Dyscirculatory encephalopathy of the brain (DEP) is a progressive lesion of cerebral structures against the background of vascular diseases. It manifests itself as worsening intellectual, psycho-emotional and movement disorders. Widespread, observed to varying degrees in 5–6% of Russians.
An appointment with a neurologist is made by phone 8(969)060-93-93.
Reasons for development
The main etiofactor is insufficient blood supply caused by pathological changes in blood vessels. In 60% of cases, DEP is provoked by cerebral atherosclerosis. The second place in prevalence is occupied by increased blood pressure due to hypertension and secondary hypertension due to kidney damage, Itsenko-Cushing's disease, and pheochromocytoma.
Other causes include vertebral artery syndrome, cerebral vascular anomalies, cervical osteochondrosis, spinal injuries, arrhythmias, vasculitis, arterial hypotension and TBI. Diabetes mellitus, complicated by diabetic macroangiopathy, is often cited as the main or complicating factor.
Previously, encephalopathy of discirculatory (vascular) origin was traditionally considered as a disease of the elderly. Now the situation has changed. Heart diseases have become “younger”, which has led to an increase in the frequency of early manifestations of DEP. Experts point out that currently the pathology is often detected in people under 40 years of age.
When systemic metabolic disorders are added, they speak of discirculatory dismetabolic encephalopathy of complex (mixed) origin. This option is more typical for representatives of older age groups.
Who's at risk
It was previously thought that older people were more susceptible to DEP. Currently, the disease has become significantly “younger” and quite often it is diagnosed in patients who are under 50 years of age. In most cases, these are people of creative professions and mental work. The most severe consequences of discirculatory encephalopathy include senile dementia and ischemic stroke.
Factors that provoke the disease are: poor diet with a predominance of fatty and smoked foods, alcohol abuse, smoking, excess weight, hormonal disorders, high blood pressure, head injuries.
Development mechanism
Insufficient blood supply to the brain leads to deterioration of nutrition, hypoxia and death of nerve cells, which means the formation of numerous “silent infarctions” and areas of rarefaction of cerebral tissue. The most affected are the subcortical structures and white matter, located at the border between areas, the blood supply of which is carried out from different large arteries.
The predominant localization of the lesion explains the “disconnection phenomenon” - the loss of connections between cortical and subcortical structures. In the early stages of the disease, functional changes occur, which are reversible with timely initiation of adequate therapy. Subsequently, persistent disorders develop, often leading to disability. In half of the patients, encephalopathy of the dyscirculatory type is complicated by degenerative processes, which makes its course more severe.
Dyscirculatory encephalopathy (DE) is a syndrome that includes a complex of subjective and objective signs arising from chronic insufficiency of blood supply to the brain, which is characterized by gradually increasing changes in symptoms and structural changes in the brain.
Quite often, terms such as chronic cerebral ischemia, cerebral atherosclerosis, hypertensive encephalopathy, vascular dementia and others are used as synonyms for DE.
DE is not an independent disease, but most often a manifestation of diseases such as arterial hypertension (AH), atherosclerosis, or a combination thereof. Diabetes mellitus and heart failure can also make an unfavorable contribution to the development and course of DE.
With cerebral ischemia/hypoxia, the structural and functional interaction between neurons and the vessels supplying them is primarily disrupted, resulting in the development of dysfunction of the “neurovascular unit”, which unites astrocytes, neurons, glial cells, pericytes, endothelial cells and other cells of small vessels. Such changes are based on damage to the basement membrane, an increase in its permeability, damage to endothelial cells and destruction of interendothelial connections, and activation of extracellular metalloproteinases. Oxygen radicals produced by vascular cells and neurons play an important role in these processes. As a result of the interaction of superoxide anion with nitric oxide, the bioavailability of the latter decreases, the lumen of blood vessels narrows, their resistance increases, blood flow decreases, and ischemia increases. The resulting peroxynitrite has a cytotoxic effect on neurons, microenvironmental cells, and endothelial cells. This leads to disruption of autoregulation of cerebral circulation and regulation of the permeability of the blood-brain barrier. Extravasation of blood plasma components into the vascular wall, as well as adjacent areas of the brain, causes thickening and disintegration of the wall of small cerebral vessels (arteries and arterioles), perivascular edema and damage to the white matter of the brain. Microangiopathy leads to diffuse or multifocal brain damage. As a result of damage to the pathways in the white matter of the brain, there is a disconnection of cortical (especially frontal) and subcortical structures, which causes impairment of motor and mental functions.
Thus, it is the disruption of the intercellular interaction of neurovascular units that is attributed the main role in the development of pathological changes in DE. Diagnostic difficulties at the onset of the disease are caused by nonspecific complaints and insignificant objective signs.
Later, as the disease progresses, the signs become more distinct and instrumental examination reveals more severe signs of structural brain damage. It should be remembered that the appearance of even the first complaints and the identification of coordination disorders, uneven tendon reflexes, signs of oral automatism in the presence of hypertension and cerebral atherosclerosis can be an early manifestation of DE, which requires appropriate therapeutic measures.
There are three stages during DE:
- I – mild or moderate (compensation stage);
- II – pronounced (stage of subcompensation);
- III – pronounced (stage of decompensation).
At stage I of the disease, patients may complain of headache, dizziness, and tinnitus, which is often found in patients suffering from hypertension and without signs of encephalopathy. However, headache with DE does not have a clear relationship with changes in blood pressure (BP). Asthenic complaints are typical (decreased performance, increased fatigue, sleep disturbances). Mild cognitive-mnestic disorders appear: a decrease in working memory, the ability to remember and perform some everyday actions not related to professional activities. Irritability occurs and depression may develop. In this case, symptoms often intensify after strenuous or long work in the evening and disappear after rest. As already mentioned, a neurological examination may reveal mild disorders, in particular oculomotor reflexes, poor coordination, uneven tendon reflexes, and signs of oral automatism.
In stage II of the disease, the number and severity of complaints decrease and neurological symptoms become clearly expressed. This stage is characterized by disturbances in motor activity: movements become inexpressive, slow, their coordination is impaired, and small-scale tremor appears. Dominant neurological syndromes: pyramidal, discoordination, amyostatic. Cognitive impairment is increasing.
At stage III, objective neurological symptoms prevail over subjective manifestations. Cognitive impairments reach the level of real dementia and are accompanied by affective and behavioral disorders (gross decrease in criticism, apathetic-abulic syndrome, disinhibition, “explosive” character). Severe movement disorders, walking and postural balance disorders develop. Falls, fainting, and generalized seizures may occur. It should be noted that with hypertension and hypertensive encephalopathy, the risk of developing dementia increases by 45% compared to that in patients with hypertension without DE [1] and the risk of developing epilepsy increases by 2 times [2]. At this stage of DE, patients lose not only their ability to work, but also their ability to function independently. The same neurological syndromes are characteristic as in stage II, but their disabling effect increases significantly.
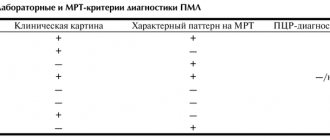
Thus, the diagnostic algorithm for DE can be presented as follows (Fig. 1) [3].
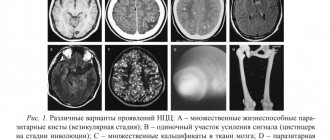
Modern research methods (computer or magnetic resonance imaging) make it possible to visualize changes in the brain at different stages of DE (Table 1).
When performing a computed tomography scan at stage I, there may be no obvious changes or minimal signs of brain atrophy and mild leukoaraiosis (decreased white matter density) may be detected; in stage II - small foci of reduced density, expansion of the ventricular system and hemispheric grooves due to the atrophic process, in stage III - multiple foci of various sizes in the hemispheres: post-ischemic cysts due to a lacunar stroke; severe atrophy of the cerebral cortex and hippocampus, severe leukoaraiosis.
Since the development of DE not only reduces the quality of life of people, but also leads to disabling disorders, proper treatment is of great not only medical, but also social importance.
Treatment for DE
The main goals of therapy can be formulated as follows:
- correction of risk factors for the development of DE and dementia;
- prevention of the development of transient ischemic attacks and strokes;
- reducing the rate of progression of DE, development and progression of dementia;
- elimination or reduction of the severity of neurological and mental manifestations of the disease.
The main thing is that in the early stages of the disease it is possible to solve the assigned problems; the transition to more severe stages reduces the effectiveness of the measures taken.
First of all, we are talking about adequate treatment of conditions that are the main causes of the development of DE: hypertension, dyslipidemia, diabetes mellitus. However, regarding treatment tactics, there is a lot of conflicting data and not only positive, but also possibly negative effects of the therapy, in particular on cognitive functions (CF) and the rate of onset of dementia, are constantly discussed. In this connection, it is necessary to dwell on this in a little more detail.
Therapy aimed at reducing the manifestations of atherosclerosis
Currently, indisputable evidence has been found that intensive statin therapy reduces the risk of developing macrovascular cardiovascular complications (myocardial infarction, stroke) both in primary [4] and secondary prevention [5]. Moreover, many of the positive effects are associated not only and not so much with the lipid-lowering effect, but with the pleiotropic effects of statins, in particular with a decrease in inflammation, oxidative stress, etc. [6]. A meta-analysis of observational studies found that people taking statins have a lower risk of developing dementia [7]. In short-term clinical studies, no effect of statins on changes in CF was found. In long-term studies (23,443 patients followed for an average of 3.0–24.9 years), the reduction in the incidence of dementia was 29% (odds ratio [OR] = 0.71, 95% confidence interval [CI] – 0. 61–0.82) [8]. This is confirmed by later analyzes [9].
At the same time, taking statins does not have a therapeutic effect on patients with Alzheimer's disease [10]. The authors of this Cochrane review indicate that there are no publications examining statin treatment for vascular dementia.
Therapy aimed at normalizing blood pressure
Hypertension itself significantly disrupts CP and leads to the development of DE [11]. Moreover, the increase in the risk of developing dementia is associated both with the level of blood pressure during the day and with the severity of nocturnal hypertension, the value of pulse pressure (both high and low), blood pressure variability, and the magnitude of its morning rise. Many studies have shown that antihypertensive therapy reduces the risk of strokes, but the assessment of its effect on DE is controversial. Thus, in the prospective study CSHA (Canadian Study of Health and Aging) [12], the relationship between the use of antihypertensive drugs of various groups and CF in people over 65 years of age was assessed over a 5-year period. It was shown that the use of calcium channel blockers more often than taking drugs of other groups led to a decrease in EF (75 versus 59%). The OR for a significant decrease in CF, measured as a 10 or more point decrease in the Modified Mini-Mental State score, was 2.28 (95% CI 1.12–4.66) for people using calcium channel blockers relative to β-blockers . However, taking into account other variables, it was shown that only the use of non-dihydropyridine calcium channel blockers increased the incidence of cognitive deficits in older people - OR = 3.72 (95% CI - 1.22-11.36). At the same time, a meta-analysis of 14 observational studies (32,658 people taking antihypertensive drugs and 36,905 not receiving antihypertensive therapy) showed that taking antihypertensive drugs significantly reduces the risk of developing any type of dementia (relative risk [RR] = 0.87 , 95% CI – 0.77–0.96) and vascular dementia (RR=0.67, 95% CI – 0.52–0.87), but does not reduce the risk of dementia due to Alzheimer’s disease or its severity [13]. On the other hand, a systematic review conducted by the Cochrane Alliance [14], which pooled data on 12,091 patients with hypertension in three large studies, did not find a significant effect of antihypertensive treatment on the risk of developing dementia. The reduction in the risk of developing dementia was 11% (RR=0.89; 95%CI – 0.69–1.16) and was not statistically significant, despite a significant decrease in blood pressure in elderly people who had not previously suffered from a decrease in CP.
It is believed that one of the reasons for the inconsistency of data obtained in randomized clinical trials may be the use of different groups of antihypertensive drugs. Thus, thiazide-like diuretics, despite reducing blood pressure and the risk of stroke, did not lead to a protective effect against dementia [15, 16].
Most studies have provided evidence that calcium channel blockers may reduce the incidence of dementia in patients with hypertension. Thus, in the Vascular Dementia Project of the Syst-Eur trial in a group of elderly people with isolated systolic hypertension who received active therapy with nitrendipine, the incidence of dementia was lower than in those receiving placebo [17]. According to a Cochrane review [18], nimodipine leads to to a highly significant (p<0.00001) reduction in changes compared to placebo on the SCAG (Sandoz Clinical Assessment Geriatric) scale in the general clinical condition and CF. This is confirmed by a study [19], where it was shown that calcium channel blockers slow down the decline in CF by approximately 0.4 points per year (MMSE scale - Mini-mental State Examination, p = 0.001). Other antihypertensive drugs did not have a similar effect. Active treatment with angiotensin-converting enzyme inhibitors and diuretics (more than 3 years) reduced the incidence of CF disorders and reduced the progression of dementia in women over 70 years of age [20].
Some evidence suggests that sartans (candesartan, valsartan, telmisartan), more than other drugs (lisinopril and hydrochlorothiazide), may improve CF, particularly in older patients with hypertension [21–23].
As can be seen from the data presented, the main results of antihypertensive therapy assess the effect on CP, but not on neurological symptoms.
It should be taken into account that changes in CP and depression that occur during DE may reduce patients’ adherence to antihypertensive and other therapy.
Vasoactive and metabolic therapy
To reduce the rate of progression of DE, the use of drugs that improve cerebral blood flow and metabolism in brain tissue is pathogenetically justified. These drugs can influence the severity of neurological and mental disorders in DE. It should be emphasized that drugs that improve cerebral blood flow and neuronal metabolism are potentially more effective in the early stages of DE.
To improve cerebral blood flow, drugs of various groups are used that have a vasodilating effect:
1. Phosphodiesterase inhibitors:
Euphylline and pentoxifylline - by increasing the content of cAMP in the smooth muscle cells of the vascular wall, they block adenosine (purine) receptors; reduce the flow of calcium ions through the channels of cell membranes, reduce the contractile activity of smooth muscles, which leads to relaxation of blood vessels and an increase in their lumen. These drugs inhibit platelet aggregation by suppressing platelet activating factor and prostaglandin E2-alpha, increase the resistance of red blood cells to deformation and thereby lead to an improvement in the rheological properties of blood, reduce thrombus formation and normalize microcirculation. With DE, these drugs reduce dizziness, headache, memory and sleep disturbances.
They should be used with caution in patients with heart damage, especially in acute coronary syndrome and heart failure. May increase the effects of antihypertensive drugs, the anticoagulant effect of heparin and fibrinolytic drugs.
Vinpocetine inhibits Ca2+-calmodulin-dependent cGMP phosphodiesterase, increases the content of catecholamines (dopamine and norepinephrine), increases the activity of adenylate cyclase, levels of adenosine monophosphate (AMP) and cyclic guanosine monophosphate (cGMP) in the brain. Increases the concentration of ATP in brain tissue. Reduces the functional activity of cellular transmembrane sodium and calcium channels, glutamate receptors N-methyl-D-aspartate and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (NMDA and AMPA). relaxes the smooth muscles of cerebral vessels, increases cerebral blood flow without significantly changing systemic circulation parameters. Moreover, there is an improvement in blood supply, mainly to ischemic areas of the brain, and there is no “stealing” effect. The drug improves the transport of energy substrates to tissues, increases glucose uptake, enhances aerobic glycolysis and improves the tolerance of hypoxia by brain cells. It has an antioxidant effect, reduces blood viscosity by reducing platelet aggregation and red blood cell deformability. It has neuroprotective activity and enhances the neuroprotective effect of adenosine.
2. Calcium channel blockers have a vasodilating effect due to a decrease in the intracellular content of calcium ions (Ca2+) in the smooth muscle cells of the vascular wall:
Cinnarizine is a selective blocker of slow calcium channels that directly reduces the tone of the smooth muscles of arterioles and reduces their response to nutrients (adrenaline, norepinephrine, dopamine, angiotensin, vasopressin). It has a vasodilating effect (especially in relation to cerebral vessels), without having a significant effect on blood pressure. It exhibits moderate antihistamine activity, reduces the excitability of the vestibular apparatus, and lowers the tone of the sympathetic nervous system. Increases the elasticity of red blood cell membranes, their ability to deform, and reduces blood viscosity.
Flunarizine acts similarly to cinnarizine. Improves cerebral circulation and oxygen supply to the brain; reduces vestibular disorders (impaired coordination of movements). It has an anticonvulsant effect and reduces the frequency of seizures in epilepsy.
Nimodipine primarily affects the blood vessels of the brain, normalizes cerebral blood supply, increases the tolerance of neurons to ischemia, and stabilizes the functions of nerve cells.
3. The alpha1-adrenergic blocker nicergoline has a vasodilator effect, eliminating the vasoconstrictor effect of the mediators of the sympathetic nervous system - adrenaline and norepinephrine. In addition, nicergoline improves metabolic and hemodynamic processes in the brain, reduces platelet aggregation and improves the rheological properties of blood, has a direct effect on the cerebral neurotransmitter systems - adrenergic, dopaminergic and cholinergic, increasing their activity, which helps optimize cognitive processes, reduces the severity of behavioral disorders, associated with dementia.
Of particular interest is the use of the combined drug Vasobral, containing α-dihydroergocriptine, a dihydrogenated ergot derivative that blocks α1- and α2-adrenergic receptors, as well as caffeine. Thus, the drug has dopaminergic, serotonergic effects, reduces the aggregation of platelets and erythrocytes, reduces the permeability of the vascular wall, increases the number of functioning capillaries, improves blood circulation and metabolic processes in the brain, increases the resistance of brain tissue to hypoxia and has psychostimulating and analeptic effects, enhances the processes stimulation in the cerebral cortex (increases mental and physical performance, reduces fatigue and drowsiness, improves memory for recent events, attention, reduces orientation disorders).
To reduce the severity of neurological symptoms and DE syndromes, as well as cognitive impairment, drugs are used that improve metabolism in the brain and have a neuroprotective effect:
1. GABAergic drugs:
Gamma-aminobutyric acid (GABA) is a biogenic amine found in the central nervous system and takes part in neurotransmitter and metabolic processes in the brain. GABA serves as the main mediator involved in the processes of central inhibition as a result of interaction with specific GABAergic receptors. Under the influence of the drug, the metabolic processes of the brain are restored: energy processes are activated, glucose utilization improves, the respiratory activity of tissues increases, and blood supply improves. GABA helps remove toxic metabolic products and normalizes the dynamics of nervous processes. Increases thinking productivity, improves memory, and has a mild psychostimulating effect. The nootropic drug piracetam has a similar effect, which enhances the synthesis of dopamine in the brain, increases the content of norepinephrine, partially affects GABAergic receptors, increases the amount of acetylcholine at the synaptic level and the density of cholinergic receptors. Stimulates redox processes, increases glucose utilization, improves regional blood flow in ischemic areas of the brain, increases the body's energy potential with the participation of ATP and adenylate cyclase. Piracetam, like other nootropics, increases the resistance of the central nervous system to hypoxia, improves integrative brain activity, promotes memory consolidation, and improves learning processes. Pyriditol may have a similar effect.
2. Peptidergic drugs and amino acids:
Cerebrolysin contains low molecular weight, biologically active neuropeptides, which are fragments of a number of brain neurotrophic factors (ciliary neurotrophic factor - CNTF, glial neurotrophic factor - GDNF, insulin growth factor-1 IGF-1 and insulin growth factor-2 IGF-2), penetrating through the blood-brain barrier and directly reaching the nerve cells. The drug has an organ-specific polymodal effect on the brain, i.e. provides metabolic regulation, neuroprotection, functional neuromodulation and neurotrophic activity. Increases the efficiency of aerobic energy metabolism of the brain, improves intracellular protein synthesis in the developing and aging brain. The drug protects neurons from the damaging effects of lactic acidosis, prevents the formation of free radicals, increases survival and prevents the death of neurons under conditions of hypoxia and ischemia, and reduces the damaging neurotoxic effect of excitatory amino acids (glutamate). It has a positive effect on the clinical and mental status of patients with DE, which is confirmed by the positive dynamics of electroencephalography indicators, and has a positive effect on CF disorders and on memory processes.
The endogenous regulator of the function of the central nervous system, Semax, is a synthetic heptapeptide, an analogue of the ACTH fragment 4–10 (methionyl-glutamyl-histidyl-phenylalanyl-prolyl-glycyl-proline), devoid of hormonal activity, which has a pronounced nootropic effect. By stimulating the function of the forebrain, it enhances selective attention at the time of information perception, improves memory consolidation, and increases learning ability. The drug also has antioxidant and antihypoxic effects.
A peptide bioregulator of brain functions is used quite widely in clinical practice: Cortexin in the complex therapy of patients with DE stages I–II helps improve the functions of attention, perception, memory and thinking, as well as normalize cortical neurodynamic processes.
Drugs that affect metabolic processes in brain cells:
Improvement of metabolic processes (supply of oxygen and glucose to the brain), antihypoxic effect on tissues, reduction of oxidative stress by reducing the formation of free radicals and lipid peroxidation of cell membranes is shown in the drug Tanakan, a standardized drug of plant origin (Ginkgo Bilobae foliorum extract). Tanakan also affects the release, reuptake and catabolism of neurotransmitters (norepinephrine, acetylcholine, dopamine and serotonin) and their ability to bind to membrane receptors. In combination with improving vasomotor reactions, it normalizes the tone of arteries and veins, improves microcirculation, rheological properties of blood, helps improve blood flow, and prevents red blood cell aggregation, which inhibits the effect on platelet activation factor. The drug improves cognitive deficits.
To correct cognitive impairment, the glutamate N-methyl-D-aspartate receptor antagonist Akatinol Memantine is also used, which reduces oxidative stress and excitotoxicity processes (damage and death of nerve cells under the influence of neurotransmitters, L-glutamate and other substances).
Citicoline is a natural endogenous nucleoside consisting of cytidine and choline linked by a diphosphate bridge, which is involved in the synthesis of membrane phospholipids as an intermediate. Restoration of cell membranes or reduction of their damage also occurs due to a decrease in the synthesis of phospholipase A2 and a decrease in the accumulation of free fatty acids, normalization of Na+/K+-ATPase function, increased activity of antioxidant systems, and reduction of oxidative stress. There is an improvement in cholinergic, dopamine and glutamatergic neurotransmission. The drug has a pronounced neuroreparative effect, reducing cell apoptosis and stimulating the processes of neuro- and angiogenesis. In chronic cerebral hypoxia, citicoline is effective in the treatment of cognitive disorders such as memory impairment, lack of initiative, and difficulties in performing daily activities and self-care. Increases the level of attention and consciousness, and also reduces the manifestation of amnesia.
Actovegin is a deproteinized hemoderivative of calf blood, containing more than 200 components. It affects a host of biochemical pathways and has many pleiotropic neuroprotective and metabolic effects. Actovegin increases the utilization of pyruvate (glucose metabolite) in mitochondria, reduces the formation of lactate, stimulates oxygen consumption, restores ionic homeostasis, optimizes energy metabolism (ATP synthesis and phosphocreatine formation), and leads to the stabilization of plasma membranes of cells during ischemia. Actovegin has an insulin-like effect - it activates aerobic glycolysis, i.e. transfers the cell to a more advantageous path of glucose utilization: glucose consumption by the cell increases by 5 times, and oxygen consumption by the cell increases by 6–7 times. Thus, Actovegin has an antihypoxic effect, which begins to manifest itself no later than 30 minutes after parenteral administration and reaches a maximum after an average of 3 hours (2–6 hours). Actovegin has a beneficial effect on the biological effects of amino acids - glutamate, aspartate and GABA. Actovegin not only affects cellular metabolism, but also improves microcirculation.
With DE, it has numerous properties: it reduces vestibulocerebellar disorders (dizziness, noise in the head and ears, lack of coordination, improves CF), helps improve the quality of life, and increases social activity. This is evidenced by a number of clinical studies conducted in accordance with modern requirements. Thus, in a double-blind, placebo-controlled study, it was shown that oral administration to elderly patients for 12 weeks significantly improved mnestic-intellectual functions (memory, synthetic and analytical abilities, concentration, memorization) [24]. A multicenter study of 1549 elderly patients showed that Actovegin therapy (2 weeks of intravenous injections of 10 ml of Actovegin solution, and then 4 weeks of oral administration of Actovegin film-coated tablets, 2 tablets 3 times a day) improved the general condition: decreased (or stopped ) headache, dizziness, anxiety and fear, memory and concentration improved (according to psychological testing) [25]. Similar data were obtained in other studies [26].
The design of the ARTEMID study was published, the purpose of which was to establish the effect of Actovegin on cognitive impairment in patients who had suffered a stroke [27].
In recent years, much attention has been paid to elucidating the mechanisms of the protective action of this drug. It is known that many neurodegenerative diseases are accompanied by the death of neurons through the mechanisms of necrosis and apoptosis. In the case of necrosis, an inflammatory response is observed, associated with the participation of proinflammatory cells and cytokines. These include microglial cells and blood phagocytes in the central nervous system.
Using primary cultures of rat neurons, it was established [28] that Actovegin inhibits the death of neurons in vitro and preserves synaptic connections between neurons. In addition, Actovegin dose-dependently reduces the apoptosis of such neurons. These protective properties of Actovegin are closely associated with a decrease in the generation of oxygen radicals, the formation of which was induced in neurons by the amyloid ten-amino acid peptide Aβ-(25-35), as well as a decrease in the level of reactive oxygen species in the cytoplasm of these cells [28].
In our laboratory, using transplanted human neurons of the SK-N-SH line, it was shown that Actovegin reduced cell death induced by hydrogen peroxide.
This protective effect of Actovegin was accompanied by a decrease in the level of intracellular oxygen radicals and a pronounced decrease in neuronal apoptosis [29]. The development of neuronal apoptosis is controlled by various intracellular signaling pathways. Using inhibitors of mitogen-activated protein kinases (p38MAPK), extracellular regulatory kinases (ERK), phosphatidylinositol-3 kinase (PI-3K) and c-Jun-N-terminal kinase (JNK), we showed for the first time (Fig. 2) that in In the mechanism of the protective effect of Actovegin against peroxide-induced apoptosis of SK-N-SH cells, the dominant role belongs to two protein kinases: p38 MAPK and PI-3K [30]. Also, using whole blood samples from patients with heart failure of functional classes II–III according to NYHA, it was shown that Actovegin, in a dose-dependent manner, effectively suppresses one of the most important manifestations of systemic inflammation - the generation of oxygen radicals by blood phagocytes induced by formyl peptide or phorbol ester, and thanks to its antioxidant properties, it removes formed oxygen radicals [31, 32].
Thus, Actovegin corrects energy metabolism, has an antioxidant effect, suppresses inflammatory reactions, affects neurons, vascular cells and blood cells, preserves synaptic connections between neurons, preserves the integrity and improves the functioning of “neurovascular units”.
It should be noted that the use of neuroprotective drugs with different mechanisms of action can increase the effectiveness of treatment. In particular, the combined use of citicoline and Actovegin (Table 2) in conditions of cerebral ischemia is considered optimal from the point of view of effectiveness.
In conclusion, it must be emphasized once again that therapy is most effective in stages I and II of the disease.
Classification
Taking into account the cause of development, the disease can be atherosclerotic, venous, hypertensive and mixed. Depending on the characteristics of the course, classic, galloping (rapidly progressing) and remitting varieties of the disease are distinguished. To clarify the severity of the process, a general three-stage classification is used, where:
- Stage 1 (initial). There are minor disorders of the emotional sphere and cognitive activity, there is no neurological deficit.
- Stage 2 (moderate). Cognitive-emotional dysfunction worsens and is accompanied by motor symptoms.
- Stage 3 (decompensation). The ability to work and the ability to self-care are lost, and dementia develops.
Discirculatory encephalopathy 2nd degree - clinical manifestations
Without proper treatment, DEP of the 1st degree progresses to the second with all the ensuing consequences. Symptoms of grade 1 dyscirculatory encephalopathy of the brain include attention and memory disorders, and spatial orientation is disturbed. Complete apathy towards the outside world appears. In some cases, loss of ability to work may occur.
Stage 3 DEP is a severe degree of the disease, in which the patient loses the ability to perform purposeful actions and needs constant care. Characteristic manifestations are disturbances in speech and pelvic organ function, seizures, and movement disorders. The patient receives disability due to the diagnosis of dyscirculatory encephalopathy of the 3rd degree.
Symptoms
Stage 1
Characterized by a gradual onset and chronic course. Emotional disturbances are often the most noticeable in the beginning. In 65% of cases, depressive symptoms reminiscent of hypochondriacal neurosis are detected. Complaints of depression and decreased mood are usually absent; unpleasant somatic sensations come to the fore: headache, noise and ringing in the head, pain in the back and joints.
Differences from neurotic depression are the absence of a provoking traumatic situation, the low effectiveness of psychotherapy and antidepressants. In adults, the symptom that determines the picture of the disease is sometimes emotional lability: attacks of aggression or causeless crying, sudden changes in mood, increased irritability. The clinic is complemented by absent-mindedness, deterioration of sleep and fatigue.
In 90% of patients, cognitive impairment occurs at the initial stage. The ability to concentrate and plan actions decreases. Memory deteriorates, thinking slows down. In the motor sphere, dizziness and slight instability when walking are sometimes detected, which are the first signs of vestibulopathy.
Stages 2 and 3
When moving from grade 1 to grade 2, motor and cognitive dysfunction worsens. Due to amnesia, decreased attention and intelligence, usual mental work becomes unbearable. A decrease in criticism and the ability to navigate in place and time arise and gradually worsen. At stage 3, behavior and personality suffer. Due to dementia, patients lose their ability to work, and in severe cases, their ability to self-care.
Apathy prevails. People are not interested in anything, do nothing or do something unproductive, and show indifference to the world around them. Movement disorders become more pronounced and noticeable from the outside. A shuffling gait is formed in small steps without lifting the foot off the floor. Patients with vestibulo-atactic syndrome have progressive balance disorders.
Signs of transition to stage 3 are severe speech problems, paresis, trembling of the limbs, urinary incontinence and pseudobulbar syndrome. Some patients develop symptomatic epilepsy. Due to unsteady gait, people fall, resulting in fractures. Women especially often suffer from injuries, which is due to the prevalence of osteoporosis during menopause.
Initial stage of the disease
Symptoms of discirculatory encephalopathy at the initial stage are hardly noticeable, since the function of dead cells is taken over by nearby neurons. In this case, minor signs appear that are not clearly expressed:
Advertising:
- headaches with a feeling of fullness;
- dizziness;
- memory loss;
- noises in the head;
- irritability;
- emotional instability.
At this stage of the disease, with timely treatment, remission for decades is possible, and in some cases, complete recovery.
Multiple sclerosis is often mistakenly called memory loss in old age. In fact, this is a disease of young people, difficult to treat, and its consequences are very serious. Read more in the article: “multiple sclerosis symptoms and causes.”
Diagnostics
Early diagnosis is of great importance for long-term ability to work and a high quality of life, so older people should undergo periodic examinations by a specialist in the field of neurology. Tests are used to detect minor cognitive dysfunction. The examination program includes the following procedures:
- examination by an ophthalmologist, determination of visual fields, ophthalmoscopy;
- echoencephalography, electroencephalography, rheoencephalography;
- Dopplerography and duplex of head and neck vessels, magnetic resonance angiography.
Differential diagnosis with other pathologies involves MRI. To clarify the reasons, an examination by a cardiologist is prescribed; according to indications, consultations with a nephrologist and endocrinologist are carried out. The list of laboratory tests includes a coagulogram, determination of glucose, lipoproteins and cholesterol. If arrhythmia is suspected, electrocardiography and daily ECG monitoring are indicated.
Cost of services
| CONSULTATIONS OF SPECIALISTS | |
| Initial consultation with a psychiatrist (60 min.) | 6,000 rub. |
| Repeated consultation | 5,000 rub. |
| Consultation with a psychiatrist-narcologist (60 min.) | 5,000 rub. |
| Consultation with a psychologist | 3,500 rub. |
| Consultation with Gromova E.V. (50 minutes) | 12,000 rub. |
| PSYCHOTHERAPY | |
| Psychotherapy (session) | 7,000 rub. |
| Psychotherapy (5 sessions) | 30,000 rub. |
| Psychotherapy (10 sessions) | 60,000 rub. |
| Group psychotherapy (3-7 people) | 3,500 rub. |
| Psychotherapy session with E.V. Gromova (50 minutes) | 12,000 rub. |
This list does not contain all prices for services provided by our clinic. The full price list can be found on the “Prices” , or by calling: 8(969)060-93-93. Initial consultation is FREE!
Treatment
According to clinical recommendations, therapy should be comprehensive, aimed at reducing the manifestations of vascular disease, improving cerebral circulation and microcirculatory processes, protecting cerebral structures from ischemia and hypoxia. The doctor explains what kind of disease this is and why it is important to undergo regular therapy.
How to treat is determined individually. Depending on the nature of the underlying pathology, anti-sclerotic, hypoglycemic and antihypertensive drugs are prescribed, and cholesterol levels are corrected using diet or special medications.
To improve hemodynamics, drugs from the groups of phosphodiesterase inhibitors, calcium channel blockers, and alpha-2 adenoceptor antagonists are used. Antiplatelet agents are used to normalize blood clotting. The brain's resistance to a lack of blood supply is increased with the help of neuroprotectors: GABA and pyrrilidone derivatives, membrane-stabilizing drugs, vitamins and cofactors. In some cases, surgical treatment is recommended: reconstruction of the arterial trunks, carotid endarterectomy, creation of an extra-intracranial anastomosis.
Recommendations for the prevention of DEP include timely treatment of vascular pathologies, blood pressure control, and giving up bad habits. How long you can live and what your quality of life will be depends on the time you start treatment and compliance with medical recommendations.
Call our operator at tel. 8(969)060-93-93 and make an appointment at a convenient time.
Predictions and prevention
It was mentioned above that in case of encephalopathy, patients are issued with disability. But this should not be considered a final verdict, since one can and should try to stop the manifestations of the disease. Even at stage 2 of the disease, its development can be stopped for 5 or more years. But if you neglect visits to the doctor and do not pay attention to the symptoms, the disease will go into the final, stage 3. Then strokes, blockage of blood vessels, swelling, etc. are more likely to occur.
There are no special preventive measures that can prevent DEP. By and large, it all comes down to general recommendations and regular preventive examinations. It is advisable to monitor blood pressure levels and normalize their indicators. It is important to check your blood cholesterol levels and avoid psycho-emotional shocks. If the disease has already been identified, you need to be examined twice a year and undergo a course of maintenance therapy prescribed by your doctor.
Stage 2 dyscirculatory encephalopathy is not a reason to give up and wait for death. On the contrary, regardless of the cause of such a condition, it is possible and necessary to be treated in order to improve health and prolong life. Attention to health, giving up addictions, timely diagnosis and treatment of various diseases are measures that every person can do. They can prevent the disease or alleviate its course.