading.
Massaging the ribs is carried out both on the back and in the chest area, the schemes are similar: gentle rubbing, stroking, squeezing. In order to thoroughly massage all the muscles and intercostal cavities, the massage therapist works with the pads of his fingers, directing them straight, in a circle or in a zigzag.
Chest massage includes the following techniques: rubbing, stroking, squeezing and pressing. At the end of the session, they again move on to massaging the latissimus muscle on the back using stroking, squeezing, kneading, and shaking methods.
Trigeminal neuralgia
The massage begins with alternate rubbing and stroking on the collar area, especially carefully massaging the back of the head, where many nerve endings are located. Next, proceed to facial massage. The scheme is as follows: stroking, rubbing in a circle, light kneading, vibration effects on areas with complete or partial loss of sensitivity.
Occipital neuralgia
Massage prescribed for the treatment of occipital neuralgia helps reduce pain and stop inflammation. The sequence of massage: back, neck, back of the head.
- Back. Techniques: stroking, squeezing, circular kneading of the longitudinal muscles, direct and circular kneading of the muscles located between the spine and shoulder blades.
- Neck and trapezius muscle. Techniques: stroking, squeezing, regular kneading, circular kneading with fingertips, kneading with phalanges.
- Back of the head. Techniques: regular and rake-like stroking, squeezing, straight, circular, zigzag rubbing with the pads or phalanges of four fingers.
Massage in the treatment of neuritis of the facial nerve
Today there are several methods for treating neuropathy, which makes it possible to choose the optimal regimen for each patient. The specialist prescribes medications to the patient and also prescribes a course of massage, which significantly speeds up the healing process. Some people resort to biofeedback treatment, although this method of therapy does not show noticeable results.
How effective?
Restoring the function of facial muscles during neuralgia takes time. Typically, massage is performed by a specialist - it is prescribed for a course of 20-25 days, but it is useful to do the procedure at home. Often, the therapeutic effect of self-massage becomes noticeable with daily therapy for at least 10 weeks.
- spasm relief;
- restoration of the function of facial muscles;
- improving blood circulation;
- elimination of speech defects that were caused by the disease.
Massage technique
Massage for neuritis of the facial nerve can be started 5-7 days after the first symptoms of the disease appear.
It is worth remembering that treatment will not be limited to a few sessions - health-improving exercises must be repeated regularly, following the doctor’s instructions. Before the procedure, you should wash and disinfect your hands. Therapy requires the use of several techniques:
- continuous stroking with the whole palm;
- point pressure and kneading;
- vibration and rubbing.
Massage technique for facial nerve neuropathy:
- First you need to develop the neck muscles. The patient tilts his head and makes circular movements clockwise/counterclockwise. Mini-charging is performed at a slow pace. After this, you can begin the procedure by kneading the neck and back of the head.
- The next stage is massaging the areas of the eye sockets with the eyes open and then with the eyes closed. Gradually it is necessary to move from the tear duct to the outer corner of the eye. Point the eyeballs down and hold the eyelid of the affected eye with your other hand. Use your fingertips to rub the area of your eyebrows and forehead.
- A thorough study of the nose area is performed. Using light pressing movements, you gradually need to move from the wings of the nose to the earlobes.
- The patient needs to massage the muscles around the mouth, and then gradually move to the cheekbones. Using vibration with your fingers in the cheek area will be effective.
- Using massaging movements, you need to smoothly move from the middle of the chin to the tops of the cheekbones.
- The final stage is kneading the front surface of the neck.
The patient should try to smile, articulate, and strain different muscles to make them move equally on both sides. Therapeutic exercises help restore blood flow, train facial expressions and help maintain normal muscle tone. To limit the range of motion, the healthy half of the face should be held with the palm of your hand.
The exercise therapy complex consists of simple exercises:
- Raise your eyebrows, depicting the emotion of surprise. Frown, trying to lower your eyebrows as low as possible.
- Wrinkle your forehead, performing a symmetrical movement. If folds do not form on the affected side, you need to help with your hands.
- Close your eyes and in this position “look” at 4 sides. Squint your eyes as hard as possible for a few seconds, and then relax. Movements should be slow.
- Flare your nostrils, then place your fingers on the wings of your nose. While continuing to breathe, you should try to provide resistance to your fingers.
- Close your lips and try to lift your upper lip, and then lower your lower lip so that your teeth show. Stretch your smile as wide as possible.
- Close your mouth and suck in your cheeks, and then inflate them as much as possible. Curl your tongue and breathe for a few minutes.
- Close your lips tightly and try to count the teeth on both jaws with your tongue, pushing it between the teeth and cheek muscles.
- Move your jaw, moving it down, inward and moving it to the sides.
Clinical manifestations
Sciatica at any age manifests itself with pain and neurological disorders. Each symptom has its own characteristics, which depend on the course of the pathology, concomitant diseases and the correctness of therapy.
Pain syndrome
The main complaint is pain. Sciatica, both in women and men, cannot occur without pain. The pain syndrome manifests itself acutely and sharply. The patient characterizes it as a blow with a knife or electric shock.
The pain is localized along the back of the thigh, in the popliteal fossa or on the lower leg. It can completely cover the specified areas or have a limited distribution. The severity of sensations varies - from minor discomfort to paralyzing attacks. In the same patient, the intensity of pain changes as the pathology progresses and the treatment is performed.
The pain syndrome can be temporary or permanent. Episodic seizures are most common. They occur during physical exertion, sudden movements of the body and legs, after hypothermia, etc. Symptoms have one-sided localization. Chronic disorders are mild; as a rule, they are discomfort and rare pain that occurs during physical activity. Exacerbations with a sharp increase in symptoms are possible. The pain may radiate to the lower back and front of the legs.
Neurological symptoms
Compression of the nerve fiber leads to neurological manifestations: impaired skin sensitivity, decreased muscle strength, etc. The severity of symptoms varies greatly in individual patients. The most common signs of sciatica are:
- Decreased skin sensitivity in the buttocks, back of the thigh, popliteal fossa and back of the lower leg. In some cases, the patient feels numbness in the toes on the affected side.
- Autonomic disorders. Thermoregulation is disrupted - a person’s feet are cold, even in the warm season. Sometimes there is increased sweating. Insufficient blood circulation in the lower extremities leads to the skin becoming pale and peeling in the area of innervation of the affected nerve.
- Motor disorders, namely, decreased muscle strength along the back of the thigh, lower leg and foot. The patient's step range on the affected side decreases, and the range of motion in the knee and ankle joint decreases. In the absence of treatment, the gait becomes “shuffling”, since it is difficult to raise the foot high when walking.
Sciatica: causes and symptoms
During the chronic period, symptoms are mild. The patient may experience slight discomfort and weakness in the leg with active movements. Exacerbations of the disease occur after hypothermia of the lower back, against the background of acute infections, severe stress, etc.
Treatment of post-traumatic sensory neuropathy
The most problematic result of dental surgery, local anesthesia or endodontic treatment is damage to the trigeminal nerve with subsequent dysfunction, most often of the inferior alveolar (IAN) and/or lingual nerve (LN). Altered sensations and pain in the orofacial area associated with damage to the branches of the trigeminal nerve can interfere with pronouncing sounds, eating and drinking, kissing, shaving, applying makeup, brushing teeth, and even working and sleeping.
Treatment of post-traumatic sensory neuropathy depends primarily on the causes and mechanisms of nerve damage and, most importantly, on the time after injury until treatment begins.
The trigeminal nerve is the largest peripheral sensory nerve in the human body, which is represented by more than 40% of the sensory cortex, so making the only correct decision about therapeutic tactics for a clinician after its injury is always a difficult task.
The most commonly iatrogenically injured branches of the trigeminal nerve are the inferior alveolar nerve (IAN) and the lingual nerve (LN).
The lingual nerve is located freely in the soft tissues, so the main causes of its damage are the removal of third molars and local anesthesia.
The inferior alveolar nerve is located in the bony canal of the mandible and the main causes of its damage include implantation, apical infection, endodontic treatment, and periapical surgery.
Rice. 1. Morphological preparation of the lower third of the face demonstrating the prepared lingual nerve, which runs deep in the soft tissues and is adjacent to the lingual surface of the mandible in the retromolar region.
Rice. 2. Schematic representation of the course of the lingual and inferior alveolar nerve.
After iatrogenic damage to the trigeminal nerve, the patient experiences not only impaired sensory function, but also a decrease in quality of life, psychological discomfort and social problems, the manifestation of which is more persistent in cases where the patient is older, and the time from the day of injury until the doctor recognizes the damage and makes therapeutic decisions more than 48 hours. It is also important to remember that post-traumatic consequences are more severe the more proximal the injury is to the cell body.
It is almost always difficult for patients to accept and cope with these negative consequences of oral and maxillofacial surgery, since third molar extraction or implantation is often an optional procedure, and the patient, choosing in favor of such surgical treatment, expects significant functional and/or aesthetic improvements.
There is still no consensus on treatment protocols for such injuries, but there is a clear understanding that the management and success of treatment of sensorineural deficits will be influenced by the mechanism and duration of nerve injury, injury-related clinical signs and symptoms, including psychological, functional or pain-related complaints of patients .
A recent Cochrane systematic review of treatment options for post-traumatic neuropathy resulting from dental procedures concluded that there is still a need for randomized controlled clinical trials to examine the effectiveness of surgical, medical and psychological treatments for iatrogenic injuries of the inferior alveolar and lingual nerves.
Coulthard P, Kushnerev E, Yates JM, Walsh T, Patel N, Bailey E, Renton TF. Interventions for iatrogenic inferior alveolar and lingual nerve injury. Cochrane Database Syst Rev 2014 Apr 16;(4):CD005293.
The priority when managing these patients is to have an honest conversation with the doctor about whether the nerve damage is permanent or temporary. This will help the patient make responsible decisions about surgical treatment, but pain control and rehabilitation should be started as early as possible, taking into account the psychological problems associated with iatrogenesis of the injury.
There is a false belief that most trigeminal nerve injuries recover, when in fact, for example, lingual nerve injuries associated with the creation of a lingual surgical approach are restored after 10 weeks and in only 88% of cases.
Folk remedies
To relieve painful symptoms, there are proven self-medication methods:
- Black radish juice is mixed with lavender oil.
Proportions: per spoon of juice - two drops of oil. Rub the mixture over the location of the nerve. To enhance the heating, apply a woolen bandage. Use the product up to 6 times a day, for 3 days. - A boiled hot egg is peeled, cut in half and each half is applied to the affected area on the face.
- Hot salt is poured into a bag and the inflamed area is warmed up. The method relieves pain well.
- Fresh geranium leaves are applied and fixed with a bandage on the painful area. Carry out the procedure for 3-4 hours, up to two times a day.
- Aloe is good at treating inflammation. Juice, immediately after squeezing, take a teaspoon, before meals, 3-4 days.
- A compress made from marshmallow roots is considered an effective method of relieving pain. Place the crushed roots in 200 ml of boiling water and let it brew for a day. Soak a clean cloth in warm infusion and apply to the sore spot. Cover the compress with a towel and leave for an hour. After removing the lotion, wrap your face again.
- An infusion of chamomile flowers will help with neuralgia in the jaw area. Pour a teaspoon of chamomile into a glass of boiling water and let cool to room temperature. Rinse your mouth up to five times a day.
All of these remedies are suitable for home treatment, but provide only temporary relief. To eliminate the cause of inflammation, you need to consult a doctor, only he will give recommendations for effective therapy.
NTN is a fairly common disease. When treating it, you need to eliminate the cause - this is the only way to get rid of painful attacks
It is important not to delay your visit to the doctor, and then you have every chance of defeating the insidious disease
From the editor: Is epilepsy inherited?