What brain diseases are visible on MRI?
A set of symptoms for which magnetic resonance imaging of the head is prescribed:
- Decreased breathing;
- Vomiting reflex;
- Loss of vision, speech;
- Unsteadiness of gait due to damage to the cerebellum;
- Twitching pupils;
- Strabismus;
- Lack of swallowing reflex;
- Difficulty in excreting feces;
- Periodic loss of consciousness;
- Frequent headaches.
The described clinical manifestations may be a consequence of brain contusion, traumatic brain injury, stroke, or severe head impacts.
The advent of MRI scanning made it possible to diagnose pathological changes in multiple sclerosis (destruction of the myelin sheaths of the nerves). After a bruise, headaches appear at a late stage, when pronounced microcirculation disorders occur. Contacts at the sites of destruction of nerve fibers cause a “short circuit” with subsequent neurological symptoms. Extensive disruption of nerve innervation is accompanied by vasoconstriction. Abnormal microcirculation provokes headaches, muscle disorders, visual and auditory disorders.
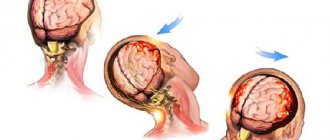
Computed tomography for traumatic brain injury
Computed tomography in traumatic brain injury.
Traumatic brain injury (TBI)
– a collective concept that includes various types and severity of mechanical damage, both to the skull itself and to intracranial formations: meninges, brain tissue, cerebral vessels, cranial nerves.
Traumatic brain injury (TBI) is one of the most common types of injuries and accounts for up to 40% of all types of injuries and, according to statistics from the World Health Organization, tends to increase by 2% per year.
Mortality in general with TBI is 5-10%, and with severe TBI it reaches 70%. Mortality from traumatic brain injury accounts for 1% of total mortality.
The average age of most victims is 20 – 50 years, i.e. during the period of greatest working capacity, while there are 2.5 - 3 times more men than women.
Among the causes of traumatic brain injuries, the first places are occupied by domestic and road traffic injuries, followed by sports injury, work injury, and secondary injury due to a patient fainting, epilepsy, and stroke.
The majority of victims (up to 60%) experience decreased performance and disability as a result of their injuries.
The frequency of traumatic brain injury and the severity of its consequences give the problem great social significance.
According to the degree of integrity of the head tissues, they are distinguished:
Closed craniocerebral injury - preservation of the integrity of the soft tissues of the head or the presence of a soft tissue wound that does not affect the aponeurosis of the skull. Open traumatic brain injury is the presence of injury to the soft tissues of the head, including, at a minimum, damage to the aponeurosis of the skull, and also possibly involving deeper formations (vault and base of the skull, membranes, brain tissue).
Penetrating traumatic brain injury - in which there is damage to the dura mater (both in the presence of a head wound and in its absence).
Non-penetrating traumatic brain injury in which the dura mater remains intact.
Based on the nature and severity of damage to the brain substance, the following clinical forms of TBI are distinguished:
- brain concussion,
- brain contusions of varying severity,
- diffuse axonal damage,
- compression of the brain,
- compression of the head,
- combined form.
Diagnosis of traumatic brain injury is based on medical history, clarification of the circumstances and mechanism of injury, identification of the classic anamnestic triad: loss of consciousness, nausea or vomiting, amnesia. Then a thorough external examination, neurological examination and additional research methods are performed.
Modern non-invasive diagnostic technologies (CT, MRI, ultrasound, PET) have made a real revolution in deciphering the pathoanatomical substrate of TBI, surpassing routine X-ray examination of the skull and brain in terms of information content, and are crucial for determining the nature of injuries and developing further tactics for managing these patients.
Applications of computed tomography
in neurotraumatology has significantly changed the understanding of the possibilities of diagnosing various traumatic brain injuries. CT is currently the “gold standard” - the most informative method for examining patients with traumatic brain injuries and allows one to judge in the shortest possible time the mechanisms of brain damage, its nature, prevalence, severity of edema and dislocation of the brain, as well as the dynamics of these changes.
CT allows you to consistently study the soft tissues of the head, skull bones, brain matter, epidural, subdural, subarachnoid spaces, basal cisterns and ventricles of the brain:
- detect fractures of the vault and base of the skull (with a sensitivity much higher than traditional radiography),
— identify the presence of an intracranial hematoma (its nature, location, size),
- identify the presence of a focus of brain contusion (its localization, size, nature, presence of a hemorrhagic component),
— determine the degree of compression or dislocation of the brain by a volumetric process,
- identify the presence of diffuse or perifocal edema and its degree,
- detect subarachnoid hemorrhage,
- identify intraventricular hematoma,
- detect the presence of pneumocephalus.
Therefore, at present it should be considered a rule that, if appropriate equipment is available, a computed tomography scan is necessary first. The only question is the timing of this study: for victims with severe TBI, especially in unclear cases, CT should be performed according to urgent indications; for mild TBI, CT can be performed as planned, but not later than the next day.
CT with intravenous contrast (CT angiography) is usually not performed for emergency indications. The indication for such a study is the detection on native tomograms of intracerebral hematomas localized in places of possible rupture of the aneurysm.
Visualization of minimal amounts of fresh blood poured out, its confident differentiation from other extracellular fluids, monitoring the dynamics of edema and swelling of the brain, necrosis and restoration of its structures, while simultaneously recognizing fractures of the skull bones, especially its base, are the advantages of CT over magnetic resonance imaging.
In addition, the positive aspects of this neuroimaging method are the short research time, the possibility of fixing the patient and using ventilators, and fewer contraindications to the examination, which is impossible with technically more complex MR imaging.
MRI of the head for injuries and bruises
Brain symptoms after bruises and injuries are varied. Manifestations depend on functional and organic changes in the brain matter. A mild concussion is rarely accompanied by loss of consciousness. More often, after a bruise of the skull, headaches, vomiting, and nausea appear. After a few weeks, the symptoms disappear on their own. The course of the pathology is monitored by neurologists.
Complications of a concussion are minor hemorrhages inside the subarachnoid space. Brain hyperintense lesions on MRI are limited. Enhanced spots after a concussion are combined with areas of normal or reduced signal. Dynamic observation allows you to visualize the normalization of the condition. The pathology persists when the vessel ruptures or the vascular wall dissects (aneurysm).
Complications after a concussion are clearly verified by MRI. A moderate bruise is characterized by fever, difficulty breathing, cardiac arrhythmia, twitching of the pupils, and loss of sensation in the limbs. Ocular nystagmus is accompanied by a movement to the right and left, which for a neurologist is a sign of damage to brain tissue.
Severe problems of intracerebral microcirculation occur when hemorrhage penetrates the brain parenchyma. With proper treatment, changes pass quickly.
Contrast MRI for severe concussion evaluates the condition of blood vessels, ventricles, and allows one to study the size of the pathological focus and location.
A severe contusion of the brain is accompanied by a blockage of the bronchial tubes due to damage to the corresponding center. Lack of oxygen supply, concomitant arterial ruptures, and aneurysms lead to muscle cramps and paresis of the limbs due to suppression of functional brain centers.
Severe brain contusion can lead to fractures and extensive hemorrhages. Intense brain lesions on MRI occur due to the accumulation of blood within the subarachnoid space. The heterogeneous density of magnetic resonance imaging is characterized by the appearance of dark and white areas in the images. Hyperintense spots do not have clear boundaries. Images indicate swelling and accumulation of blood clots.
A repeat MRI for a concussion is done after 40 days. By this time, the swelling disappears and the headaches disappear. A long course of the disease is expected with a skull fracture with increased intracranial pressure.
Should I treat it or will it go away on its own?
There is a big risk that it won't work. How do you like the prospect of terrible headaches for life, deafness, decreased vision, brain tumors and other “delights”? To prevent the injury from progressing to such an extent, it needs to be treated. Just don’t prescribe therapy for yourself based on advice from a women’s forum, but go to see a doctor and get a prescription.
At first, you will have to stay in bed, give up strong coffee and tea, put off all household chores until later, and under no circumstances drive. The doctor may prescribe painkillers and sedatives, sleeping pills, and a vitamin and mineral complex. For severe injuries, therapy is recommended to maintain blood vessels, restore nerve tissue, and improve metabolism. You should not ignore the appointment, because it is better to become an obedient patient for a week than to suffer the consequences for the rest of your life. And if a brain contusion is diagnosed, then it is better to agree to hospitalization. A bruise is dangerous not only for health, but also for life.
Venous and arterial aneurysms on MRI scans
Aneurysmal dilations of blood vessels have a special morphology - neck, body, dome. The cause of the disease is deposits of fatty complexes inside the vascular wall. The disease is called atherosclerosis and causes many complications in the brain and heart. Damage to the wall leads to disruption of permeability. Blood entering the interstitium causes dissection. Clots and formed elements accumulate between the individual layers. The movement of blood creates pressure on the thin wall. At a certain point, the vessel may not hold up. The appearance of a small rupture is accompanied by hemorrhage. Massive bleeding leads to death.
Contrast MRI for brain aneurysm is the best option for diagnosing the pathology. Tomograms reflect the full morphology - saccular, fusiform expansion of the arterial wall. Even a native MRI scan can reliably verify an aneurysm. Contrast improves visualization.
Tomograms show the size of the aneurysm. Formation over 10 mm is dangerous due to rupture.
Practical features of MRI of aneurysm after trauma:
- The spatial structure and relationships of individual parts are revealed by MR angiography. A bolus injection of contrast agent creates a clear image of the arteries and veins;
- Thrombosed and non-thrombosed aneurysmal dilatation is identified by taking multiple sections. The 3D modeling mode allows you to build a spatial projection of an object. The procedure helps determine the shape and size of the aneurysm;
- A combined study (CT and MRI) after head injuries allows you to diagnose thrombosed areas of the artery, measure the length of the neck, and verify the dimensions.
After severe trauma, angiography is performed to study the spatial relationships between various physiological and pathological formations. Magnetic resonance neuroimaging is performed to verify rupture, thrombosis, and aneurysmal dilatation of the artery. The study additionally reveals a whole list of pathologies.
Spasmodic contractions of arteries and veins of individual brain segments are diagnosed using a combination of methods - MR angiography, CT angiography, catheterization angiography. On the recommendation of a radiology doctor, additional examinations (MR spectroscopy, tractography) may be prescribed.
Ambulance
It is unlikely that you will be able to rub the bruised area and lie down for a couple of days after a head injury. In such a situation, it is better to take the victim to the nearest hospital for an x-ray, or even better, do an MRI of the brain. The fact is that fluoroscopy will only show damage to the bones of the skull, while tomography will show the condition of the bones, blood vessels, nerves, and the brain itself.
True, even city municipal clinics are still not equipped with MRI machines, and village emergency rooms don’t even dream of them. Therefore, if trouble happens to you at your dacha, you will have to go to Moscow. But you can always take advantage of the delights of civilization, that is, your smartphone or tablet. On our website you will find a list of all capital clinics equipped with a tomograph. Many of them work around the clock. So even if the problem appeared at night, you can immediately get examined. At this time of day it is usually even easier - there is no such flow of people interested, you can get a discount. The price of MRI of the brain in the evening and at night is 10-30% lower. So don't put off your trip until the morning.
Magnetic resonance imaging of a cerebral cyst
A small brain cyst does not pose a danger if located outside the functional centers. Morphologically, the formation looks like a cavity with liquid internal contents. The bubble can remain inside the white or gray matter for life. If it forms after an injury and increases in size, dynamic control of the cavity is required.
Inflammatory cysts are formed by bacteria and parasites (echinococcus, alveococcus). After the infection is suppressed, the formations subside.
Autoimmune cysts gradually progress. Dynamic MRI helps monitor the condition of the bladder. With a growing formation, surgical treatment will be required. The absolute norm against the background of autoimmune damage to brain tissue requires repeated magnetic resonance imaging no later than 1 year.
The formation of antibodies to brain neurons and blood tests for infections are additional ways to verify pathological changes. After an MRI of the aneurysm, laboratory evaluation of cholesterol and blood clotting will be required.
Periodic rises in pressure are dangerous by rupture of cerebral arteries with the development of hemorrhagic or ischemic stroke. Classical MR angiography helps to obtain maximum information about the pathology.
Will an MRI show a concussion?
Magnetic resonance imaging is a method that visualizes the brain substance with a slice thickness of 1 mm. High resolution determines the widespread use of this technology. The doctor receives an accurate image, diagnosis becomes faster, and conclusions are more reliable. MRI shows the following parameters for a concussion:
- brain structure;
- location and size of various areas;
- vascular condition;
- presence of neoplasms, etc.
With a concussion, there is no anatomical damage, and an MRI after the injury will show normal tissue. If the severity of the impact is greater, then a CT scan will be more useful. The method detects a fracture of the skull bones, rupture of a vessel and accumulation of blood (hematoma), as well as other changes. The described complications can be detected with bruise or compression of the brain.
Features of cerebral concussion in children
The first symptoms in children appear early - immediately after the blow. The first signs of a concussion in a child:
- Pale skin;
- Lethargy and weakness;
- Complaints of dizziness;
- Blueness of the skin;
- Noise in ears;
- Cutting inside the eyes.
Suspicion of an intracerebral concussion requires consultation with a neurologist and traumatologist. Specialists will prescribe the necessary types of clinical and instrumental diagnostics:
- Lumbar puncture;
- Computed and magnetic resonance imaging (CT and MRI);
- Echoencephalography;
- Electroencephalography.
During hospitalization, diagnostic methods make it possible to evaluate the effectiveness of treatment with nootropics, sedatives, dehydration therapy, and local hypothermia.
Infants may experience nonspecific symptoms:
- Lack of appetite;
- Frequent regurgitation;
- Irritability and causeless crying;
- Cloudiness of consciousness.
In older children, accompanying symptoms appear:
- Cold sweat;
- Blueness of the skin;
- Stupor and stupor;
- Repeated vomiting;
- Increased pressure inside the eyeballs;
- Intra-ear noise.
Multiple associated symptoms can lead to antegrade and retrograde amnesia.
Complex disorders in pathology:
- Exotropia;
- Oculomotor disorders;
- Gaze paresis;
- Pulse lability;
- Reduced blood pressure;
- Increased temperature (hyperthermia).
Symptoms of a concussion are more difficult to identify in infants. The smaller the baby, the more difficult it is to verify the clinical nosology.