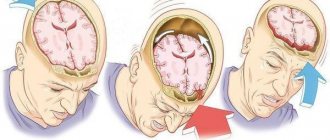
A disruption of the normal functioning of the brain, which occurs after a mechanical injury to the skull and is not based on vascular pathologies, is called a concussion. A similar disorder occurs in 60-70% of people who have suffered a head injury in one way or another.
A concussion falls into the category of mild types of TBI (damage to the cranial bones and/or soft tissues, called traumatic brain injury), the most common type in medical practice. It is characterized by the development of general cerebral and/or unstable focal neurological symptoms, which usually pass rather quickly.
There is injury, no symptoms
How can you tell if you have a TBI if you haven’t lost consciousness?
Alexander Borovsky:
— As for injuries in adults (it’s different with children), if a person hits his head so hard that he gets a TBI, he usually loses consciousness. He may not even notice that he has “passed out.” If a person loses consciousness even for a few seconds and/or has nausea and vomiting, with the presence of a head injury, this is a sign of at least a mild TBI. Regardless of the severity, patients with such injuries should be observed in a hospital. Why is it important? Due to possible delayed deterioration of the patient's condition.
The period of imaginary well-being, before the development of secondary symptoms, is called the light interval. A vessel in the head is torn or a small fracture occurs that is not felt, there is no external damage. This is likely if, for example, the victim was wearing a helmet or hat at the time of the accident. Bleeding leads to the formation of an intracranial hematoma and can cause delayed compression of the brain. In this case, the person loses consciousness not from the concussion, but from compression and dislocation of the brain. Here a person will no longer regain consciousness without outside help. If they manage to get him to the hospital and undergo surgery, he will be lucky.
If you still don’t go to the hospital, will such injuries make themselves known in the future?
— The consequences of severe TBI can be compared with the consequences of a stroke. Severe TBI often results in neurological impairment. To regain lost functions, patients will need long-term rehabilitation.
Timely treatment of moderate TBI helps to restore lost functions within a month. Ignoring symptoms can lead to disability.
A single mild traumatic brain injury goes away without consequences after an average of a week, but repeated concussions are dangerous. This is especially true for boxers, because a knockout is at least a concussion. Athletes endure quite a lot of them during their lives. Gradually accumulating, brain damage ultimately leads to dementia, which manifests itself clinically in the form of absent-mindedness and focal neurological symptoms. When we hospitalize a patient with a mild TBI, he is not so much treated as he is monitored so that the minor injury does not develop into a severe one. And for recovery, by and large, only psycho-emotional peace and sometimes painkillers are needed.
Treatment of TBI and consequences of brain injuries
In the acute period, decongestant, neurometabolic, neuroprotective, symptomatic therapy is carried out, which consists of selecting several medications offered both in the form of tablets and in the form of injections (drip and intramuscular).
This treatment is carried out for about a month. After which the patient remains under the supervision of his attending physician, depending on the severity of the TBI, from six months to several years.
For at least three months after a TBI, drinking alcoholic beverages and strenuous physical activity is strictly prohibited.
In addition to traditional methods of treating TBI, there are no less effective methods:
- acupuncture,
- osteopathy.
In combination with drug therapy and physiotherapy, these techniques can have a more pronounced and faster effect. However, in some cases they are contraindicated for use.
Everyone knows the fact that treatment must be comprehensive, and the more techniques are used during treatment, the better.
After completing the course of treatment, the patient must be under the supervision of a doctor, and subsequently he may need repeated courses, usually once every six months.
Chronic hematoma in the elderly
Any bruising gradually disappears as the hematoma resolves. Why does an acute hematoma in the cranial cavity sometimes become chronic?
Alexander Borovsky:
— Chronic hematoma can be a consequence of traumatic brain injury, this is more common in older people. For example, a person slightly hit his head and forgot about this incident. After 10-14 days, the hematoma becomes chronic.
In older people, over the years, the volume of the brain becomes less than the intracranial volume, and many free cerebrospinal fluid spaces appear. After injury, minor bleeding does not lead to compression of the brain, so an asymptomatic course is possible. Over time, the blood breaks down into its components. Fibrin, which is contained in the blood, falls out, forming a capsule around the hematoma. The capsule works like a semi-permeable membrane, then red blood cells are destroyed and large protein molecules are released. Along an osmotic gradient, water from the surrounding tissues begins to flow into the hematoma cavity.
Another danger is an increase in the volume of the hematoma due to new hemorrhages from the newly formed vessels of the capsule. When it grows strongly (2-3 cm thick and can be more than 300 ml in volume), symptoms arise, for example, a headache appears, an arm or leg fails, speech and consciousness are impaired.
By the way, there are other factors that contribute to the formation of chronic hematomas: taking anticoagulants, vascular diseases, etc.
Periods, consequences and complications of TBI
The so-called traumatic disease includes three periods:
- Acute (duration 2 weeks – 2.5 months) – development of defense reactions to a damaging factor.
- Intermediate (duration 6 months – 1 year) – the process of lysis and repair in damaged areas.
- Long-term or final (duration 2-3 years, with complications - until the end of life) - completion of tissue degeneration and restoration of functions.
Complications of TBI in the acute phase:
- Impaired function of the respiratory system (respiratory depression and gas exchange disorders).
- Problems with central and regional (cerebral) circulation.
- Hemorrhagic complications (cerebral infarction, intracranial hemorrhage).
- Dislocation (displacement) of brain parts.
- Complications of a purulent-inflammatory nature: intracranial (abscesses, osteomyelitis, meningitis, encephalitis), extracranial (pneumonia, for example).
Possible consequences of TBI:
- Paralysis of the limbs (partial, complete) on one or both sides.
- Loss of vision, hearing, ability to speak, swallow, and breathe.
- Loss (weakening) of control over the function of the pelvic organs (the patient is not able to control the processes of urination and defecation).
- Tremor (shaking) in the limbs.
- Partial memory loss, deterioration of attention, changes in character and other consequences associated with higher nervous activity (usually after a coma).
In the long-term post-traumatic period, the development of epilepsy (acquired epilepsy), occlusive hydrocephalus, neuroses, and parkinsonism is possible. Also, cases of arachnoiditis and arachnoencephalitis (a disease of the central nervous system - serous (non-purulent) inflammation of the arachnoid membrane of the brain or spinal cord) are not uncommon.
TBI in children has its own characteristics
Today in Minsk, children’s traumatic brain injuries are dealt with by specialists from the Republican Scientific Research Center of Neurology and Neurosurgery; until 2010, young patients were also admitted to the Emergency Hospital, which had a children’s neurosurgical department.
The reaction of a child’s body to injury differs from the reaction of an adult due to the anatomical and physiological characteristics of the brain and skull in childhood. Clinical manifestations of TBI are sometimes subtle.
Very young children cannot complain about where it hurts or describe symptoms, so it is difficult to collect an anamnesis. Doctors can only rely on the mother or other witnesses to the injury. If a child under the age of one year has a head injury, even if he fell from a small height and the mother thought the blow was insignificant, the child must be seen by a doctor. Children under 3 years of age are hospitalized together with their mother.
Some people mistakenly believe that children are more susceptible to TBI because of their immature skull, which has not yet ossified. This is wrong. Babies' brains are very hydrophilic, sensitive to shock, bruises and concussions. The fontanel and unformed bone sutures in no way protect against increased intracranial pressure during injury.
Parents need to pay attention to the following symptoms after a head injury: changes in behavior (become lethargic, drowsy, strange), nausea, vomiting, headache, dizziness, convulsions, especially bleeding or discharge of clear fluid from the ear or nose, bruises under the eyes. Symptoms may occur immediately or within 24 hours.
Notice when the baby cried: immediately or some time after the fall. If you did not see the moment of injury with your own eyes, you may have missed the time of loss of consciousness and may not even be aware of the TBI. It is important to monitor the child’s appetite and activity after an injury. Any of the above symptoms is a reason to immediately consult a doctor.
Treatment of brain injuries
Each type of brain injury requires a specific type of treatment, and the treatment options are quite complex and varied. The decision on the type of treatment is made by several doctors and only with the consent of the patient or his representative.
The positive outcome of treatment is influenced by the disease recognition factor. If the disease is detected at an early stage, treatment will be successful. Otherwise, special treatment regimens may be required. As a rule, doctors use complex methods to treat patients with brain lesions.
Where to go if you have a TBI
If there is a wound on the head, you need to contact a surgeon to stitch it up, and he should already determine whether a CT scan and consultation with a neurosurgeon are necessary. If there is no wound, but you are worried about vomiting or other symptoms of a traumatic brain injury, we turn to a neurosurgeon, or in regional hospitals to a neurologist, traumatologist or surgeon.
According to instruction No. 1110 on the procedure for organizing the provision of medical care to patients with traumatic brain injury, such care is provided in stages: at the pre-hospital stage; in the emergency department of hospital healthcare organizations; in specialized neurosurgical departments of regional, city and interdistrict hospitals, in surgical and trauma departments with assigned beds for the treatment of patients with TBI in regional, city, interdistrict and district hospitals; in intensive care wards and anesthesiology and intensive care departments of regional, city, interdistrict and district hospitals.
All patients with mild TBI should be hospitalized. If it is not possible to do a CT scan, it is necessary to observe them in a hospital for at least 5 days.
Computed tomography of the brain is the main method for studying patients with TBI. It allows you to identify intracranial hematomas and hemorrhagic stroke, exclude a tumor or, for example, an ischemic stroke.
What if the victim refuses hospitalization?
Alexander Borovsky:
— A patient’s refusal to hospitalize for a brain injury has no legal force. The victim may be in an inadequate state, unable to make the right decision, and not understand the full danger of refusing hospitalization for his health. And the doctor has no right to force him to hospitalization if the patient is conscious and refuses medical care. We do not force hospitalization. We are trying to explain as clearly as possible what threatens him. Perhaps through relatives. If the patient leaves without permission, we transfer the asset to the clinic at the place of residence, and sometimes we turn to the police for help.
When is a patient with a TBI brought to the hospital reported to law enforcement?
If there is a suspicion of a criminal nature of the injury, it is mandatory to report to law enforcement agencies. If the patient arrives unconscious and it is impossible to find out the circumstances under which the injury was sustained, a report is also sent to the police. We report patients injured in road accidents to the traffic police.
Mental disorders in traumatic brain injury
1. Impaired consciousness
Traumatic brain injury (TBI) in Russia is registered annually in four out of 1 thousand people. The most common types of injuries are domestic, criminal and road traffic injuries. Based on the nature of brain damage, focal, diffuse and combined forms of TBI are distinguished. By severity - mild (concussion and mild contusion of the brain - 83% of all TBIs), moderately severe (moderate contusion of the brain - 8-10% of all TBIs) and severe (severe contusion and compression of the brain - 11% of all TBIs). There are acute, intermediate and long-term periods of the course of a traumatic disease. Mental disorders are observed in almost all cases of TBI, and these disorders are very diverse.
In the acute period of TBI, the main disorders are syndromes of depression of consciousness: moderate and deep stupor, stupor and coma.
| | Often, symptoms of various mental disorders, such as schizophrenia, also appear with TBI. That is why comprehensive diagnostics is necessary to make a diagnosis. |
Moderate stupor is the mildest depression of consciousness, slowing of movements and speech, lengthening of pauses between the doctor’s questions and the patient’s answers are detected. Reduced active as well as passive attention. The answers to the questions are incomplete, inaccurate, errors regarding orientation in place and time are possible. The face is inexpressive, the gestures are depressed. This condition appears immediately after a mild TBI. Partial congrade amnesia is possible. Fluctuations in clarity of consciousness are characteristic. Synonym: nullification.
Profound stupor or somnolence. It is characterized by increasing drowsiness, lethargy, slowing of speech, movements, and loss of expressive acts (and emotions) after TBI. Contact with the patient is still possible, but you have to repeat questions or bother the victim to get his attention. The answers do not follow immediately and are often limited to the words “yes” or “no.” It turns out that the patient is disoriented in place and time, inaccurately oriented in the environment, but correctly oriented in his own personality and in the situation. The response to pain is preserved, the patient can show where he feels it. Control over the functions of the pelvic organs is weakened. Congrade amnesia is such that the patient remembers very little of what happened and was perceived by him during the period of deafness, which lasts up to 20–30 minutes or more. The recovery from stupor is gradual, with fluctuations in the clarity of consciousness.
Stupor is a depression of consciousness in which verbal contact with the patient is completely interrupted, he does not understand the questions addressed to him and does not answer them. The patient still reacts to a loud sound, painful stimulation, opens his eyes, responds with a grimace of pain, reaches his hand to the place of pain. Elementary recognition is preserved: at the sound of a loved one’s voice, the patient’s heartbeat quickens and the face turns red. Muscle tone is reduced. There are no skin reflexes. Corneal, pupillary and conjunctival reflexes are preserved, tendon and periosteal reflexes are quite lively. Left to himself, the patient lies silently, with his eyes closed, without moving or making simple automated movements. Stupor occurs with a TBI approaching moderate severity and can last tens of minutes. The emergence into clear consciousness is gradual, bypassing the state of stunning. Congrade amnesia is complete.
Coma is a state of complete shutdown of consciousness and mental activity, from which it is impossible to remove the patient. Congrade amnesia is total. There are three degrees of coma. Moderate coma (I degree coma) is manifested by the fact that the reaction to pain is preserved. This is a reaction in the form of defensive movements of flexion, extension of the limbs or uncoordinated dystonia. Difficulty swallowing. Pupillary and corneal reflexes are preserved, abdominal reflexes are absent, tendon and periosteal reflexes are variable, respiratory and cardiovascular disturbances are insignificant. Deep coma (II degree coma) is characterized by an absolute loss of reactions to any external stimuli and inhibition of most reflexes. Pathological reflexes are evoked and meningeal symptoms appear.
There is no swallowing. Weak pulse, arrhythmia, decreased blood pressure. Breathing is impaired, control of the functions of the pelvic organs is lost, disturbances in muscle tone vary from diffuse atony to hormetonia. Mydriasis may be one-sided. Terminal coma (coma III degree) is manifested by severe disturbances of spinal, bulbar and cortical-subcortical functions. Breathing is severely impaired to the point of apnea. Severe tachycardia. Blood pressure is at a critical level or cannot be determined. Diffuse muscle atony, bilateral fixed mydriasis.
Coming out of a coma occurs in the reverse order, and it can stop indefinitely at different stages. To monitor recovery from coma, a scale of stages of this process is recommended (Dobrokhotova et al., 1985; Zaitsev, 1993). The coma state is defined as the first stage. The second stage is eye opening, or vegetative status. The third stage is gaze fixation and tracking, i.e. akinetic mutism. The fourth stage is discrimination between loved ones, i.e. akinetic mutism with emotional reactions. The fifth stage is understanding speech and following instructions, i.e. mutism with understanding speech.
The sixth stage is the restoration of one’s own speech activity, i.e., the syndrome of reintegration of long-absent speech. The seventh stage is the restoration of verbal communication, i.e. amnestic confusion. The eighth stage is mnestic-intellectual deficiency syndrome. The ninth stage is psychopath-like syndromes. The tenth stage is neurosis-like disorders. This scale, with certain reservations, can be used as a basis for describing other mental disorders in TBI (excluding stunned consciousness).
2. Vegetative status
This stage, as well as the next one - akinetic mutism, often represent reversible post-comatose states, even if they last up to 10 years or more. Reversible vegetative status is a state of relative stabilization of viscerovegetative functions, beginning after coma from the moment of the first opening of the eyes and ending with gaze tracking. It was first described by E. Kretschmer (1940) under the name “apallic syndrome”. The reverse development of the vegetative status occurs in stages. The stage of scattered reactions is distinguished by short periods of wakefulness when the patient lies with his eyes open.
More often he does this during the day. The eyeballs are motionless or “floating”. The arms are bent, brought to the body, the legs are extended. Extrapyramidal phenomena, chewing, sucking, and swallowing movements are possible. Urination and defecation are involuntary. Reactions to various kinds of stimuli are scattered. With positive dynamics, the patient reacts to touching it by chewing more frequently and intensifying, and in response to pain, he makes chaotic movements, and then directed to the place of pain. In other words, he is already demonstrating the simplest sensorimotor act. The reintegration phase of simple sensory and motor responses is characterized by longer periods of wakefulness, which can be supported by feeding and other procedures. There is a clear tendency towards the formation of a normal sleep-wake cycle.
The patient's reactions to close people are guessed - this is, for example, facial hyperemia, increased chewing, vocalization such as mooing, etc. Anxiety appears and then becomes constant before urination, as well as defecation. Movements to the place of pain are also constant. Reactions to the urge to urinate, to the voices and touches of loved ones become more and more vivid and stable; the patient seems to distinguish the latter from strangers. Some spontaneous movements return, sometimes stereotypical ones.
The stage of reintegration of the simplest psychomotor and psychosensory reactions manifests itself in longer daytime wakefulness, persistent revival before urination, defecation and calm after these functions. Facial expressions of suffering and disgust become clear, and the first signs of differentiation of smells, tastes, edible and inedible appear. When touching himself, the patient begins to make certain movements, for example, opening his mouth if his lips are touched with a spoon. He can be taught to bring his hand to his mouth. Spontaneous movements diversify, gradually acquiring the property of arbitrariness.
Reactions to loved ones become clearer. It is on them that he begins to fix his gaze, at first sometimes for a very short time, and gradually - more often and for a longer time. Then gaze tracking is restored. The sleep-wake cycle becomes close to normal.
A number of publications present the results of observation of patients who were in a vegetative state for a long time. It has been established that most often in the future they experience deep disability.
3. Akinetic mutism
This is a condition with akinesia and mutism, which in favorable cases ends with the restoration of motor activity, understanding of speech and one’s own speech activity (or identification of aphasia). First, speech understanding is restored. While awake, patients lie with their eyes open, turning their gaze and head towards the source of sound or light. Their facial reactions to words with different meanings gradually differentiate. The simplest and then more complex requests are fulfilled, and movements are accelerated. Lack of speech understanding indicates the fact of sensory aphasia. Next, one’s own speech is restored. This is happening against the backdrop of an increasing variety of active movements. The first word is rarely spontaneous and is pronounced very unclearly. Episodes of pronouncing phonemes and words gradually become more frequent, then verbalization becomes spontaneous. Phrasal speech appears, and eventually speech contact is restored. As active speech is restored, the forms of voluntary motor activity also expand. The absence of active speech indicates motor or dynamic aphasia.
In addition to akinetic mutism, patients may also experience hyperkinetic mutism. This often happens when the right hemisphere of the brain is predominantly affected. Motor excitation is iterative in nature: patients sometimes repeat the same movement until exhaustion, returning to it after a break and not paying attention to the speech addressed to them. Characterized by inversion of the sleep-wake cycle. Excitement intensifies in the evening and at night. Nevertheless, even in this state, speech is gradually restored. First comes the understanding of individual words, phrases, simple requests, and the fulfillment of the latter. As the understanding of the meaning of words is restored, motor excitement weakens, and the patients' behavior becomes more orderly. Then the patients themselves make attempts to articulate sounds and words. At first, they try to speak in response to speech addressed to them, then their speech gradually becomes more and more spontaneous. In the absence of aphasia, phrasal speech is also restored to varying degrees.
4. Confusion syndromes
This is a group of very heterogeneous disorders, the place of which in the mentioned scale of postcomatose disorders is not indicated. The group also includes clouding of consciousness syndromes, and even the phenomena of depersonalization-derealization. But since we are talking not about the laws of psychopathology, but about the empirical side of the matter, we will briefly describe these disorders, if possible in accordance with the Dobrokhotova-Zaitsev scale.
Amnestic confusion is a fixation amnesia with a predominant lesion of explicit memory and loss of cognitive structures that organize current impressions. The result is amnestic disorientation.
Amnestic-confabulatory syndrome includes, in addition to fixation and congrade, also retrograde amnesia and confabulation of the replacement type.
Korsakov's syndrome in terms of mental disorders does not differ significantly from the previous one. Sometimes Korsakoff's syndrome occurs in combination with left-sided hemiparesis, hemihypesthesia, hemianopia and left-sided gaze disturbances. Such patients also exhibit left-sided spatial agnosia associated with focal pathology of the right parieto-temporo-occipital region.
Patients do not notice, ignore the left half of space, including their own body, are not aware, for example, of left-sided paralysis, loss of sensitivity on the left. T.A. Dobrokhotova and other authors indicate that Korsakov's syndrome and left-sided spatial agnosia “can be considered intermediate between disturbed and clear consciousness” and that they “can complete the restoration of consciousness after a coma.”
Speech confusion is represented by partial or complete aphasia (sensory, motor or amnestic). The disorder can be combined with right-sided hemiparesis. Speech motor excitation is observed in severe TBI with intracranial hemorrhage. Periods of general and speech arousal may be followed by depression of consciousness (up to coma), which indicates an increase in the volume of hemorrhage.
Syndromes of stupefaction are relatively rare and mostly occur in mature patients. They are not observed in old people and children in the first years of life. Mention is made of oneiroid, depersonalization and derealization, “flashes of past experiences” (meaning life in the past, i.e. ecmnesia), twilight state and delirium. Psychotic disorders usually occur in the first two months after emerging from a coma.
Transient global amnesia is temporary (up to 24 hours) and total amnesia, in which absolutely everything can be forgotten, including one’s own name. Sometimes it happens immediately after a very short coma (seconds, minutes), it is noted with a concussion, mild to moderate bruises of the brain. It is important not to confuse this disorder with episodes of amentive confusion.
5. Affective disorder syndromes
The absence and extreme impoverishment of emotionality and expressiveness in post-comatose states is later replaced by euphoria, anger, aggressiveness, and then mania, depression, and bipolar mood disorders may occur. The most severe disturbances in the emotional sphere are observed with bruises and hematomas of the frontal regions of the cerebral hemispheres. Bipolar affect disorders in TBI are observed with damage to the right hemisphere.
Emotional paralysis (in aspontaneity syndrome) is observed in severe TBI with hemorrhage in the left frontal region of the brain. The phenomena of aspontaneity can last for months. As the patient’s activity increases, against a background of indifference, initially rare smiles, irritation, anger, and gradually and more often other emotional manifestations appear.
Euphoria with disinhibition is more often observed with contusions of the fronto-basal parts of the brain, and lasts most long after a prolonged coma. This condition is usually defined as pseudoparalytic syndrome.
Angry mania usually occurs in patients with bilateral damage (contusion) to the frontotemporal regions of the brain. Combined with euphoria. It is more pronounced in mature patients in the acute period of TBI, lasting up to several weeks.
Dysphoria occurs in the long-term period of TBI and occurs in short (up to several days) and repeatedly repeated episodes. Possible evening worsening of mood.
Hypomania in TBI is rare and occurs both in the acute period of concussion and in the long-term period with bruises and hematomas of the posterior parts of the right hemisphere. According to EEG data, it indicates activation of brainstem structures.
Melancholy depression is more characteristic of remote and intermediate periods of the course of a traumatic disease with damage to the temporal parts of the right hemisphere. It is usually combined, like other affective disorders, with a psychoorganic disorder.
Anxious depression is more often observed with bruises of the temporal part of the dominant hemisphere (i.e., left - lateralization is indicated from the position of a right-handed person).
Apathetic depression is observed with damage (bruise) mainly to the anterior parts of the hemispheres.
6. Borderline syndromes
Asthenic syndrome. The phenomena of asthenia are observed at different stages of the course of a traumatic disease. Often this is the only disorder in the residual period of TBI.
Obsessive-phobic syndrome. It occurs quite rarely in TBI.
Hysteria-like syndromes. Sometimes there are phenomena of pseudodementia, as well as rental behavior.
Phenomena of pseudology. According to some reports, they were often encountered after head injury (especially with brain contusions) during the Great Patriotic War.
Paranoid syndrome . Rarely encountered; its connection with TBI is quite complex.
Hypochondriacal syndrome. Shows somewhat exaggerated attention to the state of one's own health. Much more often, perhaps, patients underestimate the severity of their disorders.
7. Syndromes of decreased mental activity
Traumatic dementia. It is a consequence of severe TBI or a series of TBIs of lesser severity. According to A.S. Shmaryan (1948), one should not rush to make this diagnosis. There are known facts of significant improvement in cognitive functions in seemingly hopeless cases.
Memory disorders. This refers to different types of amnesia of the organic type.
Abulia. Rarely reaches the degree of complete spontaneity. Significant improvement is possible, however, even in severe cases.
8. Epileptic syndrome
A common consequence of TBI. Seizures are observed, for example, in 12% of children who have suffered a TBI. Seizures can be of different types, but in a patient with traumatic epilepsy they are usually of the same type. If these are grand mal seizures, then, as a rule, they are secondary generalized. With left-sided brain damage, twilight states of consciousness, absence seizures, psychomotor seizures, speech and ideation seizures, and seizures with psychotic phenomena may occur. More often (72%) seizures occur 6–12 months after TBI. It is believed that with traumatic epilepsy, personality changes are less pronounced than with genuine epilepsy. The exception is children and adolescents who were injured at an early age.
Some authors believe that TBI in early and old age has more severe consequences. Treatment for patients with TBI is individualized and determined by the current condition. Of primary importance is therapy aimed at eliminating liquorodynamic, metabolic, hemodynamic disorders, inflammatory processes, resorption of adhesions and scars. The prognosis is determined by the severity of the TBI and subsequent complications.
Back to contents