Learn more about diseases starting with the letter “D”: Debility, Double-wave viral meningoencephalitis, Dementia with Lewy bodies, Depressive neurosis, Dermal sinus, Cerebral palsy, Jacksonian epilepsy, Diastematomyelia (diplomyelia), Discogenic myelopathy, Dystrophic myotonia Rossolimo-Steinert-Kurshman, Diabetic encephalopathy, Dyscirculatory encephalopathy, Diffuse axonal damage to the brain, Benign rolandic epilepsy.
Diffuse axonal brain injury is a condition caused by severe traumatic brain injury. Its hallmark is axonal tears or diffuse breaks. After an injury, damage to stem cells is typical, which leads to a lack of ability for mental activity, that is, to a person’s vegetative state.
It is possible to get rid of the coma condition primarily with the help of artificial ventilation, as well as intensive care. Usually, after waking up from a coma, doctors prescribe a number of drugs of different types to completely restore the body. These include nootropic, vascular and metabolic drugs.
Another mandatory requirement that the patient must comply with is therapeutic exercises. In other words, physical education, impact on the psyche and restoration of full speech thanks to the help of speech therapists and special exercises.
General information
For the first time among traumatic brain injuries, diffuse axonal brain injury was recognized as a separate type of disease since 1956. The official name, which it has retained to this day, appeared only in 1982. The condition experienced by a person while in a coma has a special name - comatose.
Scattered axonal breaks and small foci of hemorrhage among cerebral structures are the morphological substrate of the comatose state.
The most common areas of the brain where injury occurs are the corpus callosum, brainstem, hemispheric white matter, and periventricular areas. It is typical that this disease is slightly more common in young people and children. Unfortunately, in the second case, this disease occurs in a more serious form with deep coma and additional disorders in the field of neurology.
There is a division of DAP into several types, depending on the severity:
- Mild degree. Coma lasts between 6-24 hours.
- Moderate degree. The coma lasts about a day. There are no or only slight stem damages.
- Severe degree. It is characterized by a long period of time in a coma, during which decerebration and decortication are possible.
Regardless of the degree of DAP, this disease poses a great threat to humans, which threatens a vegetative state or, in the worst cases, death. Therefore, it is clear that many areas of science and medicine, such as neurology and traumatology, are interested in establishing the most effective treatment methods.
Causes and morphology
Many patients do not have a skull fracture or any other visual damage due to the fact that such injury is not always accompanied by direct contact of the head with a hard object.
Vascular damage with the formation of hemorrhages in the brain substance is caused by acceleration in the sagittal plane. Most often, DAP occurs after car injuries, falls from great heights, and also after injuries associated with changes in pressure.
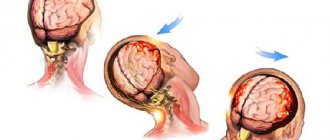
The most mobile hemispheres, as statistics have shown, manifest themselves in rotation, while the fixed stem sections are subject to torsion. A fairly common occurrence in such injuries is mutual displacement of individual layers or parts of the brain. Even a slight displacement of cerebral structures can lead to partial or complete rupture of small vessels and axons.
There are three main symptoms of diffuse axonal damage:
- focus of injury in the corpus callosum;
- lesion in the brain stem;
- diffuse axonal breaks.
The lesion in the corpus callosum, as well as the lesion in the brain stem, initially appears as microscopic injuries and manifests itself in hemorrhage, the size of which is approximately 5 mm. There are often cases where such lesions look like tears in the tissue, the edges of which are soaked in blood.
After some time (about 2-3 days), such places turn into pigmented areas, the color of which resembles rust, and then painful scars form from them. In addition, lesions in the corpus callosum may be accompanied by a phenomenon such as cyst formation.
The main issue is the identification of diffuse axonal damage, which is carried out through special microscopic studies of brain tissue. Such studies include the immunohistochemical method and silver impregnation.
Such studies make it possible to see multiple axonal balls, which are located at the sites of rupture of nerve fibers. All subsequent changes will be expressed in a macrophage reaction with the appearance of reactive microgliocytes and astrocytes.
DAP is very different from a simple brain contusion; its difference lies in the absence of segmented elements. After 2-4 weeks, fragmentation and demyelination of damaged axons will be added to the symptoms of the disease.
Diffuse axonal injury
In 1956, pathologist Sabina Strich published the results of studies of macroscopic specimens of the brain of patients who had been in a post-traumatic vegetative state for a long time (up to 1.5 years).
These were soldiers who suffered in the American-Korean War and were in the hospital with a diagnosis of severe traumatic brain injury. However, at autopsy, no macroscopically detectable signs of brain injury were found in 15 of the deceased. Only signs of atrophic changes in the brain, which are not typical for people at such a young age, were noted. Histologically, diffuse myelin degeneration was detected in the white matter.
The detected changes, according to S. Strich, could be explained by the primary rupture of axons immediately at the time of injury. Despite the fact that after the appearance of this publication, Strich's conclusions were met with skepticism from many of her colleagues, today diffuse axonal injury (DAI) is recognized as one of the leading causes of death in traumatic brain injury: according to the National Institute of Health Traumatic Coma Data Bank (USA). ), the incidence of DAP is 28‒55% of all severe TBI. Mortality for different degrees of severity of DAP ranges from 47 to 70%. Diffuse axonal injury is the cause of death in 35% of victims with severe TBI.
Further research in this area revealed the mechanisms of occurrence of DAP, its typical pathophysiological, clinical and radiation manifestations, which we will talk about today.
Mechanism of damage
In TBI, the force affects bone, soft tissue, vascular structures and the brain substance itself. Of these, it is the GM substance that has the lowest tolerance to tensile forces, which is why, firstly, damage to brain tissue is more pronounced when exposed to tensile forces than compression, and secondly, DAP can occur in the absence of a direct blow - under the influence of forces inertia, and thirdly, it can be observed without damage to soft tissue and bone structures. An example would be a passenger wearing a seat belt during an accident: even if there was no direct impact to the head, his head is subjected to a strong inertial “impact” during sudden braking.
What happens when force is applied? When subjected to impacts or inertial influences, the brain makes movements in the sagittal, vertical and horizontal planes. Rotational impact is considered especially dangerous.
In this case, the fibers that are most susceptible to tension and twisting will be damaged first, namely:
- at the border of the cortex and white matter. The gray and white matter of the GM have different fluid contents, and at the moment of impact, the more plastic white matter is displaced relative to the denser gray;
- around the ventricles of the brain. Previously, it was believed that cerebrospinal fluid and the ventricles of the brain should cushion brain damage, rather than cause it. However, the use of DAP models that are closer to the real brain has made it possible to establish that the turbulent flow of fluid at the time of injury leads to the appearance of “waves” in the boundary layer of the white matter, which leads to rupture of axons in the periventricular zones;
- areas in which long axons are concentrated connecting the cerebral cortex with subcortical structures and the brain stem. In the event of a large impact, the cerebral hemispheres undergo rotation relative to the fixed brainstem sections, and even a slight displacement of the brain can be sufficient to rupture nerve fibers, synapses and blood vessels. It is in these areas that macroscopic changes characteristic of severe DAP are revealed—fine-focal tears with hemorrhages in the corpus callosum and small-focal hemorrhages in the anterior parts of the brain stem.
Figure 1 | Typical localization of axonal lesions (black circles) and hemorrhagic foci (shaded areas). K. Bostrom, C. G. Helander (1986).
The classification of diffuse axonal brain damage is based on the characteristic localization of damage (Adams J. N., 1989), which is often used by pathologists and radiation diagnosticians:
Type I - axonal damage in the white matter of both hemispheres of the cerebrum, corpus callosum, brain stem and cerebellum;
Type II - in addition to the described changes, there are local lesions in the corpus callosum;
Type III - in addition to the listed changes, there are local lesions in the dorsolateral areas of the rostral parts of the brain stem.
It is not difficult to guess that the “higher” the type of damage, the more likely the patient’s condition is more severe and the more likely the force was applied.
The classic cause of traffic accidents is considered to be road accidents that occur at high speed. However, similar injuries have also been described in athletes (football players, hockey players and soccer players colliding with each other and with obstacles) and even in the form of a “baby concussion symptom” - as a result of shaking movements when trying to “rock” the child.
Radiation manifestations
Radiography
Classic radiography is unable to detect DAP.
Computed tomography
Computed tomography without contrast is often performed in patients with TBI, but unfortunately has low sensitivity to DAP (59–80% of patients will have a normal CT image).
Manifestations include:
- round/oval foci of altered density, located diffusely in areas of characteristic localization (cerebellum, cerebral peduncles, corpus callosum, periventricularly and in the hemifserae at the border of white and gray matter);
- hemorrhagic lesions are better visible on CT - they will look hyperdense. Lesions without hemorrhage are hypodense, the latter are detected extremely rarely;
- foci of axonal damage may not be detected during examination immediately after the patient’s admission, but become visible several days after the injury;
- in addition to the actual foci of damage, cerebral edema may be observed in the form of loss of differentiation of gray and white matter, narrowing of the ventricles, prolapse of the cerebellar tonsils into the foramen magnum (must be differentiated from Arnold-Chiari syndrome - the symptoms of edema are temporary);
You can also observe other changes characteristic of TBI: hematomas, including subdural ones, disruption of the integrity of the skull bones, etc.
Figures 2 and 3 show typical changes found on CT scans.
Figure 2 | A 9-year-old boy who survived a traffic accident. A CT scan performed on the day of injury showed several hyperdense foci in the left frontal lobe. Figure 3 | CT scans show several hyperdense lesions, the largest in the left frontal lobe. Signs of swelling of the brain. Magnetic resonance imaging
MRI is the method of choice for diagnosing DAP.
The damage will manifest itself as follows:
- multiple foci of enhancement on T2-weighted images (T2WI) and FLAIR of characteristic localization represent non-hemorrhagic foci;
- hemorrhagic lesions appear hyperintense on T1WI;
- The SWI sequence is considered one of the most informative: the resulting images are sensitive to hemoglobin breakdown products, and hemorrhage areas will be characterized by a “loss” of signal. (Fig. 5);
- DWI-weighted images show limited diffusion in this area.
Figure 4 clearly demonstrates the higher specificity of MRI for DAP compared with CT—compare with Figure 3 (same patient).
Figure 4 | Well-visible foci in the frontal lobe and in the trunk of the corpus callosum, as well as a zone of altered hyperintense signal at the border of the pons and medulla oblongata.
Figure 5 | Hemorrhagic foci are well detected in SWI mode.
Sources:
Meythaler JM et al. Current concepts: diffuse axonal injury–associated traumatic brain injury //Archives of physical medicine and rehabilitation. – 2001. – T. 82. – No. 10. – pp. 1461-1471.
Lebedev V.V., Volkov P.V. Diffuse axonal damage to the brain // Neurosurgery. – 2005. – No. 3. – pp. 10-15.
Ezaki Y. et al. Role of diffusion-weighted magnetic resonance imaging in diffuse axonal injury //Acta Radiologica. – 2006. – T. 47. – No. 7. – pp. 733-740.
Symptoms
A feature of DAP that distinguishes it from all other types of traumatic brain injury is the immediate transition to coma. Basically, it has a long, moderately calm or deep character. It occurs immediately after injury.
If we look at the statistics for adults, the cases of moderate coma are 63% versus 37% deep. In children, the readings vary much less: 43% to 57%. As for the average amount of time a person spends in a coma, it ranges from 3 to 13 days.
Signs characteristic of coma include occasional motor agitation and activity in certain parts of the body or organs, as well as tonic reactions.
Stem symptoms include:
- disturbance of the respiratory process and its rhythm;
- anisocoria;
- different locations of the pupils relative to the horizontal and reduction;
- complete absence of photoreaction and corneal reflexes.
In the field of neurology, symptoms of coma include:
- variable and inconsistent nystagmus;
- lack of response of the muscles of the back of the head;
- irritation of the meninges, that is, Kernig's sign.
Autonomic symptoms have many different manifestations, the most common of which are hypersalivation, hyperhidrosis and arterial hypertension.
DAP is also characterized by significant disorders in motor functions. Their most common manifestation is pyramidal-extrapyramidal tetrasyndrome. This is due to the fact that patients’ hands generally lie in a position called “kangaroo paws” - arms with hanging hands attached to the patient’s body and bent at the elbows.
It is not surprising that tendon reflexes decrease and then may disappear altogether, despite the fact that they are exaggerated at the beginning. Also, coma is characterized by foot signs that are pathological in nature. Disorders in body dynamics and muscle tone can vary greatly in each patient: from generalized hypotension to hormetonia. During the coma they often change and are not stable. Muscle tone is characterized by an asymmetrical and dissociative character.
Outcome options
If a patient manages to survive diffuse axonal damage, then his disease can develop in only two different directions:
- Coming out of a coma. In this case, recovery from the disease is accompanied by the opening of the eyes, however, there is tracking and fixation of the gaze. This phenomenon can occur either spontaneously or due to extraneous factors, sound or pain stimuli. Over time, the patient’s condition normalizes, consciousness is restored, and it gradually becomes possible to carry out any simple instructions and actions, and verbal contact develops. In addition, such processes are necessarily accompanied by a slow regression of neurological manifestations.
- Transition to a vegetative state. Being in a long-term coma leads to a transition to a vegetative state. The duration can range from 1-2 days to several months. This situation has a persistent and transient nature. A vegetative state can be judged by the opening of the eyes without tracking or any fixation of gaze. In this case, variable, changing focal symptoms appear - separation of the stem and hemispheric structures. With a prolonged and persistent vegetative state, vegetative-visceral disorders begin to appear, such as tachycardia, hyperthermia, and facial flushing. Most often, the appearance of such symptoms is due to damage to somatic organs and intercurrent infections. Also, in a vegetative state, neurotrophic disorders develop, mainly bedsores.
Diffuse axonal brain injury
A distinctive feature of DAP, in comparison with the clinical picture of other TBIs, is a long-term moderate or deep coma that occurs immediately after injury. In adults, the ratio of cases of moderate to deep coma is 63% to 37%, in children - 43% to 57%. The average duration of coma varies from 3 to 13 days.
Typical for coma with DAP are postural-tonic reactions of a diffuse nature, provoked by various stimuli, periodic motor excitation against the background of adynamia. Stem symptoms are characteristic: decreased or complete loss of photoreaction and corneal reflexes, anisocoria, different horizontal positions of the pupils, disorder of the respiratory rhythm and respiratory rate. In addition, the neurological status often reveals variable spontaneous nystagmus, stiffness of the neck muscles and Kernig's sign, vegetative symptoms (hyperhidrosis, arterial hypertension, hypersalivation, etc.).
Movement disorders are usually represented by severe pyramidal-extrapyramidal tetrasyndrome. In most victims, the arms with hanging hands are brought to the body and bent at the elbows (the so-called “kangaroo paws”). Tendon reflexes are initially increased, then decrease or disappear completely. Pathological foot signs often occur. Muscle tone disorders range from generalized hypotension to hormetonia, are prone to change, and are often asymmetrical or dissociative in nature.
Outcome options for diffuse axonal injury
In surviving patients, the further course of DAP can go in 2 directions: exit from coma and transition to a vegetative state. In the first case, the opening of the eyes begins to occur, accompanied by tracking and fixation of the gaze. It can be either spontaneous or provoked by various stimuli (sound, pain). Consciousness is gradually restored, simple instructions can be followed, and verbal contact expands. This process is accompanied by a slow regression of neurological manifestations.
A prolonged coma in most cases leads to a transition to a vegetative state, which can be persistent or transient and last from 1-2 days to several months. The onset of a vegetative state is indicated by the opening of the eyes, which is not accompanied by fixation of gaze and tracking. Signs of separation of the hemispheric and brainstem structures appear - variable, unusual, changing focal symptoms. In persistent vegetative states, neurotrophic disorders (including bedsores) and vegetative-visceral disorders (tachycardia, hyperthermia, facial hyperemia, tachypnea, etc.) develop. A significant role in the occurrence of the latter is played by damage to somatic organs (multiple organ failure) and intercurrent infections (pneumonia, pyelonephritis, sepsis) that appear as a complication.
Diagnostics
There are a number of signs by which specialists are able to identify diffuse axonal damage in patients:
- mechanism of the resulting traumatic brain injury with angular acceleration of the fall;
- onset of coma immediately after injury;
- characteristic features of clinical symptoms;
- absence of congestive changes in the optic discs.
Despite these signs, doctors experience great difficulty in identifying this disease.
To correctly diagnose DAP, it is necessary to conduct a magnetic resonance or computed tomography scan of the brain. With this disease, when these studies are carried out in the acute period, cerebral edema is determined with a decrease in the ventricles and subarachnoid spaces.
In addition, the disease is often accompanied by an accumulation of fluid over the frontal lobes. The greatest difficulty is in diagnosing mild and moderate diffuse axonal damage, in which, as a rule, there are no visible pathologies: microscopic signs are not observed, cerebral edema, and hemorrhages are insignificant.
If the tomographic picture does not differ from that of a healthy person, specialists are guided by typical tomographic dynamics, that is, regression of hemorrhages and edema with a tendency to dilation of the ventricles, followed by ventriculomegaly, as well as an increase in diffuse atrophy of cerebral structures.
Diffuse axonal injury (DAI)
Diffuse axonal injury ( DAI ) is a severe form of traumatic brain injury caused by shear forces. Diffuse axonal injury is potentially difficult to diagnose because findings may be subtle on CT scans, but can result in severe neurological impairment.
As a diagnostic, the best modality is magnetic resonance imaging, in which diffuse axonal damage manifests itself in the form of several small areas of magnetic susceptibility artifacts surrounded by a zone of hyperintense MR signal on FLAIR images, localized at the border of gray and white matter, in the corpus callosum, and in severe cases in brain stem.
Pathology
Diffuse axonal damage is the result of exposure to shear forces arising during rotational acceleration (less commonly, braking). Due to the different densities (relative mass per unit volume) of white and gray matter, the shift occurs predominantly in axons at the border of gray and white matter, which is what the name of the pathology reflects. In most cases, these forces also lead to cell damage, which is manifested by edema. But complete rupture of axons occurs only in severe cases.
Clinical picture
Patients with diffuse axonal injury typically lose consciousness at the time of the incident. Post-traumatic coma can last a considerable time and is often a manifestation of concomitant visualized injuries (eg, cerebral contusion). Often, the diagnosis of DAP begins when, contrary to expectations, the patient's signs of neurological deficit do not disappear.
Diagnostics
Diffuse axonal injury is characterized by multiple foci of damage with a typical distribution, typically at the gray-white matter interface, in the corpus callosum, and in severe cases in the brainstem.
CT scan
Non-contrast computed tomography of the brain is a routine procedure in patients with traumatic brain injury. Unfortunately, CT is not sensitive in the diagnosis of occult diffuse axonal damage, and patients with a relatively normal CT picture may have severe neurological deficits unexplained by the CT picture [4, 5].
The CT picture depends on whether the hemorrhage is visible or not. The hemorrhagic lesion will be hyperdense, varying in diameter from a few millimeters to several centimeters. Non-hemorrhagic damage becomes more clearly visible due to the swelling that develops around it after a few days. It may be associated with significant and disproportionate cerebral edema.
Computed tomography is virtually insensitive to non-hemorrhagic lesions and can detect up to 19% of such lesions, compared with 92% of lesions detected on T2-weighted images [4].
Magnetic resonance imaging
MRI for suspected diffuse axonal damage is the modality of choice, even in the presence of a completely normal CT picture [5-6]. MRI, especially with SWI or GRE sequences, is extremely sensitive to hemoglobin breakdown products and can detect small areas of magnetic susceptibility artifacts at the gray-white matter interface, corpus callosum, or brainstem.
Some lesions may be nonhemorrhagic (even when using high field strength SWI sequences).
The degree of surrounding edema usually increases after a few days, although post-traumatic FLAIR changes have largely resolved after 3 months [7]. In contrast, changes on the SWI take much longer to resolve, although significant resolution is also observed at 12 months after injury [7]. Typically, swelling from DAP resolves more quickly than swelling from hemorrhage.
It is important to note that even with modern high-field scanners, absence of change cannot be used with high accuracy to exclude diffuse axonal damage.
MR spectroscopy
MR spectroscopy may have advantages in identifying patients with grade I damage who may be asymptomatic on other sequences. Signs are an increase in the choline peak and a decrease in the N-acetylaspartate peak [3].
Differential diagnosis
- contusion of the cerebral cortex is the first in the differential series in patients with TBI
- localized superficially involving the cortex (rather than the gray-white matter boundary) and is usually associated with volume-variable extra-axial blood collection (traumatic subarachnoid hemorrhage, subdural hematoma)
- amyloid angiopathy
translation of Radiopaedia publication 05/18 [8]
Treatment
The main treatments needed by patients with diffuse axonal injury are continuous mechanical ventilation, nutritional routes that do not involve the gastrointestinal tract, and intensive care. Its goal is to support and restore homeostasis, eliminate cerebral edema, as well as all major systems and functions of the body. Naturally, such therapy should prevent the occurrence of any infectious diseases. There are cases of severe complications in the functioning of motor functions. Then doctors resort to using anesthesia.
The first thing that needs to be done after emerging from a coma is an accelerated reduction in deviations associated with mental and emotional health. This can be achieved with psychostimulotherapy.
Exercise therapy will help restore the muscles and motor system of the body, and will prevent joints. Often, after recovering from a coma, the help of speech therapists is needed to correct speech.
Restoration of the central nervous system occurs through the use of drugs intended for this purpose: nootropic and vascular.
The first include piracetam, nicergoline, cortexin and gamma-aminobutyric acid, the second - cinnarizine and vinpocetine. If the patient has certain characteristics during the recovery period, then neurotransmitters (levadopa and piribedil) and anticholinesterase drugs (galantamine and neostigmine) are added to his treatment.
As for contraindications, surgical procedures are strictly not recommended. Doctors allow surgical intervention only if there is a danger of compression of the brain. Such a threat may arise in connection with intracranial injuries, for example, crush lesions, intracranial or subdural hematomas, depressed skull fractures.