Study in more detail information about various diseases starting with the letter “V”: Vegetative state, Ventricularity, Vestibular ataxia, Vestibular neuronitis, Vibration disease, Viral meningitis, Viral encephalitis, Temporal lobe epilepsy, Intracerebral hematoma, Intracranial tumors of the cerebral hemispheres, Intracranial hypertension, Inflammatory myopathy, Inflammatory polyneuropathy, Congenital myopathy, Congenital paramyotonia, Secondary parkinsonism
Concept
Viral encephalitis is a painful condition of the human body, manifested in inflammatory foci of a diffuse nature, which are localized in the tissues of the brain. The presented disease manifests itself as a result of specific viral microorganisms entering the body. The symptoms of the disease have various types of systemic disorders, all of which are directly dependent on the type of infection and the state of the patient’s immunity. In addition, it is composed of general infectious indications, cerebral manifestations and specific inflammatory foci.
Brief information
Viral encephalitis is a pathological deformation of the components of the main organ of the central nervous system of viral origin. If cerebral surfaces are involved in the dysfunction, then this phenomenon is called meningoencephalitis, and if the deviation progresses to the spinal cord, it is called encephalomyelitis. In addition, there are two forms of the disease - primary (arising due to the entry of a viral agent into the cerebral structures) and secondary (caused by an underlying illness, such as influenza, rubella, etc.), as well as after vaccination depending on the individual sensitivity of the patient.
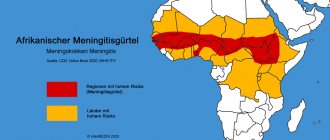
According to average statistical data, the prevalence of the described disease differs significantly depending on the country’s climate and geographical indicators. It is found in Asian areas, America, Europe, etc. Taking into account the features of the pathological process, the complexity of studying the body and the classification of the pathogen, there is a high risk of developing serious complications. Currently, inflammation of this type still continues to be a rather relevant and troubling issue among practicing neurologists.
Herpes viruses are widespread causative agents of various human diseases, among which lesions of the nervous system occupy a significant place. Herpetic neuroinfections cause meningitis and encephalitis, myelitis and various syndromes of damage to the peripheral nervous system. At the same time, identifying viral neuroinfections is associated with diagnostic difficulties, which require large material costs, modern equipment and qualified personnel, so the number of diagnosed infections in leading clinics rarely exceeds 40-50% [21].
The possibilities of new diagnostic methods and the effectiveness of etiotropic antiherpetic drugs attract even more attention to this pathology [1].
Currently, eight herpes viruses are known to be pathogenic for humans, each of which can cause an infectious disease with a characteristic clinical picture and damage to a number of organs and systems (skin and mucous membranes, lymph nodes, organ of vision, liver, lungs) in combination with lesions nervous system. Diseases of the nervous system of a herpetic nature can occur independently, without signs of involvement of other organs.
Herpes viruses can cause intrauterine deformities and fetal malformations, stillbirths, and cause neonatal herpes, a rare severe disease with high mortality [13, 16]. Some of the herpes viruses cause severe cancer (herpes simplex virus type 2 - HSV-2 - cervical cancer; Epstein-Barr virus - primary central nervous system lymphoma, nasopharyngeal carcinoma, Burkitt's lymphoma; herpes virus type 8 - Kaposi's sarcoma in HIV-infected persons). In table Table 1 lists the main human diseases caused by herpes viruses.
All herpesviruses are capable of entering a latent state with periodic reactivation. It is believed that this ability was developed as a result of prolonged contact with the human body and was the main condition for the preservation of herpes viruses as a species. Latency can manifest itself in two qualitatively different states: dynamic
latency in the form of viral persistence with the constant release of a small amount of virus without manifestations of disease and
latency with the manifestation of infection
in the form of persistence of the viral genome with subsequent viral replication and development of the disease.
The evolution of the herpes virus is closely related to its latency as one of the main features of its biological characteristics [20]. Strains of herpes simplex virus type 1 (HSV-1), isolated from geographically distant areas or anthropologically different ethnic groups, turn out to be different in the nature of their genomes.
HSV-1 is so widespread in the population, causing in most cases benign blistering rashes on the skin and mucous membranes, that it was only by the mid-twentieth century that it was recognized that it could also be a cause of severe encephalitis. Skepticism about HSV as an etiological factor of encephalitis was also caused by the statement of the famous scientist C. Levaditi (1922) that the herpes virus is the cause of Economo's lethargic encephalitis, but this opinion was not confirmed [13].
In 1941, M. Smith et al. [18] reported the isolation of HSV from the brain of a child with severe encephalitis. In 1949, W. Haymaker described 3 adult patients with acute sporadic encephalitis in whom HSV was cultured from the brain. Later, the connection between severe encephalitis and HSV was confirmed by numerous studies [7]. A. Nahmias and W. Dowdle in 1968 in the USA determined the incidence of herpetic encephalitis (HE) as 1 case per 1 million people per year. Later, with the advent of new diagnostic capabilities, this figure increased and is now considered to be 4-5 cases per 1 million people per year [13, 19].
In the history of the study of HE, several main stages can be distinguished depending on the methods of verification and treatment used. In the 40-60s of the twentieth century, a number of publications appeared devoted to the description of the clinical picture and pathomorphological changes in this disease. Using the electroencephalography (EEG) method, attempts are made to identify changes specific to GE (focal slow-wave activity, epileptic activity, etc.). A common method for diagnosing HE is the isolation of herpesvirus from diagnostic brain biopsies taken at the sites of its greatest damage, determined using clinical methods and MRI. Isolation of the virus was carried out on tissue cultures, laboratory animals and using electron microscopy. These methods were available only to large university centers in developed countries. The UK HSE Working Group [5] proposed diagnostic criteria for the disease: detection of virus in brain tissue using culture or immunological techniques or clear histopathological evidence of acute necrotizing encephalitis with detection of Lipschutz bodies and/or ultramicroscopic evidence of detection of herpes virus capsids together with serological evidence of infection HSV.
Subsequently, the number of publications describing patients with verified isolation of herpesvirus from the central nervous system and cerebrospinal fluid (CSF) increased significantly. New diagnostic methods have appeared: immunological examination of CSF, isotope scanning, computer (CT) and magnetic resonance (MRI) imaging of the brain.
Currently, virus isolation from patients with HSE is used quite rarely due to its high cost, the length of time it takes to obtain results and the emergence of informative methods - serological testing of blood serum and CSF and molecular biological research (polymerase chain reaction (PCR) and its modifications).
Of the serological methods, the most used is enzyme-linked immunosorbent assay (ELISA), which, by a single determination of the levels of specific immunoglobulins M (IgM) and G (IgG), allows an etiological diagnosis to be made. It is preferable to determine immunoglobulins to HSV not only in the blood serum, but also in the CSF, since in some cases the production of antibodies in the CSF occurs faster than in the blood, and in some patients they can be determined only in the CSF [3].
The PCR method is currently the optimal diagnostic test. In specialized laboratories involved in the diagnosis of GE, its specificity is 100%, and sensitivity is 75-98% [12, 19]. It is rightfully considered the fastest, most sensitive, economical and least invasive method [15], which is widely used in diagnosing and monitoring the treatment of HSV [9].
Determination of HSV DNA in the CSF is comparable in diagnostic value to virus isolation from brain biopsies or intrathecal detection of antibodies to HSV. The results of CSF PCR testing should always be considered in the context of the clinical features of each case. In patients with a low probability of GE based on clinical signs, a pseudonegative PCR result reduces the percentage of correct diagnosis by less than 1%. At the same time, in patients with a high probability of clinical symptoms of GE (MRI, EEG, pleocytosis, etc.), a negative test reduces the likelihood of a correct diagnosis by 5%, but does not completely exclude it. This is important when considering the advisability of interrupting antiviral therapy for GE in the case of negative PCR [19].
It is advisable to use the PCR method in parallel with a serological test of blood and CSF, since 1) the DNA of the virus is determined mainly in the first 10-14 days of illness, and the patient can be admitted and examined at a later date; 2) the PCR method can be pseudonegative or pseudopositive, and parallel testing of antibodies increases the effectiveness of the study [17].
It is known that GE is one of the most common types of encephalitis in temperate countries. Its share is more than 20% in the structure of all viral encephalitis [2, 14]. The incidence of GE occurs evenly throughout the year. Some authors note that the age distribution of cases covers two “peaks”: 1) between 5 and 30 years and 2) over 50 years. About 30% of cases of GE occur in childhood. HSV-1 is detected in 95% of cases, HSV-2 - in 5% [12].
The pathogenesis of GE is heterogeneous. The virus can penetrate the central nervous system through hematogenous and neuronal routes. Typically, in adult patients, GE develops as a result of reactivation of a latent infection. If previously it was believed that the most common route of infection in the pathogenesis of HE was the primary route of infection, now there is more reason to believe that the predominant number of diseases are the result not of a primary infection, but of the activation of a latent virus [13].
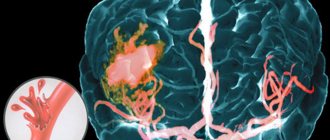
Before the era of the use of acyclovir, pathomorphological changes in HE were so characteristic that often the diagnosis could be made during an external examination of the brain of a person who died from HE. Foci of necrosis in the form of softening or hemorrhagic foci are located mainly in the temporal, frontal, less often parietal lobes, the area of the Sylvian fissure and the insula. Necrosis primarily affects the gray matter, but also extends to the white matter, being located asymmetrically. The boundary between gray and white matter is not clearly visible not only in the temporal, but also in the frontal regions, insula, cingulate gyrus, etc. Numerous hemorrhages are observed in the cortex and underlying white matter [6].
The histological picture in the affected areas reveals the presence of diffuse meningoencephalitis with pronounced infiltration of the membranes and perivascular spaces by lymphocytes and histiocytes. In a number of parts of the brain there are accumulations of glial cells (“glial nodules”). In cells (neurons and glia), intranuclear eosinophilic inclusion bodies (Lipschutz, Cowdry) can be observed [10, 11].
Until recently, studies of the immune system of patients with GE did not reveal serious immune defects. Recently, French researchers from the genetic laboratory of the University of Paris René Descartes [8] published the results of a study of 2 children who were in a related relationship (their parents were cousins) who were sick with HSE. Autosomal recessive inheritance of deficiency of the intracellular protein UNC-93B, responsible for the production of cellular interferons selectively for HSV-1, was discovered. Later, an epidemiological study of children with GE in France showed that 13% of them were blood relatives. Thus, according to scientists, immunodeficiency in GE may be the result of a mutation in a single gene that does not cause impaired immunity to other pathogens, as is observed in most known primary immunodeficiencies. Other severe infectious diseases, according to the authors, may also have similar monogenic immune disorders.
Clinical characteristics of patients with GE
For the period 1971-2008. We inpatiently examined and treated 112 adult patients with GE (74 men and 38 women). The average age of the patients was 37.9±14.8 years. The male:female ratio was 1.9:1. Disease outcomes: 90 (80%) patients remained alive, 22 (20%) died. The distribution of hospitalized patients by year is presented in Fig. 1.
Figure 1. Number of hospitalized patients with herpetic encephalitis by year of observation. The x-axis is years, the y-axis is the number of hospitalized patients.
The main criterion for inclusion in the study group for survivors is a connection with HSV-1 according to immunological and virological criteria in the presence of symptoms of viral neuroinfection (encephalitis). Inclusion criteria for the deceased were clinical signs of acute encephalitis, foci of necrosis in the brain, association with herpes viruses, and the absence of another alternative diagnosis.
In table Table 2 shows the main indicators obtained during the examination of patients with GE.
The onset of the disease in the vast majority of patients was acute with fever and general infectious manifestations, accompanied by general weakness, headache, and respiratory symptoms (cough, runny nose, hyperemia of the pharynx). Patients were admitted on average 8.4±6.8 days of illness. In 2 patients, due to the severity of the condition and the level of impairment of consciousness, it was not possible to determine the day of illness.
The course of GE in most patients can be divided into 4 periods: 1) infectious manifestations - until the appearance of neurological changes (from 1 to 30 days); 2) neurological disorders (from 1 to 50 days); 3) convalescence (from 1 to 12 months); 4) residual effects.
The duration of the infectious period averaged 5.1 (range 1 to 30) days. The duration of the febrile period is on average 12.5 days. In 104 (93%) patients the temperature was high (38-39 °C and above), in 7 patients it was low-grade, and in 1 it was normal. In the acute period, 5 (4%) patients had herpes vesicular rashes on the face. The increase in neurological symptoms in the majority occurred against the background of high temperature, accompanied by increased intoxication and severity of the disease, and averaged 10.6 (from 1 to 50) days.
In patients receiving acyclovir, this period was shorter. In those who did not receive acyclovir, it was violent, manifested by increasing disturbances of consciousness (to stupor and coma), convulsive syndrome and mental disorders (sometimes like delirium). In 8 patients, there was a subacute development of the disease with prolonged malaise, decreased performance, strange behavior, and low-grade fever. In 14 (12.5%) patients, the onset of the disease was an acute cerebrovascular accident with increased blood pressure, epileptic seizures, and impaired consciousness.
Impaired consciousness was detected in 101 (90%) patients: in 70 (62.5%) - consciousness was impaired by the type of confusion, stupor, disorientation in place and time; in 17 (15%) - severe disturbances of consciousness to the level of coma of patients, in 14 (12.5%) - stupor. The soporous and then comatose state most often developed on the 6-12th day of illness, its duration ranged from 3 to 10 days. In 6 of the deceased, a comatose state occurred 1-6 days before death.
Epileptic seizures with tonic and clonic convulsions in the acute period of the disease were observed in 70 (62.5%) patients. In 20 patients, GE debuted with a convulsive syndrome. In 8 patients, seizures were repeated, taking on the character of status epilepticus, in 23 they were repeated during the course of the disease, in 39 they were single. Local (Jacksonian) seizures were observed in 3 people.
Mental disorders occurred in 85 (76%) patients. In 18 people, the disease began with mental disorders, against the background of which neurological symptoms subsequently developed. Patients often experienced hallucinations: more often visual, less often auditory and olfactory. The patients were not oriented in place and time, could not find their place in the ward, did not recognize close people and relatives, and committed unmotivated actions. The intellectual-mnestic sphere was most affected.
Violation of higher mental functions more often manifested itself in the form of aphasia - in 47 (42%) patients, in the majority of whom (41 people) speech disorders were one of the leading symptoms of the disease. A combination of motor and sensory aphasia was more often observed. Among other lesions of cortical functions, a violation of praxis, various types of agnosia, alexia, dyscalculia, agraphia, etc. were noted.
31 (28%) patients had motor disorders in the form of central paralysis and paresis. In most patients they manifested as hemiparesis, with left-sided hemiparesis observed in 21 and right-sided hemiparesis in 8 people; 3 patients had tetraparesis, 1 had lower paraparesis. In 7 people, monoparesis of the peripheral type was detected. Muscle strength in most cases decreased to 2-4 points and tended to recover during treatment.
Damage to the cranial nerves was common - in 67 (60%) patients. The oculomotor and facial nerves were most often affected. 12 (11%) people had severe dysfunctions of the IX-X cranial nerves, manifested by phonation disturbances, difficulty swallowing, and absence of the pharyngeal reflex.
Other abnormalities of the nervous system included signs of supranuclear palsy and coordination disorders, and sensory disorders.
In 27 (24%) patients, severe meningeal syndrome was observed in the form of general hyperesthesia, photophobia, neck muscle tension, Kernig and Brudzinski symptoms. The nature of meningeal syndrome did not always correlate with the severity of inflammatory changes in the CSF, which were observed in 107 (95.5%) patients in the form of an increase in cellular composition (from 6 to 1613 cells per 1 μl) and protein (from 0.49 to 9.9 g/l). On average, the number of cells was 242±216 in 1 μl of CSF. In 5 (4.5%) patients, cytosis in the CSF was without abnormalities. In some observations, there was a delay in the sanitation of cerebrospinal fluid during examination in the long-term period. Thus, in 2 patients examined 10 and 14 months after the onset of the disease, inflammatory changes persisted in the CSF, which indicated chronicity of the infection.
As an illustration, we present 2 case histories of patients with GE: with a good treatment effect and with a fatal outcome of the disease.
Patient Yu.
, 23 years old, student. He became acutely ill on March 28, 1999: the temperature rose, headache, nausea, and vomiting appeared. The patient's condition did not improve, and on the 6th day of illness he was hospitalized.
Upon admission to the hospital on 04/03/99: conscious, oriented, moderate meningeal symptoms. In the CSF: 197 cells (83% lymphocytes), protein 0.264 g/l, glucose 2.8 mmol/l.
04/05/99 (8th day) the condition worsened: disorientation, amnesia of the acute period, agitation. Neurologically: anisoreflexia S>D, Babinski's sign on both sides. On the same day, generalized tonic-clonic convulsions with involuntary urination were noted. Blood pressure (BP) 180/100 mm Hg, pulse 160 beats/min. Acyclovir 1.5 g/day was prescribed intravenously.
In the following days, drowsiness, slight stupor, memory loss, positive meningeal syndrome. 04/8/99 (11th day) HSV-1 DNA was determined in the CSF using PCR.
A CT scan of the brain, performed on the 18th day of illness with the introduction of contrast (omnipaque), revealed in the right hemisphere in the projection of the temporal and occipital lobes, with partial extension to the subcortical formations and the parietal lobe, an extensive focus of heterogeneously reduced density, fragmentarily accumulating contrast. The median structures are shifted to the left, the third and lateral ventricles are compressed. Conclusion: changes of an inflammatory nature (Fig. 2, a).
Figure 2. CT scan of the brain of patient Yu., 23 years old. a - in the acute period of the disease on the 18th day of illness. Repeated CT scan (40th day) noted positive dynamics: the focus of low density decreased in size; the volumetric effect is practically not determined (Fig. 2, b).
Figure 2. CT scan of the brain of patient Yu., 23 years old. b — during the period of convalescence on the 40th day of illness.
A study of blood serum on the 6th day of illness for antibodies to HSV-1 was negative, on the 26th day it revealed positive IgM and IgG antibodies to HSV-1 in ELISA units. wholesale pl.
Among the somatic disorders in the acute period of the disease, the electrocardiogram (ECG) showed diffuse changes in the myocardium of both ventricles with impaired intraventricular conduction, which then gave way to signs of overload of the right side of the heart. Clinically, these changes were accompanied by tachycardia up to 90-100 beats/min. During treatment, myocardial changes reversed. Cardiac dysfunction was regarded as a phenomenon of myocarditis, which is observed in encephalitis [4]. During the course of the disease, the patient had an increase in liver enzymes (aspartate aminotransferase - 177 units, alanine aminotransferase - 89 units), which were reversible, indicating signs of reactive hepatitis.
Thus, based on the clinical manifestations of the disease, the results of laboratory tests (PCR, serological screening), characteristic changes on CT scan of the brain with the reverse dynamics of focal changes, herpetic (HSV-1) meningoencephalitis, myocarditis, and reactive hepatitis were diagnosed.
Subsequently, the patient is conscious, but disinhibited, euphoric, uncritical of his condition, and rational. When talking, he quickly becomes exhausted, asthenized, and the phenomena of echolalia occur. During the treatment, the patient's condition improved, the CSF was sanitized (day 39): 78 cells/μl (70 lymphocytes), protein - 0.66 g/l. The EEG in the acute period of the disease shows gross diffuse changes in the bioelectrical activity of the brain in the anterior central regions, epileptic activity (acute-slow wave complexes). Subsequently, the EEG picture will improve.
After treatment (acyclovir, dexamethasone, symptomatic therapy), the patient was discharged in satisfactory condition.
The combination of cerebral pathology with changes in other organs (heart, liver) is also pointed out by other researchers who believe that encephalitis is a particular complication of a general infection with damage to internal organs [7].
Patient T.
, 49 years old, builder, resident of the Moscow region. He became acutely ill on May 17, 1990: his temperature rose to 38 °C and he noted catarrhal symptoms. He was being treated for the flu. On the 4th day of illness, mental disorders appeared in the form of unmotivated behavior, aggressiveness, and hallucinations. At the same time, several generalized tonic-clonic seizures developed, meningeal signs and Babinski symptoms were detected. He was hospitalized in the district hospital, where delirium alcoholism was suspected due to an infectious disease. Periods of agitation were combined with episodes of hypersomnia. After 2-3 days, the level of consciousness decreased to stupor. On the 9th day of illness, a coma developed. When examining the CSF on the 10th day of illness: cytosis 3 cells/μl with normal protein content. CT scan of the brain (day 12) revealed a large area of low density on the convexital surface (Fig. 3a).
Figure 3. CT scan of the brain of patient T., 49 years old.
a — the first study on the 11th day of illness. On the 16th day of illness, GE was suspected, and treatment with acyclovir was recommended. On the 18th day, with a diagnosis of encephalitis, he was transferred to Infectious Diseases Hospital No. 1 in Moscow. CSF examination on day 18: cytosis 6 cells/μl with normal protein and glucose content. Treatment with acyclovir 15 mg per kg body weight per day intravenously was continued. Further, due to breathing problems, he was transferred to artificial pulmonary ventilation (ALV). Serological testing of blood and CSF for antibodies to HSV-1 using ELISA showed their significant increase (serum titers - 1:4096; CSF - 1:8). Repeated CT on the 24th day of head disease identified multiple foci of low density in both hemispheres (Fig. 3, b).
Figure 3. CT scan of the brain of patient T., 49 years old. b — study over time on the 24th day of illness.
The patient's condition remained the same: mechanical ventilation, deep coma with atony and areflexia. Progressive trophic disorders developed in the form of bedsores on the sacrum, limbs, and in the area of the shoulder blades. On the 42nd day of illness, death occurred.
An autopsy revealed multiple foci of necrosis in the parietal, temporal, frontal areas of the cortex and subcortical substance; an extensive focus of softening in the right frontal lobe. Throughout the brain, microscopic examination revealed glial nodules and perivascular inflammatory infiltrates. Pathological examination confirmed the diagnosis of herpetic encephalitis.
In conclusion, it should be noted that GE is a severe rare disease that causes significant damage to the nervous and mental sphere. It is accompanied by high mortality and severe psychoorganic disorders. Diagnosis of the disease is often difficult and requires modern clinical, virological, immunological, neuroimaging and laboratory studies. Despite the available active antiviral drugs, the problem of effective therapy for this disease is also not completely resolved.
The main factors causing viral encephalitis
The most common source that can begin to activate inflammation in the body is the herpes simplex virus. In addition to it, various other infections become the mechanism of manifestation:
Cytomegalovirus.- Chicken pox.
- Mononucleosis.
- Enteroagents.
- Adenoviruses and others.
The ways of spreading the disease are:
- Airborne method.
- Contact.
- Fecal-oral.
- Transmissible.
- Vaccination.
The development of this disease often occurs in newborns and people of retirement age. And also in patients suffering from HIV and other conditions that impair the functioning of the immune system.
Encephalitis caused by herpes simplex virus
Encephalitis, which is caused by the herpes simplex virus , is a very common clinical manifestation of a severe generalized herpes infection that affects the entire nervous system of the human body. Occurs sporadically. The severity of this disease is associated with the necrotic nature of the process and the subsequent formation of foci of hemorrhagic decay of the brain substance. In addition to herpetic encephalitis in newborns, in most other cases the causative agent of herpetic encephalitis is the herpes virus type 1. The main route of spread of infection is airborne, but household contact is also possible.
CLINICAL PICTURE
The disease begins acutely, with a rise in body temperature. Meningeal symptoms quickly appear, and general epileptic seizures often occur. Focal symptoms are manifested by central mono- and hemiparesis, hyperkinesis. In the cerebrospinal fluid, pleocytosis with a predominance of lymphocytes (up to several hundred cells in 1 μl), an increase in protein content (up to 2-3 g/l), mild xanthochromia or a small admixture of erythrocytes is detected.
SYMPTOMS
Early clinical manifestations of encephalitis are not specific. The onset of the disease resembles an influenza infection. The first symptoms are an increase in body temperature to high levels, severe headaches, decreased or complete loss of appetite, nausea, and possibly repeated vomiting. A state of prostration appears. Further, if the source of inflammation is localized in the temporal or frontal lobes of the brain, adults and older children may experience inappropriate behavior, psychosensory disturbances, skin hyperesthesia, delirium syndrome, taste and olfactory hallucinations. All of the above symptoms in young children are almost impossible to recognize. Subsequently, the course of the disease is in many ways similar to the clinical picture of acute encephalopathy, which is expressed in an increasing disturbance of consciousness from somnolence and stupor to cerebral coma.
One of the main manifestations of encephalitis is local convulsive twitching or attacks of generalized tonic or clonic-tonic seizures, which in younger children can develop at the very beginning of the disease, which can cause errors in diagnosis. Within a few days, depending on the focus of the inflammatory process, focal neurological symptoms in the form of hemiparesis, various sensitivity disorders, and aphasia begin to intensify. In addition, symptoms such as drooping of the corner of the mouth, smoothness of the nasolabial fold on one side, unilateral blepharoptosis, anisocoria, and deviation of the tongue may be observed. As a manifestation of increasing intracranial pressure, examination of the fundus reveals a congestive optic disc. In most cases, a sign confirming the herpetic nature of encephalitis is the appearance of a vesicular rash on the skin of the body around the end of the first week of the disease. If left untreated, the disease begins to progress steadily and in most cases has a poor prognosis.
A significant number of surviving patients develop severe persistent residual effects from the neuropsychic sphere in the form of intellectual impairment and the development of paralysis, paresis and contractures.
TREATMENT
Treatment should be carried out exclusively by a neurologist. Self-medication is unacceptable. Etiotropic therapy for herpetic encephalitis includes antiviral treatment with acyclovir (Zovirax, Virolex). This therapy should be based on the results of a clinical examination of the patient. Laboratory specific examination methods are time-consuming and cannot provide early diagnosis. Therefore, treatment with acyclovir should be started as early as possible, only if the herpetic nature of the disease is suspected, as well as with encephalitis of unknown etiology. To reduce body temperature, physical cooling methods are used - applying ice to the head and on the area of large vessels, wiping the surface of the body with alcohol or a 1-2% solution of vinegar or wrapping in a wet sheet, administering antipyretic drugs such as paracetamol, aspirin, cefekon and etc., introduction of lytic mixtures.
Symptoms
The first stage of the anomaly is distinguished by such complaints as:
Feverish condition.- Manifestation of malaise.
- Painful sensations in the muscles.
- Sore throat.
- Loose stools.
- Compression in the abdominal area.
The second stage involves the following problems:
- Pain in the head area.
- Nausea unrelated to eating.
- Gag reflexes.
- Particular sensitivity to bright light.
- Dizziness.
- Psychosensory disturbances.
- General lethargy.
- Epileptic seizures and more.
Simultaneously with these manifestations, focal neuralgic disorders progress. At the same time, the person begins to experience:
- Impaired sensitivity of the limbs.
- Difficulties in coordinating voluntary muscle activity.
- Problems with the speech apparatus.
- Sources of damage to FM neurons.
- Change in gait.
- Tremor.
The described symptoms can be diagnosed in various forms of the disease. But some manifestations of viral inflammation have a special type of severity, for example:
- Serious disturbances in consciousness.
- Hallucinations.
- Psychomotor seizures, etc.
Clinical analysis. Herpetic meningoencephalitis in patients over 20 years of age.
Authors: prof. Doctor of Medical Sciences Shmyrev V.I., prof. Doctor of Medical Sciences Devyatkin A.V., Ph.D. Kalenova I.E., Gavrilov D.Yu., Sharinova I.A., Litvinov N.I.
Introduction The causative agent of herpetic meningoencephalitis can be herpes simplex virus type 2 (HSV-2) and the varicella zoster virus. The mortality rate for this pathology is 15-20%, and without antiviral therapy 70%. Patients who survive often have persistent neurological deficits. The most common forms of herpetic lesions of the central nervous system are encephalitis, which can occur both against the background of other organ lesions (generalized cutaneous-visceral form) and in isolation. Herpetic encephalitis (HE) occurs with a frequency of 2-4 per 1 million population per year. Children account for about a third of all cases. PGs have dermatoneurotropism. This means that they primarily affect the skin, mucous membranes with stratified epithelium, eyes and the central nervous system. In the latter case, the most severe, life-threatening pathological processes develop in the form of encephalitis, meningoencephalitis, meningoencephalomyelitis, etc. GE can develop in connection with both the reactivation of a latent infection in the brain (according to modern concepts, in approximately 2/3 of patients), and with exogenous infection with a highly virulent strain of the virus (in 1/3 of patients). HSV can penetrate the central nervous system hematogenously or through nerve trunks (mainly through the branches of the trigeminal nerve and the olfactory tract). It has already been proven that they spread mainly through the neuronal route. From the Gasserian ganglion, the virus enters the subcortical nuclei, brainstem nuclei, thalamus and reaches the cerebral cortex. As the virus spreads along the olfactory tract, the hippocampus, temporal gyri, insula and cingulate gyrus (i.e. limbic system) are affected, and then in most cases the midbrain, brain stem and hemispheres are captured. In terms of clinical manifestations, HE is a classic example of encephalitis. It is characterized by four main syndromes: the syndrome of impaired consciousness, hyperthermic syndrome, convulsive syndrome and the syndrome of focal disorders. Herpetic encephalitis begins acutely (usually after 1-5 days of ARI clinic) with a sudden increase in temperature (usually more than 39°C), which is poorly reduced even while taking antipyretic drugs. Consciousness is disturbed: at first there may be short-term (for several hours) excitement, which is replaced by lethargy, drowsiness, and lethargy. Subsequently, the depression of consciousness progresses until it is completely lost. More often, against the background of high fever, impairment of consciousness manifests itself in the form of pronounced, deep, persistent depression (coma of varying degrees). Consciousness returns gradually, and after its stable recovery, signs of focal disturbance syndrome remain. In this case, the frontal lobes of the brain are often affected, which is clinically manifested by mnestic-intellectual disorders. The syndrome of focal disorders may also include dysfunction of any cranial nerves with the development of the corresponding clinic. Paresis of the hemiplegia type, asymmetry and loss of reflexes, and the appearance of pathological reflexes are possible. Another feature of GE is persistent convulsive syndrome. Convulsions are often generalized. A characteristic feature of GE is also hyperthermic syndrome, but sometimes so-called “cold” GE are encountered. Mortality in HE before the advent of acyclovir was 70-74%. Today, with timely initiation of adequate etiotropic therapy, it has decreased to 5-6%. However, as already noted, herpetic brain damage is a necrotic process, so after HE there is a high probability of neurological consequences. They can be either temporary or permanent. However, against the background of modern antiviral therapy, not only the mortality rate has decreased, but also the outcomes of GE in surviving patients have improved. Meningitis with herpetic lesions of the central nervous system usually develops against the background of encephalitis, i.e. proceeds as meningoencephalitis (MME). Moreover, inflammation of the membranes of the brain is serous in nature. Isolated damage to the meninges by HSV is rare. It is impossible to make a diagnosis of herpetic meningitis based on clinical signs alone. Special laboratory testing methods are required. However, with prolonged or recurrent serous meningitis, along with other studies, examinations for the presence of HSV are necessary. Description of a clinical case In a neurological department for patients with acute cerebrovascular accidents with intensive care wards, a 28-year-old woman was observed with a diagnosis of “Acute herpetic meningoencephalitis. Brain swelling. Right-sided hemiparesis. Exacerbation of chronic right-sided sinusitis. Diffuse bilateral endobronchitis. Endoscopic surgery on the right maxillary sinus dated April 17, 2010: submucosal vasotomy of the inferior turbinates. Tracheostomy dated April 28, 2010.” History of the disease. At the end of November - beginning of December 2009, the patient was observed as an outpatient with trigeminal neuralgia. At the end of March 2010, the patient traveled to Cuba. The patient noted a deterioration in her condition on April 5, 2010, when nasal congestion appeared. On April 12, 2010, I developed a severe headache. On 04/15/10, the headache intensified, dizziness, disorientation, nausea, vomiting, and hyperthermia appeared (body temperature 38.8 C). She was hospitalized at Clinical Hospital No. 1 in the ENT department with a diagnosis of acute purulent sinusitis. Course of the disease. A 28-year-old patient was admitted to the ENT department on April 17, 2010 due to right-sided sinusitis. CT scan of the paranasal sinuses dated 04/17/10: CT picture of right-sided sinusitis. Slight thickening of the mucosa in the left frontal sinus. Hypertrophy of the inferior turbinates. Deviation of the nasal septum. An emergency operation was performed: submucosal vasotomy of the inferior turbinates. Biopsy of the contents of the right maxillary sinus: areas of edematous and sharply inflamed polyposis-altered mucous membrane, bordered by respiratory epithelium with signs of hypersecretion, were sent. Microbiological examination of swabs from the throat and nose dated April 20, 2010 revealed: Acinetobacter spp. - abundant growth, sensitive to moxifloxacin, vancomycin. On the day of admission, general cerebral symptoms increased, disorientation appeared, the patient was consulted by a neurologist. Neurological status on admission: Stupefaction. Dysphoric, disoriented in place, time and personalities. personality. Rigidity of the nuchal muscles 3 points, Kernig's muscle on both sides, Pupils D=S, live photoreactions, nystagmus in the extreme leads. Tendon reflexes are lively and symmetrical. There are no pathological foot signs. PNP and PKP are performed with intention on both sides, more on the right. A cerebrospinal fluid analysis was taken and serous meningitis was diagnosed (in the cerebrospinal fluid: cytosis more than 800/3 with a predominance of lymphocytes more than 50%, with a slight increase in protein, Pandey’s test is negative). During microbiological examination of the cerebrospinal fluid, no microflora was isolated. In the UAC upon admission: Hb - 116 g/l, erythrocytes - 3.69 x 1012, platelets - 223, leukocytes - 12.4 x 109, p/i - 14%, s/i - 76%, eo - 1%, base - 0% , lymph-7%, mon-2%, ESR-36mm/h. No changes were detected in the biochemical blood test, coagulogram, and general urine test upon admission. CT scan of the brain upon admission: no pathological changes in the brain were detected. Since April 18, he has been in the intensive care unit due to serous meningitis. Detoxification and decongestant therapy was carried out, despite the treatment, the patient’s condition showed negative dynamics. Focal neurological symptoms appeared (right-sided deep hemiparesis, pathological foot signs), depression of consciousness to the point of coma, and several episodes of tonic-clonic seizures. On April 19, 2010, a repeat MRI of the brain was performed. (see Figure No. 1): In the basal parts of the temporal lobe there is an encephalitic focus measuring 57*39*50 mm. Perifocal edema is not expressed. The median structures are not changed. Conclusion: the pattern of identified changes in the left hemisphere in the temporal region most likely corresponds to inflammatory changes (encephalitis). Differentiate with ischemic changes. On April 19, 2010, a liquor analysis was taken for PCR diagnostics of pathogens of viral neuroinfections and microbiological research. A decrease in cytosis to 610/3 was noted. 04/20/10 Respiratory problems appeared, the patient was transferred to mechanical ventilation. On April 28, a tracheostomy was performed. In a study of cerebrospinal fluid dated April 19, DNA of virus types 1 and 2 was detected. Due to the herpetic etiology of the process, antiviral therapy was started. On 04/27/10, a CT scan of the brain was repeated: the CT picture of inflammatory changes (encephalitis) in both hemispheres is negative, with the presence of areas of cerebral edema in the lesions. The patient was consulted by an infectious disease specialist, a neurosurgeon, but the transfer was refused due to the lack of epidemiological danger to others and the severity of the patient’s condition. Against the background of the therapy, there is a positive dynamic: the level of wakefulness increases to the point of stunning, and he tries to carry out basic commands. In control studies of cerebrospinal fluid - a decrease in cytosis to 147/3 from 04/26/10, lymphocytes about 70%. Analysis of cerebrospinal fluid in the dynamics of Table 1. The level of respiratory support was gradually reduced, and on 05/03/10 the patient was transferred to spontaneous breathing. A consultation was held with the participation of infectious disease specialists, neurologists, and resuscitators to decide on the need to transfer the patient to an infectious diseases hospital. Conclusion: Acute meningoencephalitis caused by herpes simplex virus types 1 and 2 (HSV DNA in the cerebrospinal fluid) with foci of cerebromalacia of the brain. Considering the endogenous nature of the infection, there is no need for isolation. The patient is transferred to the neuroinfection department of the clinical infectious diseases hospital No. 1 in the city. Moscow. The patient was transferred to Clinical Hospital No. 1. In the neurological status at the time of transfer, consciousness is at the level of stunning, follows simple instructions, rapid exhaustion persists, right-sided hemiparesis is more pronounced in the leg, the impression of sensorimotor aphasia.
1 month after transfer to Clinical Hospital No. 1, she was re-hospitalized at Clinical Hospital No. 1 of the Administrative Department of the President of the Russian Federation. The patient was examined by neurologists, in neurological status: Conscious. Emotionally labile, disinhibited, criticism reduced. No speech disorders were identified. Moderately pronounced mnestic-intellectual decline (21 points on the MMSE scale). There are no meningeal signs. Parts of the cranial nerve: without pathology. There are no paresis, sensitivity disorders, or pathological foot signs. Treatment: 1. complex etiotropic therapy - Zovirax 1500 mg/day from April 20, 2010, for 12 days, ceftriaxone 4 g/day IV, from April 30 Zovirax IV drop 1000 mg/day, additionally cycloferon 250 mg IV Meronem 3-4 g/day, tavanic 500 mg/day IV. 2. Upon admission, a procedure for extracorporeal filtration of the cerebrospinal fluid was performed using a single-puncture “pendulum” method, against the background of which cerebral symptoms (headache, nausea, disorientation) decreased, a repeat analysis of the cerebrospinal fluid was taken, a significant decrease in the cellular composition of the cerebrospinal fluid was noted from 783/3 (neutrophils 198, lymphocytes 586), up to 202/3 (neutrophils 89, lymphocytes 113). The patient had no complications after the procedure. 3. Decongestant, neuroprotective, metabolic, anticonvulsant, and immunostimulating therapy were also carried out. Conclusion. A clinical case of herpetic meningoencephalitis during conservative therapy and a liquor filtration procedure with a favorable outcome is described. Bibliography. 1. Yushchuk N.D., Klimova E.A., Dekonenko E.P., Fedoseenko G.I. // Herpetic neuroinfections-2003. Moscow State Educational Institution VUNMC Ministry of Health of the Russian Federation.-p.4-32. 2. Lobzin Yu.V., Pilipenko V.V., Gromyko Yu.N. // Meningitis and encephalitis. - 2006 Folio. St. Petersburg. - p. 65-70 3. Protas I.I. // Herpetic encephalitis . -2000. Minsk: LLC "Met".-p.12-126 4. Sorokina M.N., Bezukhikh S.M. // Damage to the nervous system during herpetic infection - 1996. St. Petersburg: SPbNIIDI.-p.5-30 5. Ginzburg A.L., Romanova Yu.M. // Polymerase chain reaction for the diagnosis and control of treatment of infectious diseases. – 1998. – No. 2. – P. 35 39. 6. Nesterenko V.G., Bekhalo V.A., Lovenetsky A.N.// Clinic, treatment and laboratory diagnosis of human herpesvirus diseases: A guide for doctors/. – M., 1998. – 46 p. 7. Rakhmanova A.G., Prigozhin V.K., Neverov V.A. and others //Infectious diseases: A guide for general practitioners/. – M.–SPb, 1995. – 304 p. 8. Isakov V.A., Borisova V.V. Laboratory diagnosis of herpes virus infections // Unknown epidemic: herpes. – Smolensk, 1997. – P. 20-31. 9. Sorokina M.N., Bezukh S.M. // Lesions of the nervous system during herpetic infection. – St. Petersburg, 1996. – 35 p. 10. Weber B.// Biology of herpes virus infections and tagers of anti viral therapies Int. Meet. Skin Therapy Update.-1994- – EADV, EADV Board. – 1994. – P.46
Diagnostic options
Since such a disease lacks a specific clinical picture and is very similar to other central nervous system disorders, testing for this phenomenon becomes a rather difficult process. All stages are monitored by a specialist in the field of neurology. It is he who is obliged to compare anamnestic and epidemiological indications, features of symptoms and information obtained after additional examination techniques. The most common diagnostic procedures:
EEG.- Echo-encephalographic test to determine liquor hypertension.
- Ophthalmoscopic examination of optic nerve objects.
- Lumbar puncture.
- Cerebral fluid analysis is performed using a CT scan and an MRI scan.
- Serological techniques.
- PCR assessment.
Herpes simplex - symptoms and treatment
The incubation period for the acquired form lasts 2-14 days. Most often, it cannot be installed due to lack of manifestation.
Herpes simplex in children usually occurs as stomatitis and gingivitis - the temperature rises, fever, general intoxication, focal hyperemia (redness) of all mucous formations of the oral cavity, pain when chewing, increased salivation. Small children refuse to eat due to pain. In a short period of time, small vesicular rashes appear at the site of hyperemia, which quickly open, leaving behind painful erosions - aphthae. Regional lymph nodes enlarge and become painful. Over time, the immune system strengthens and the symptoms gradually regress without any traces of damage. Relapses are rare.
When the skin is affected (mainly in adults), vesicular rashes often appear around the mouth, wings of the nose, and sometimes on the torso and buttocks. The rash consists of small vesicles with serous contents on a slightly hyperemic skin background. Subsequently, they open and dry out, after which crusts form without a trace.
Sometimes the bubbles merge into quite large bubbles. Often their contents fester, oozing forms, and a secondary streptococcal or staphylococcal infection (staphylo- and streptoderma) occurs.
General health, as a rule, does not change. Sometimes the regional lymph node may be slightly enlarged and painful. In general, the process rarely lasts more than a week.
With severe immunodeficiencies, the infection may take a more widespread (generalized) course. In this case, a syndrome of general infectious intoxication occurs and internal organs are affected: the liver and spleen are enlarged, the nervous system is affected (meningoencephalitis, encephalitis and meningitis), as well as the lungs, kidneys and other organs. With relapses of a chronic infection, patients sometimes feel mild discomfort and tingling in the area of future rashes.
With genital herpes, rashes appear on the skin and mucous membranes in the genital area and perineum. They are usually accompanied by soreness, hyperemia of the surrounding tissue, enlargement and tenderness of the inguinal lymph nodes. The frequency of relapse depends on the individual characteristics of the immune system.
With ophthalmoherpes - eye herpes - unilateral lesions are more often observed due to the transition of the primary process to the organ of vision, i.e., a secondary lesion occurs. Keratitis, blepharoconjunctivitis, iridocyclitis, uveitis, chorioretinitis, optic neuritis and other manifestations may be observed.
A very unusual form of manifestation of herpes simplex is known as Kaposi's eczema herpetiformis - eczema herpeticum. As a rule, it occurs in people who have any skin disease or predisposition to it (dermatosis or “problem skin”). In this case, intoxication and high body temperature are observed, herpetic blisters appear everywhere, quite abundant and closely spaced, periodically merging, sometimes with hemorrhagic impregnation. In some cases, they suppurate, then they open, dry out and form a solid crust. When the rash is completely treated with green paint, the patient’s skin takes on the appearance of crocodile skin. The disease is often quite severe and can lead to death.
During pregnancy, the child becomes infected:
- before birth - in 5% of cases (primary infection and ascending infection during this period are rare);
- during childbirth, i.e. when passing through the natural birth canal - in 95% of cases.
With primary infection of a pregnant woman in the first trimester or with ascending infection of the fetus, malformations often develop that are incompatible with life, or a miscarriage occurs, especially when infected with type II herpes virus, which is the infecting agent most often - up to 80% of cases.
When a pregnant woman is infected in the second and third trimesters, the risk of injury to the child is about 50%. At the same time, the liver and spleen enlarge, specific inflammation of the lungs, jaundice, metabolic disorders, malnutrition, meningoencephalitis, anemia and more occur. After birth, it can occur either in an asymptomatic subclinical form or have severe disabling consequences - blindness, severe damage to the central nervous system, deafness [1][2][6][8][11].
How to get rid of viral encephalitis
After all clinical testing is completed, the treating doctor draws up a special treatment plan, which includes complex therapy. It consists of numerous techniques. Let's look at them in more detail:
- Etiotropic step - the use of drugs with antiviral effects is prescribed, as well as interferon and its like, special forms of immunoglobulin. The main task of such therapy is to correct vital options, the use of anti-edema drugs, antihypoxic and neuroprotective medications.
- Symptomatic step - aimed at taking anticonvulsants, antiemetic components, antipsychotics, tranquilizers and other psychotropic substances.
- The restorative step is carried out by a neuroprotective and vascular treatment method, various massages and exercise therapy are used, as well as physiotherapeutic techniques.
In case of mental problems, several sessions with a psychiatrist will be required. Thanks to the consultation, the patient will participate in correctional therapy, learn social adaptation and go through all stages of psychotherapy.
Next move
An inflammatory process of an encephalitic nature can cause a huge number of serious consequences, in particular the formation of swelling of the brain and the formation of a dislocation disorder, which provokes compression of the main organ in the area of the column. This process can be the main factor in death. If a coma develops, the person switches to a vegetative mode. The death of the patient in some cases is associated with the connection of microorganisms of an intercurrent nature, the progression of cardiac failure and respiratory failure.
With viral encephalitis, the patient begins to experience epilepsy, persistent neurological deficits, hearing loss, mental disorders, etc. According to the information received, the further prognosis for people with a similar disease depends on the form, severity of development and general condition at the beginning of treatment. Based on information from interviews with many medical workers, almost 30% of patients with the tick-borne form of the disease end up fatal. The Japanese stage is distinguished by a large number of deaths and a high percentage of residual consequences in those who have recovered from the disease. The post-vaccination form often has a favorable prognosis. The only exception is a disease that spreads after an anti-rabies injection like Landry's ascending paralysis and provokes the risk of death as a result of bulbar deformities.
In order to prevent damage to the body by such a disease, it is necessary to adhere to the following medical recommendations:
- Apply protective measures against insects that are active carriers of inflammation.
- Timely seeking qualified help from specialists if an infection occurs.
- Monitor your immunity level.
- Carefully choose doctors for vaccinations.
- Observe the dosage and administration of the drug.
Acute encephalitis. Herpetic encephalitis
1) Herpetic encephalitis (HE), acute necrotizing encephalitis.
It is the most common (20% of all viral encephalitis) and most severe form of sporadic acute encephalitis.
Prevalence - from 0.3 to 1.8 per 100,000 population per year (according to other sources - 2-4 per 1,000,000). The causative agent is most often the DNA genomic herpes simplex virus type 1 (HSV-1), which also causes herpetic lesions of the oral mucosa and various diseases of the central nervous system. Less commonly, DNA genomic herpes virus 2 (HSV-2), which causes rashes in the genital area and is sexually transmitted; It is this that causes encephalitis in some newborns; they become infected from a sick mother after rupture of the membranes or during childbirth. Herpes viruses multiply in the nucleus of neurons of the sympathetic and sensory ganglia, then pass into a latent state and remain there during life, periodically leading to relapses of herpes infection in persons with temporary or persistent immunodeficiency of various origins (poor nutrition, drugs, alcohol, AIDS, heredity, etc. ). In the postnatal period, infection can occur through contact with persons who have an exacerbation of cutaneous herpes.
In the first 10 years, the most widespread infection of children with herpes viruses occurs (70–80% of cases). The development of encephalitis is possible during primary infection with HSV (30%) or due to activation of a persistent AI virus (70%). The virus enters the brain through the hematogenous route and through the perineural tract of the cranial nerves.
When the disease occurs in the brain, severe swelling, single or multiple foci of hemorrhage, softening, perivascular lymphocytic infiltration and liquefaction necrosis occur, mainly in the cortex of the temporal and frontal lobes of the brain and the underlying white matter. Edema can lead to dislocation and herniation of brain structures, in particular, infringement of the hippocampal gyrus or brain stem, which is a frequent cause of death. In subacute and chronic GE, along with fresh areas of necrosis with perifocal and perivascular infiltration, cystic cavities and foci of gliosis are found.
The incubation period of GE lasts from 2 to 26 days, more often – 9–14 days. Symptoms of HE in newborns appear at 2–4 weeks of life, and with generalized herpetic infection - in the first 10 days after birth. When the infection generalizes, both the brain and other organs are affected, and jaundice, collapse, and shock are possible. GE often develops against the background of acute respiratory viral infections, influenza, aphthous stomatitis, laryngotracheitis, and gastrointestinal diseases. In children, especially in newborns, typical herpetic rashes are observed on the skin and mucous membranes (in adults - in 10–15% of cases). There are 4 stages of GE: early, culminating, reverse development and residual phenomena.
The disease begins acutely, less often - subacutely, with a rise in body temperature to 39–40°C (sometimes low-grade fever), headache, general weakness, vomiting. The febrile period lasts up to several weeks, sometimes it is fleeting or even absent. Sometimes there are two febrile waves separated by a “clear” interval, with focal neurological symptoms occurring during the second wave. Neurological and psychiatric symptoms may develop acutely or gradually.
Its nature depends on the predominant localization of the lesion in the temporal or frontal lobe. Violations of higher brain functions (motor, sensory, amnestic and other forms of aphasia), amnesia, agnosia, apraxia, behavioral disorders, pathology of smell and taste (anosmia, olfactory and gustatory hallucinations), confusion, depression of consciousness (up to coma) are observed. hemiparesis, hemianopsia, cranial nerve lesions, autonomic disorders, complex partial epileptic seizures. Generalized epileptic seizures often occur at an early stage, and status epilepticus (with seizures of various types) may develop. In most cases, meningeal symptoms are detected, sometimes congestive optic discs and herpetic rashes on the lips are found. It should be noted: herpes labialis can occur in any febrile state, not only with GE.
Without treatment, the condition steadily worsens, coma develops, and death occurs in 50–70% of cases. Death can occur in the first 24–72 hours of illness due to swelling and herniation of the brain due to respiratory arrest, cardiac activity, and destruction of other vital centers of the brainstem. For example, in the USA, 5,000 cases of HE are registered annually, with 1/3 of patients dying, and 1/3 of patients developing persistent neuropsychiatric disorders.
In recent years, atypical forms of HE have been described with erased subacutely developing symptoms, with predominant damage to the brain stem (brainstem encephalitis, as well as forms that mimic acute psychiatric pathology, in particular delirious stupefaction). A recurrent form of HE with exacerbations 2–10 years after the next remission is rare. In middle-aged and elderly people, a chronic form of GE occurs with a gradual increase in neuropsychic disorders and mnestic-intellectual decline.
The stage of residual phenomena is formed within 1–2 years or more after the end of the manifest stage of HE.
Diagnosis. When examining the cerebrospinal fluid, increased pressure, lymphocytic or lymphocytic-neutrophilic pleocytosis (on average 50–100, sometimes up to 1000 cells in 1 μl), a moderate increase in protein concentration, normal glucose levels are revealed (in 25% of cases the glucose level is reduced, this creates certain difficulties in differential diagnosis with tuberculous or fungal meningitis). In more than 40% of patients, red blood cells and xanthochromia are found in the cerebrospinal fluid - an indication of the hemorrhagic nature of the lesion. In 5–10% of cases, during the first examination of the cerebrospinal fluid, no changes are detected in it.
On the EEG, against a background of diffuse slowing of electrical activity, focal changes in the anterior parts of the brain (frontotemporal region) are recorded in 85% of patients in the form of slow-wave activity or periodic high-amplitude epileptiform discharges. At the beginning of the disease, they can be in one hemisphere, but later they are detected on both sides.
CT scan may not detect changes in the first 3–5 days. Later, most patients develop foci of low density with mass effect, primarily in the frontotemporal region, cingulate gyrus, and insular zone on one or both sides. Sometimes hyperdense (superdense) areas of hemorrhages are found. Lesions may accumulate peripheral contrast, reflecting disruption of the blood-brain barrier.
MRI allows you to identify focal hyperintense zones in T2 mode at a time when they are not yet visible on CT; in the first two days they may not be visible even on MRI (but with a brain abscess, tumor, subdural empyema, they are detected very early).
Due to the widespread prevalence of herpes infection, the detection of specific antibodies is not of great importance (even with a high titer). The results of the study of paired sera become too late (on the 10th–12th day). The fastest and most reliable method for identifying HE is now the polymerase chain reaction. It becomes positive already on the 1st day after the onset of neurological symptoms. The probability of error during PCR does not exceed 5%.
Therapy. Usually performed in an intensive care unit. The drug of choice is acyclovir (Virolex, Zovirax), which selectively inhibits viral DNA synthesis. The main condition for the success of treatment is its early start (at least before the development of stupor or coma). Treatment with acyclovir is recommended to begin at the slightest suspicion of the herpetic nature of encephalitis, i.e. in almost every case of severe encephalitis. Only after eliminating the possibility of GE, treatment with acyclovir is stopped and another one is prescribed, corresponding to the etiology of the disease. Acyclovir is administered intravenously in a single dose of 10 mg/kg 3 times a day, slowly over at least 1 hour (to prevent precipitation of the drug in the renal tubules). The course of treatment is at least 10–14 days.
Pathogenetic and symptomatic therapy is also important, aimed at maintaining respiratory and cardiovascular functions, water and electrolyte balance, prevention and treatment of secondary bacterial and trophic complications (aspiration pneumonia, bedsores, urinary infection), deep vein thrombosis of the leg. To reduce ICH, osmodiuretics, mechanical ventilation in hyperventilation mode, and in especially severe cases, barbiturates are prescribed. Corticoids do not significantly reduce ICP in GE, and their administration is believed to be of little value. In the presence of seizures, as well as for their prevention (when paroxysmal island-wave activity appears on the EEG), anticonvulsants are prescribed.
The early start of rehabilitation measures is very important.
Forecast. The use of acyclovir reduces mortality to 28%, and among surviving patients increases from 5 to 28% the proportion of those who recover completely or with minor residual neuropsychic disorders. Approximately half of the patients develop a persistent residual defect in the form of amnesia, aphasia, dementia, personality changes, epilepsy, and other mental and neurological disorders.
Return to Contents