Human infection, namely damage to the central nervous system by pork tapeworm, is one of the main causes of epilepsy today. Most often, this disease occurs where people farm and are in constant contact with pigs, and where sanitation and hygiene conditions leave much to be desired. According to recent data, neurocysticercosis affects approximately 50 million people per year. This disease is widespread in developing countries.
What it is?
Neurocysticercosis or cysticercosis of the brain is a disease that is caused by the pork tapeworm (Taenia solium) and affects the central nervous system. Every year, 50,000 people die due to this disease, and the rest remain disabled for life. The most endemic areas for this disease are: Mexico, South America, India, China, African countries, New Guinea.
A person becomes an intermediate host when they ingest pork tapeworm eggs. It enters the body through contaminated water, food and poor hygiene (hand washing). When ingested, cysticerci show a special affinity for the brain, eyes and striated muscles. It is these structures that contain large amounts of glycogen and glucose.
Fact 10: Elimination of neurocysticercosis requires interruption of the T. solium life cycle
Careful case detection, improved diagnosis and treatment, and public health awareness campaigns are key to controlling the parasite and interrupting its life cycle. There is a need to ensure the participation of many sectors in implementing activities that can reduce the risk of infection. WHO is working with countries to develop strategies tailored to their individual needs to enhance control of T. solium and improve the management of patients with neurocysticercosis. Partners in this effort include FAO, the World Organization for Animal Health, the private sector, NGOs and the scientific community.
Causes of the disease
The main cause of the disease is the entry of the parasite into the human body. Initially, Taenia solium enters the body through the gastrointestinal tract and then spreads throughout the body through the bloodstream and is introduced into various tissues and organs.
The adult form of the tapeworm lives in the intestines, and often there may be no symptoms. An infected person releases a huge amount of the pathogen, thereby contaminating household items, especially if he does not adhere to hygiene rules.
After entering the brain, these embryos turn into cysticercus - the larval form of the pathogen. This is a finna up to 13-15 mm in size with liquid inside. The cysticercus shell is thin and not strong, and inside there are suckers and hooks. Cases have been described in medicine when the number of these larvae reached thousands. Then, local inflammation forms in the brain and a fibrous capsule forms around the larvae, which separates the cysticercus from the brain substance.
Most often, the larvae die after a year and a half, but leave behind bubble-like formations, which become calcified over time (cavities with calcium inclusions) and thus the inflammatory process becomes chronic.
Reference! According to data, on average cysticerci live 5-7 years.
In the brain, the larvae settle on the cerebral cortex, in the pia mater, in the basal ganglia, inside the ventricles (free floating or attached to the choroid plexus). In addition to causing local inflammation, they also interfere with the normal circulation of cerebrospinal fluid and compress the brain tissue.
When it enters the meninges, a strong inflammatory reaction is caused in the subarachnoid space and exudates of a dense consistency are formed, which subsequently affect the cranial nerves and the openings of Magendie and Luschka are blocked, which does not allow the cerebrospinal fluid to flow freely and hydrocephalus is formed. All these changes lead to the appearance of epilepsy and various neurological symptoms.
Forecast
Neurocysticercosis is a disease whose prognosis cannot always be predicted, since it is not known how many larvae are in the brain (after all, not all of them can be detected during examination). Late diagnosis, multiple lesions, lack of surgical treatment are unfavorable factors of the course. Sometimes death is possible during an epileptic attack or when the fourth ventricle is blocked with the development of acute occlusive hydrocephalus.
Thus, we can summarize the above: neurocysticercosis is a treacherous disease. Infection occurs unnoticed by humans. The disease may not make itself felt for a long time, sometimes it is completely asymptomatic. The detailed clinical picture does not have specific symptoms, and diagnosis requires a whole range of studies. Treatment is not always effective. In order not to become infected with neurocysticercosis, it is necessary to strictly observe the rules of personal hygiene and thoroughly process foods before eating them.
Symptoms
The clinical picture of neurocysticercosis is very diverse. But the specific symptoms of each patient depend on the following factors:
- number of cysticerci;
- location and attachment;
- what state the larva is in - alive, dead, dying;
- the body's ability to mount an immune response.
The main symptom of neucysticercosis is epilepsy - tonic-clonic or partial seizures. Neurological symptoms are different, but resemble those of a brain tumor. Intracranial hypertension, dementia, focal symptoms, dementia are also detected. The development of encephalitis is facilitated by massive infestation by larvae.
Very often the disease affects the sella turcica and the pituitary gland, which is located on it. And as a result, problems of an ophthalmological and endocrine nature begin.
When the spinal cord is damaged, motor-sensory disorders and pain along the spinal column, reminiscent of radiculitis, are detected.
When the eyes are affected, there is deterioration in vision, loss of visual fields and atrophy of the optic nerves.
Parenchymal neurocysticercosis
This form of the disease begins when cysticerci attach to the border of the white and gray matter of the brain. The parenchymal form is characterized by:
- decreased muscle strength in the limbs;
- convulsions - epileptic seizures. And these attacks get worse and become more frequent during the death of the parasite, because they release toxins and the damage increases;
- decreased sensitivity in the limbs;
- loss of visual fields due to damage to the optic chiasm;
- speech disorder;
- with damage to the cerebellum, unsteadiness of gait and dizziness are observed;
- trembling, tremor and involuntary flexion of the arms;
- dementia and loss of mental capacity;
- with massive damage, delusions and hallucinations appear.
Important! It should be remembered that the main symptom is convulsions and epileptic seizures, and that the frequency and duration increases with the start of therapy.
Cysticercosis of subcutaneous tissue and muscles
The introduction of pork tapeworm larvae into muscle tissue is accompanied by myositis, fever and eosinophilia. Tumor-like formations appear in muscle tissue. Nodes in the subcutaneous adipose tissue are round, soft, painless, often single, less often multiple (tens and even hundreds). After the death of the cysticerci, the nodes become denser and sometimes resolve. In some of them lime salts are deposited (petrification).
The palms, shoulders, chest and back are the most common locations for nodes.
In 40% of cases, cysticercosis of the subcutaneous tissue and muscles occurs with severe eosinophilia. An allergic reaction manifests itself in the form of hives.
The disease is often asymptomatic. The prognosis is favorable.
To identify cysticerci, X-ray examination and biopsy are used. On a radiograph, cysticerci enclosed in a capsule appear as oval or spindle-shaped formations with clear contours, often calcified.
Treatment is surgical. In some cases, treatment is not indicated; the patient is monitored. Mass death of parasites under the influence of anthelmintic drugs can lead to the development of a severe allergic reaction.
Rice. 11. Cysticercosis of the submucosal layer.
Rice. 12. Cysticercus in muscle tissue, separated from the bed.
Subarachnoid neurocysticercosis
This form of the disease is characterized by symptoms with meningeal signs, which are not as pronounced as with meningitis. Symptoms include: increased sensitivity to light and sound, nausea and vomiting that does not bring relief, headache and increased intracranial pressure, coma, dementia.
All symptoms depend on the number of larvae and what area of the brain they have affected. The greater their number and the size of the lesion, the more the symptoms worsen, the optic nerves are compressed and visual acuity rapidly deteriorates. Turning your eyes to the side becomes very painful.
The most serious complication is damage to the fourth ventricle of the brain, which often leads to death.
Intraventricular neurocysticercosis
Like the previous variant of the disease, the intraventricular form is characterized by intracranial hypertension. But this is also accompanied by a sharp attack-like deterioration of the condition. This is directly related to the movement of cysticerci in the ventricles. At one point, they can block the outflow of cerebrospinal fluid, which leads to increased pressure inside the skull.
This variant of neurocysticercosis is characterized by Bruns syndrome. It includes:
- attacks of dizziness;
- fainting;
- vomiting that does not bring relief;
- headache;
- bradycardia;
- disruptions in breathing rhythm;
- increased sweating.
Often it is the fourth ventricle that is affected, which leads to severe hydrocephalus.
Neurocysticercosis of the eye
In addition to severe brain damage, the disease also affects the condition of the eyes and visual functions. Symptoms include:
- drooping eyelid;
- rotation of the eyeball;
- conjunctivitis in the chronic stage;
- movements of the eyeballs become minimal and limited and are accompanied by painful sensations.
Also characteristic is swelling of the orbits and paraorbital areas, loss of visual fields and a feeling of a foreign body in the eye. During therapy, the larva dies and releases a toxin. As a result, optic nerve atrophy or abscess develops.
Diagnosis of the disease
With the development of medicine and the emergence of new diagnostic capabilities, it has become possible to identify the disease in the early stages and with the first appearance of symptoms. The main diagnostic methods include:
- Laboratory blood test. But this method helps to verify the disease only in 50% of clinical cases. From the analysis, eosinophil indicators are important for diagnosis. They indicate helminthic infestation.
- One of the main methods is to determine helminth eggs or their segments in feces. After the parasite is isolated, attention is paid to the scolex, the number of suckers and hooks.
- CSF analysis. In most cases, pleocytosis, increased glucose levels and increased blood pressure are detected.
- Immunological diagnostics. Using the express ELISA method, it is possible to detect antibodies to cysticerci in the blood.
- Serological methods are not very informative and very often give false positive results.
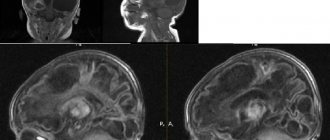
- MRI. Using this imaging method, doctors see foci of inflammation in the spinal cord and brain, in the brain stem and posterior cranial fossa. The use of gadolinium improved the visibility of the cyst walls.
- CT. Using this method, it is possible to identify cystic cavities and the calcifications that form on them. You can also see the focus of inflammation.
- Examination of the fundus. In the anterior chamber or in the vitreous body it is possible to see the cysticerci that float there.
Important ! One of the complications may be chorioretinitis or retinal detachment.
The structure of the pork tapeworm
The pork tapeworm (pork tapeworm) has a white ribbon-shaped body about 3 meters long (in rare cases it can reach 6 meters).
Figure 1 - Schematic structure of pork tapeworm
On the head (scolex) with a diameter of up to 3 mm there are four suckers, as well as a corolla of special hooks, the number of which is 22-32, for which it was nicknamed armed. All these devices help the helminth adhere to the wall of the small intestine of the final host.
Figure 2 - Scolex of pork tapeworm
The scolex is followed by a short, unsegmented neck up to 1 cm long, after which the body (strobilus) of the parasite is located, consisting of individual segments (proglottids). In the initial sections of the tapeworm's body, the width of the segments prevails over the length, while towards the end the length of the segments, on the contrary, prevails over the width.
Each mature segment usually has a length of 11 to 15 mm and a width of 6-7 mm. The short neck of the tapeworm performs a “body-forming” function (by budding).
The pork tapeworm is a hermaphrodite, that is, one individual contains both male and female reproductive organs. During the growth of the worm, male genital organs are formed first, and then female ones. There are no genitals in the front of the body. Sexually mature hermaphroditic proglottids appear only in the middle of the body.
By the end of the body, all the genital organs of the helminth disappear, leaving only the uterus filled with worm eggs. Mature end segments are able to separate from the body of the parasite and exit into the environment along with feces.
All helminths of the tapeworm class lack digestive, circulatory and respiratory systems. The worm's shell is made up of the tegument, roughly speaking, the “skin” of the helminth. The tegument has not only a formative and barrier function, but also a digestive one.
The worm feeds over the entire surface of the body through pinocytosis (absorption of useful elements through special holes located on the tegument). The tegument also secretes a special enzyme onto the surface of the body, which protects the helminth from digestion in the host’s intestines.
The muscular membrane of the pork tapeworm is represented by two layers - outer (circular) and inner (longitudinal). The excretory system consists of several longitudinal trunks, interconnected by bridges at the end of each segment. In the terminal segment, the excretory system is represented by one common opening. The nervous system consists of 6 to 12 cords running along the body and connected to each other by commissures.
Treatment
Neurocysticercosis can be cured using conservative or surgical methods. Often, drug therapy includes an antiparasitic drug and medications for symptomatic therapy.
Since one of the main symptoms of the disease is seizures, anticonvulsants are prescribed first. Patients whose parenchymal form is in the acute stage are prescribed albendazole. This drug belongs to the group of anthelmintics and is taken for up to 28 days in combination with dexamethasone. But in the case of the development of encephalitis, antiparasitic drugs should not be taken. Since the released toxins will only worsen the patient’s condition. In this case, it is recommended to use corticosteroids.
The larvae are surgically removed from the ventricular cavity. Afterwards, shunts are placed inside them for better outflow of cerebrospinal fluid and to avoid recurrence of intracranial hypertension.
What do you need to remember?
- Neurocysticercosis is a serious disease with severe damage to the central nervous system.
- The reason is the pork tapeworm and the eggs of this helminth, which enter the body with poorly processed food, dirty hands and water.
- Main symptoms: convulsions, blurred vision, impaired movement and sensitivity in the limbs, hallucinations, intracranial hypertension.
- The main diagnostic methods include: ELISA, CT, MRI, general blood test.
- Conservative treatment includes anticonvulsant drugs and corticosteroids, and surgical treatment includes placement of an intraventricular shunt.
- The prognosis of the disease depends on the form of the disease and the duration of human infection with pork tapeworm.
Literature
- “Helminth infections of humans”, ed. F.F. Soprunova - M., “Medicine”, 1985
- Zaplotnaya A.A. CNS lesions caused by cestodes: neurocysticercosis / A.A. Zaplotnaya // News of medicine and pharmacy. - 2010. - No. 330. - P. 37-42.
- Ozeretskovskaya N.N., Zalnova N.S., Tumolskaya N.I. “Clinic and treatment of helminth infections” - M., “Medicine”, 1984.
- "Nervous diseases" ed. prof. E.I. Guseva - M., “Medicine”, 1988.
- Neurocysticercosis – a review / Ansari JA // Kathmandu University Medical Journal. - 2003. - Vol. 1, No. 1. - P. 48-55.
- Del Brutto OH, Sotelo J. Neurocysticercosis: an update // Rev. Infect. Dis. - 1988. - Vol. 10. - P. 10751087.
- Grisolia JS, Wiederholt WC CNS cysticercosis // Arch. Neurol. - 1982. - Vol. 39. - P. 540544.
- Garcia HH, Gonzales AE, Evans CAW, Gilman RH Taenia solium cysticercosis // Lancet. - 2003. - Vol. 362. - P. 547–556. Dixon HBF, Lipscomb FM Cysticercosis: an analysis and followup of 450 cases // Med. Res. Counc. Spec. Rep. Ser. - 1961. - Vol. 299. - P. 158.
Fact 8: Diagnosis of neurocysticercosis in rural areas is difficult
Currently, computed tomography (CT) is required for diagnosis of suspected neurocysticercosis. Appropriate equipment is usually not available in rural areas where the disease is particularly common, making it difficult to identify and treat patients. It is important to combat the parasite by identifying and treating affected people, thereby reducing the likelihood of transmission.
WHO/A. Craggs