What is intercostal neuralgia?
Neuralgia of the intercostal nerves is pain of a different nature that occurs due to various etiological factors. It is more often observed in adult men and women over 30-35 years of age. Symptoms of neuralgia may appear suddenly on one or both sides of the chest, along one or more intercostal nerves. The disease has an ICD code - M.79.2.
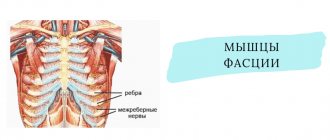
To understand what intercostal neuralgia is, you should understand the anatomical features of the thoracic nerves. There are 12 pairs in total. Each intercostal nerve contains motor, sensory and sympathetic fibers. It originates from the anterior roots of the spinal cord of the thoracic spine, passes along the lower edge of each rib, reaching the sternum. The parietal pleura covers the nerve fibers on top.
Thoracic nerves transmit impulses to the skin, the musculo-ligamentous apparatus of the chest and the anterior wall of the abdomen, partly the pleura and peritoneum, and the mammary glands. Sensitive fibers of neighboring nerve trunks actively interact with each other, creating cross innervation.
How are intercostal nerves arranged? What functions do they perform?
Two nerve roots emerge from the spinal cord: the anterior one is formed by the processes of motor nerve cells, the posterior one - by sensory ones. Then, while still inside the spinal canal of the spine, these roots are connected to form the spinal ganglion. Two spinal nerves depart from it: anterior and posterior.
In the thoracic spinal cord, the anterior branches of the spinal nerves pass into the intercostal nerves. They pass in the spaces between the ribs - each of them is located along the lower edge of the corresponding rib - and, unlike the anterior spinal roots, are mixed, that is, they are responsible for both movement and sensitivity:
- provide movement of the chest muscles involved in the breathing process;
- provide sensitivity to the skin of the chest and upper abdomen.
How to distinguish intercostal neuralgia from heart disease?
If neuralgia has acute symptoms in the thoracic region on the left side, differential diagnosis with heart disease must be carried out. You should not look for the cause of the pain syndrome on your own. Thoracalgia on the left side should always be a reason to consult a doctor.
Heart pain and symptoms of intercostal neuralgia on the left have distinctive features:
| Intercostal acute neuralgia on the left: typical symptoms | Cardiovascular diseases: characteristic manifestations |
| The pain intensifies with forced breathing, coughing, sneezing, laughing, physical exertion and movement, but does not change with fast walking and excitement. | The pain does not change its intensity with a deep breath or muscle tension, but intensifies with cardio exercise (fast walking, running, climbing stairs). |
| Chest neuralgia is not relieved by taking nitroglycerin | With angina pectoris, the pain attack goes away within 3-5 minutes after using nitroglycerin. With myocardial infarction, severe pain cannot be relieved with medications. In this case, you should immediately call an ambulance. |
| Normal pulse and blood pressure are determined | Changes in heart rate and blood pressure |
| Pain increases with palpation of the ribs and spaces between them | The intensity of pain does not change when palpating the intercostal spaces |
| Painful symptoms on the left “go” along the nerve or are encircling in nature | Pain is localized behind the sternum or in the projection of the heart |
Symptoms of intercostal neuralgia on the left and right should also be differentiated from other diseases (pleurisy, pneumonia, thoracic aortic aneurysm, pericarditis, acute pancreatitis and others). If there is severe pain in the chest, only a doctor can determine exactly what it is - neuralgia or another pathology.
Necessary examinations
When I encounter such phenomena, I immediately refer the patient for an ECG. This is especially true for people over 45 years of age, even if the signs are not typical for myocardial ischemia. It is better to make sure that the person is not in danger, and only then calmly carry out treatment for neurological or other abnormalities. If you have angina, you should do an ECG with stress, since it may not show any changes when pain is eliminated.
In some cases, it is necessary to use other instrumental methods:
- Coronary angiography. It is carried out using contrast injection and helps determine the presence of narrowing in the vessels of the heart.
- EchoCG. Ultrasound is used for this. It allows you to see the structure of the chambers of the heart muscle, the condition of the valves, the thickness of the walls, and the presence of inflammatory processes.
- Tomography of the spinal column (or MRI). Performed after ruling out cardiac pathology. During the manipulation, the size of the intervertebral spaces and the condition of the bone tissue, the presence of disc protrusions and pinched neurovascular roots are assessed.
The laboratory evaluates biochemical markers (ALT and AST), their increase indicates the development of a heart attack or myocarditis. More modern ways to determine acute necrosis are to increase the concentration of troponins in the blood.
Causes of intercostal neuralgia and risk factors
Intercostal neuralgia can develop for a variety of reasons. Among them are:
- injuries to the thoracic nerves, chest and spine;
- surgical interventions, long-term immobilization of a person in a certain position;
- poisoning with chemicals, prolonged use of medications;
- congenital developmental anomalies, hereditary diseases;
- infectious processes (shingles, tuberculosis, brucellosis and others);
- some neurological diseases, such as radiculitis and multiple sclerosis;
- diseases of the spine (osteochondrosis, deforming spondylosis, herniated intervertebral discs);
- compression of nerve branches in the bone-connective sheaths, for example, in the presence of scar changes, benign or malignant neoplasms;
- immunodeficiency (HIV infection, cancer, etc.);
- allergic reactions;
- diabetes;
- various metabolic disorders in nervous tissue and its hypoxia;
- lack of B vitamins in the body;
- alcohol abuse;
- osteoporosis;
- pathology of nearby anatomical structures (aorta, lungs, pleura);
- various systemic diseases (atherosclerosis, rheumatism, anemia, thyrotoxicosis, etc.).
More often, chest neuralgia appears due to several causes. Therefore, it is typical for older patients with vascular, degenerative and metabolic disorders. Sometimes symptoms of neuralgia appear after excessive physical activity, sudden movements or prolonged stay in one position. They can also occur after hypothermia or severe stress.
More often, intercostal neuralgia is observed on the left or right; less often, there is a bilateral lesion. In most cases, the pathogenesis is based on muscle spasm, leading to compression of nerve fibers. Pain occurs in response to nerve damage.
In children, signs of intercostal neuralgia are rare. When they appear, parents should definitely show the child to the doctor, as this may be a signal of the presence of a serious pathology. The doctor will determine the possible causes and explain how to cure intercostal neuralgia in this case.
Forms of the disease
Chest neuralgia can be primary (an independent pathology) and secondary (a symptom of another disease). There are also radicular and reflex forms of the disease. In the first case, symptoms of intercostal neuralgia on the left and right arise due to irritation of the spinal roots. The second type of pathology occurs due to a negative effect on peripheral receptors.
In addition, clinicians distinguish the following types of thoracic neuralgia:
- musculoskeletal;
- vertebrogenic;
- spicy;
- chronic;
- right-sided;
- left-handed;
- psychogenic;
- during pregnancy.
Intercostal neuralgia of a certain type has its own characteristic symptoms and treatment features.
Prevention
The following recommendations help to avoid the appearance of intercostal neuralgia:
- Moderate physical activity to strengthen the muscle frame and maintain their elasticity.
- Maintaining correct posture.
- Healthy eating.
- Daily routine and alternation of work and rest time.
- Protection against hypothermia.
You should not endure the pain of intercostal neuralgia and worry about its causes - consult a doctor to be sure that there are no serious pathologies and for quick relief of symptoms.
Symptoms of neuralgia on the right and left
Any neuralgia, including intercostal neuralgia, is primarily pain. Painful sensations can be of a different nature (aching, dull, sharp, piercing, burning) and have different intensity. Sometimes the pain is so severe that it forces a person to take a forced position and sharply limit physical activity. Intercostal neuralgia, which has pronounced symptoms, is described by patients as a lumbago or electric current discharge running from the spine to the sternum.
Thoracalgia often begins gradually, with a tingling sensation in the intercostal spaces, then acquires pronounced intensity. Less often it occurs suddenly. The pain can radiate to the scapula, epigastric area, heart, arm and lower back. Sometimes it takes on an encircling character. It intensifies with changes in body position, movements, coughing and deep breathing.
As a rule, painful attacks are constantly repeated, lasting from a few seconds to 2-3 minutes. Therefore, treatment of acute intercostal neuralgia on the right and left, first of all, always begins with the elimination of pain.
In addition to thoracalgia, a person may be bothered by characteristic local signs caused by the influence of sympathetic, sensory and motor nerve fibers. Intercostal neuralgia, depending on the damage to a particular nerve, will have characteristic symptoms on the right, left or both sides of the chest:
- impaired sensitivity, crawling sensation, numbness, tingling;
- muscle twitching;
- increased sweating;
- change in skin color.
If chest neuralgia appears against the background of a herpes infection, it may be accompanied by skin rashes. The latter appear 2-4 days after the onset of thoracalgia. Elements of the rash are located on the skin of the intercostal space in the form of small pink spots, which then turn into vesicles and then into crusts. Subsequently, traces of pigmentation may remain on the skin.
Heart diseases with similar symptoms
I want to say that there are many cardiac and vascular pathologies that are accompanied by similar symptoms. I propose to consider the most common abnormalities, this will help to understand whether the heart or neuralgia is the cause of the pain.
Angina pectoris
Pain in this case occurs in the area of the heart muscle (but do not forget that there are atypical attacks). It has a diffuse nature, a person is not able to indicate the exact location. Its strength and description are variable: it can be pressing, piercing, cutting, baking. It radiates to the left arm, under the shoulder blade, neck, lower jaw. It does not depend on the position of the body, but can be provoked by physical overload, nervous stress, as well as sudden hypothermia or overheating.
At this moment, there is a fear of death, shortness of breath with difficulty in inhaling. The attack can be one-time, occurring 1-2 times a day or more often. Its duration ranges from 3-5 to 20 minutes. Almost the same signs are characteristic of myocardial infarction. But unlike angina, the attack usually lasts a long time. The patient takes a certain position in bed - sitting with his legs down or lying on several pillows. You can read more about angina pectoris and how to deal with it in the article at the link.
Myocarditis
Inflammatory diseases are accompanied by moderate pain, which is monotonous. Occurs in 90% of all patients. They describe it as aching or pressing. In the acute period, signs of inflammation are observed (fever, body aches), shortness of breath with impaired inhalation or exhalation. The history often reveals a recent infectious disease. There is no clear dependence on physical activity.
Often myocarditis simulates angina pectoris, especially in older people, when pain and lack of air come to the fore, and the rest of the symptoms are smoothed out or do not appear.
Perikadite
The pain of pericarditis gradually increases, but when effusion appears, it can significantly decrease or go away completely. It stings, cuts, radiates to the neck, back, shoulder, to the right side, and lasts for a long time. Some relief occurs in a sitting position with anterior tilt.
In acute dry inflammation, an attempt to make a deep entrance increases the pain, so with this disease a person breathes quickly and shallowly. During auscultation, in this case, I clearly heard the pleural friction noise. The heart most often hurts with this type of pericarditis in the apex area.
A complete collection of information about pericarditis and its treatment methods is here.
Aortic aneurysm
The symptoms of this acute condition are largely reminiscent of myocardial infarction. A sharp increase in blood pressure, stress or physical activity can be a provocation. The pain is tearing, bursting, localized in the retrosternal region, radiating to the neck, lower jaw, right side of the chest, and sometimes runs along the spine. Has a wavy character. In some cases, it spreads to the projection area of the abdominal aorta and even to the legs.
At the same time, sharp pressure surges appear; when the pressure drops, a collapsible state may occur. There is an asymmetry of the pulse on the left and right arms. As blood begins to accumulate under the inner lining of the aorta, symptoms of anemia (pallor and blueness of the skin, dizziness) quickly develop.
Pulmonary embolism
Pulmonary embolism is accompanied by sharp and severe pain, which is localized in the center of the sternum, as well as to the left or right of it. It can last from a few minutes to 3-5 hours and is associated with respiratory movements of the chest. At the same time, a lack of air comes to the fore, a sharp decrease in pressure, up to collapse. Clinical manifestations depend on the location of the thrombus and its size. When the lumen of a large vessel is blocked, cyanosis appears in the upper part of the body, arrhythmia with an increase in pulsation frequency. When small arteries are blocked, the skin develops blue, shortness of breath, the pain is most often moderate, cough and sputum streaked with blood are observed.
Diagnosis of intercostal neuralgia
Make an appointment Shpigel Anna Yakovlevna Neurologist, massage therapist 33 years of experience. The specialist receives: - newborn children and schoolchildren - adults - athletes Reviews from patients Consultation from 3000 rubles.
Acute intercostal neuralgia is a reason to contact a competent, qualified neurologist. Since symptoms in adults with damage to the thoracic nerves can be disguised as other diseases, the patient must undergo a comprehensive examination to exclude possible pathology. The doctor must conduct a survey and examination.
The person’s posture is noteworthy when he leans towards the healthy side, so as not to provoke a painful attack. Palpation of the chest reveals pain. Trigger points are identified at the lower edge of the rib, where the affected nerve passes. If neuralgia affects several nerve branches, which often happens, this leads to a decrease or complete loss of sensitivity in the corresponding area of the body.
First of all, the doctor must distinguish the symptoms of intercostal neuralgia on the left from cardiovascular pathology. For this purpose, the patient undergoes an ECG. If indicated, a cardiologist is consulted. In order to correctly diagnose and treat intercostal neuralgia, the doctor also excludes diseases of the respiratory system, digestive tract, musculoskeletal system, infectious processes and other diseases. He may prescribe a number of additional tests (laboratory tests, x-ray of the lungs, ultrasound of the abdominal organs, MRI of the spine, etc.).
Thoracic neuralgia is an indication for electroneurography. This method allows you to determine the condition of nerve fibers by assessing their structure and functionality.
Chest neuralgia can be a manifestation of benign and malignant tumors. It is often the first symptom of a herniated disc and degenerative changes in the spine. Therefore, early identification of its causes is considered an important task for the neurologist and the patient.
What other diseases lead to girdle pain in the chest?
Often people tend to dub “neuralgia” any girdle pain along the ribs. But this symptom may have other causes, including:
- Spondylosis is an inflammatory disease that causes damage to the vertebral bodies and deformation of the spinal column.
- Hormonal spondylopathy is a pathology that develops in older people, for example, in women after menopause. The spine is deformed, and disorders occur in the vessels that supply it.
- Malignant tumors - those that arise in the spine itself or metastases from other parts of the body.
- Ankylosing spondylitis is a chronic inflammatory process that leads to decreased mobility in the spinal column.
- Gastritis and other diseases of internal organs.
How does the treatment of intercostal neuralgia depend on the cause?
With intercostal neuralgia, it is not enough to eliminate the main symptom of the disease - pain. You should always look for and treat the underlying cause. The doctor prescribes therapy individually, depending on the pathological changes detected during examination and examination, and the final diagnosis.
Make an appointment at the Medica24 International Clinic - get a consultation with an experienced neurologist and undergo an examination using our modern equipment. This will help to quickly and accurately establish a diagnosis and prescribe the correct treatment in a timely manner.
Get a consultation with a doctor
Message sent!
expect a call, we will contact you shortly
The main manifestation of intercostal neuralgia – chest pain – can also occur with many other diseases. And figuring out the correct diagnosis is not always easy.
The diagnostic process begins with a visit to a neurologist. The doctor will ask you some questions:
- When did you first experience pain? How did this happen? What preceded this?
- What is the nature of the pain, when does it usually occur, how often, how long does it last?
- Do you have chronic lung or heart diseases? Are you monitoring your blood pressure?
- What infections have you had? Have you had any chest injuries or surgery?
- What other symptoms bother you?
You may be asked to complete a special “pain questionnaire”. The doctor will perform a complete neurological examination to rule out other neurological diseases. You will then be given an examination.
To understand the causes of irritation or compression of the intercostal nerve, the doctor may prescribe x-rays, CT, MRI, and, if necessary, other studies.
How to treat intercostal neuralgia?
Treatment of any neuralgia, including intercostal neuralgia, is aimed at eliminating the clinical manifestations and causes of the disease. Therapy includes a whole range of activities. If a patient is diagnosed with neuralgia, you can find out how to treat it from the specialists of our clinic. The doctor will select the optimal therapeutic course, taking into account the characteristics of the disease and the individual characteristics of the person.
As a rule, intercostal neuralgia requires long-term treatment and further measures to prevent painful attacks. The doctor prescribes specific methods of therapy, determines the duration of each course, and gives his recommendations on lifestyle and regimen. The treatment plan may include:
- painkillers;
- etiotropic therapy aimed at combating the underlying disease;
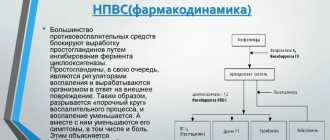
- anti-inflammatory drugs;
- neurotropic drugs;
- physiotherapy;
- osteopathy;
- massage;
- Exercise therapy.
The doctor always chooses how to treat neuralgia, based on the clinical picture, the stage of the process, the results of diagnostic examinations and the individual characteristics of the patient.
Treatment
The goals of therapy for intercostal neuralgia: reduce pain, eliminate the cause of pinching or inflammation.
For this purpose, drug treatment is prescribed using:
- Muscle relaxants to relieve muscle spasms.
- Neuroprotectors for the protection and restoration of nerve cells.
- Painkillers and injection therapeutic blockade with various drugs. It has a strong analgesic effect, relieves swelling and eliminates muscle spasms.
Drug treatment of intercostal neuralgia is complemented by physiotherapy. The following physiotherapeutic procedures can be used:
- Exercise therapy is an individually selected set of exercises to relax spastic muscles, improve blood circulation and lymph flow in the problem area. Exercise therapy is effective for the treatment and prevention of neuralgia, but it can only be done if there are no contraindications. It is important not to cause harm, which is possible with home exercises. What exercises will be effective, how exactly to do them, the number of repetitions - all this will be advised by a physical therapy doctor. The safest and most effective classes are under the supervision of a physical therapy instructor in individual or group classes.
- Laser therapy uses light energy to increase blood circulation, relax muscles, and reduce pain and inflammation.
- Magnetotherapy - the effect of an electromagnetic field on the body leads to the elimination of congestion, improvement of blood circulation, and reduction of pain syndromes.
- Diadynamic therapy, galvanization, exposure to interference currents and other procedures with electric current of varying power and frequency. They have a healing effect on soft tissues, improving blood circulation and lymph outflow, relaxing muscles and providing an analgesic effect.
- Electrophoresis is a procedure that improves the penetration of drugs into soft tissues and accelerates their action.
- Therapeutic massage and manual therapy are methods of influencing the body with the hands of a doctor. They allow not only to reduce or completely relieve pain, but also to treat the causes of intercostal neuralgia - pathologies of the spine, functional blocks in its work. What exactly to use - acupressure, segmental or other types of massage - is decided by a chiropractor or massage therapist.
- Acupuncture (acupuncture) – injections with thin needles into biologically active points on the body to relieve pain and normalize the functioning of internal organs.
Treatment of intercostal neuralgia on the right or left side of the chest, in the side with the help of physiotherapeutic procedures is carried out in several procedures. A full course usually consists of 10-15 sessions. Appointments are always individual.
Is osteopathy effective for intercostal neuralgia?
The causes of neuralgia in the rib area can be different. However, in many cases, a pinched nerve is caused by the consequences of various injuries a person has received in the past. The capabilities of fine diagnostics using hands make it possible to identify and eliminate these disorders, which leads to the elimination of compression of the nerve and the restoration of its normal blood supply. As a result, inflammation and its integral companion – pain – go away. Osteopathy shows high effectiveness in the treatment of both unilateral and bilateral intercostal neuralgia.
How to eliminate pain
Providing assistance depends on the cause of the pain, it is carried out as follows:
- "Nitroglycerin" and "Aspirin" during angina pectoris.
- "Analgin" or "Ibuprofen" for pinched roots. Simultaneous use of ointments and gels “Deep-relief”, “Menovazin”.
- In case of a heart attack, aneurysm or embolism, the attack is stopped in intensive care with the use of narcotic analgesics.
If pain radiates to the abdominal area, you should not self-prescribe treatment until a doctor arrives. This will help eliminate acute conditions of the abdominal organs.
Possible complications and consequences
Any neuralgia, in particular intercostal neuralgia, that does not respond to treatment, may be a sign of a serious illness. Most of the complications that arise with thoracalgia are precisely a manifestation of the underlying pathology, which worsens against the background of constant pain.
Chest neuralgia itself, with a long-term severe course, can provoke the development of a hypertensive crisis or an attack of angina (less often, myocardial infarction). Severe, constant pain affects a person’s physical and mental state in different ways. Often severe symptoms of intercostal neuralgia on the left or right significantly complicate the patient’s life. He sleeps poorly, is nervous, cannot move normally and do his usual work.
Pain in the intercostal spaces does not allow the patient to perform full breathing movements, which leads to a decrease in oxygen supply to the body and the development of hypoxia. Sometimes neuralgia is accompanied by such debilitating pain that it contributes to emotional exhaustion, and this is a serious complication, since this condition causes depression.
Methods for treating intercostal neuralgia
Drug therapy. There is a wide variety of drugs to eliminate pinched nerves: painkillers, anti-inflammatory drugs, those that increase the body’s defenses, injections, blockades. All drugs have a long list of side effects, so before using them you need to consult a specialist. Any medicine is selected depending on the severity, tendency to allergies, and the characteristics of the course of the disease.
- Anticonvulsants inhibit the conduction of pain impulses.
- Tricyclic antidepressants relieve tension in chronic pain syndromes.
- Venotonics and diuretics relieve swelling.
- Corticosteroid drugs are used in cases of severe inflammation.
- Vitamins B1, B6 and B1 accelerate the restoration of the nerve sheath, reduce inflammation and pain.
Compresses. They can be either hot or cold. They are used to reduce inflammation and also to reduce pain. This is only a temporary measure and has no therapeutic effect.
Other methods: gymnastics, shock wave therapy, massage, physiotherapy - alleviate your condition, ensuring complete recovery. And these procedures do not harm the body.
Physiotherapy and exercise therapy. Intercostal neuralgia is often caused by poor posture. The goal of physical therapy is to relieve the back muscles and open the chest. Therapeutic exercises should be performed 3-4 times a day.
Physiotherapy includes acupuncture, osteopathy, manual therapy, massage with warming creams and ointments, and kinesiotaping. They relax the fascia of the chest and back. Heat helps to temporarily relax muscles, relieve swelling, inflammation and acute pain.
Massotherapy. It should be done while sitting. When performing the procedure, the intercostal spaces are rubbed and stroked with your fingertips. In addition to this, they knead and rub the back muscles with both hands. During acupressure massage, use your fingers to press on active points associated with one or another affected organ. Acupressure can stimulate defenses and relieve pain.
Neuralgia during pregnancy
If intercostal neuralgia appears in a pregnant woman, how to diagnose it and how to treat it is decided by a neurologist together with a gynecologist. Therapy is selected taking into account possible negative effects on the fetus. Self-medication in this situation is considered unacceptable, as this can have a negative impact on the health of the expectant mother and child.
To prevent chest neuralgia from appearing during pregnancy, it is advisable to follow preventive measures. If a woman has previously had attacks of thoracalgia, then at the stage of preconception preparation she should visit a neurologist and osteopath. The doctor will conduct a diagnosis, and then the neurologist will give a number of recommendations on how to treat intercostal neuralgia. An osteopath will identify possible causes of neuralgia and conduct a treatment session aimed at eliminating them.
Forecast and prevention of intercostal neuralgia
In most patients, intercostal neuralgia can be completely cured. If thoracalgia occurs against the background of a herpetic infection, relapses are possible.
If adequate treatment of neuralgia does not bring the desired result, a more “deep” diagnosis is carried out to search for the possible cause of this condition. First of all, spinal hernias, benign and malignant tumors are excluded.
To prevent neuralgia of the intercostal branches from recurring, and its symptoms in adults to manifest themselves less painfully, doctors recommend the following preventive measures:
- follow the canons of a healthy lifestyle: give the body adequate physical activity, eat right, actively relax in the fresh air, give up bad habits, etc.;
- maintain normal functioning of the immune system;
- monitor posture and spinal health;
- promptly treat chronic diseases and infectious processes;
- if possible, visit the pool and harden yourself;
- undergo preventive examinations on time;
- undergo regular scheduled examinations by an osteopath approximately once every six months.
If a person has previously had thoracic neuralgia, he should not be overcooled, be in a draft, expose the body to excessive physical stress, perform sudden movements or remain in an uncomfortable position for a long time. In addition, it is necessary to eliminate or minimize as much as possible stress and any unfavorable factors that can cause symptoms of intercostal neuralgia on the left, right or both sides.
Did you like the article? Add the site to your browser bookmarks
Diagnostics
The examination of the patient begins with a standard examination by a cardiologist. The doctor conducts auscultation of the heart to identify signs of organic pathology - rough noises, deafness, splitting or accentuation of tones. Since it is quite difficult to find out the cause of tingling during a clinical examination, laboratory and instrumental diagnostic methods are used:
- Electrocardiography.
Based on the results of the study, the doctor accurately determines the presence of arrhythmia and its type. Violation of repolarization and a decrease in the voltage of the teeth indicates myocarditis or coronary myocardial diseases. If there are difficulties in diagnosis, daily ECG monitoring is recommended. - Ultrasound of the heart.
Echocardiography is effective in identifying organic cardiac pathology that causes tingling in the heart. According to echocardiography, the thickness and uniformity of contraction of the heart wall, ejection fraction, and the condition of the pericardial cavity are assessed. Blood flow is measured using Doppler ultrasound. - Radiography.
A standard chest x-ray is necessary for a preliminary assessment of the size and shape of the heart and visualization of the contours of the great vessels. For a more detailed study of anatomical structures, an MRI is performed. - Blood tests.
Inflammatory damage to heart tissue is manifested by leukocytosis and increased ESR in the hemogram. An increase in acute phase proteins is characteristic. In coronary diseases, an increase in the levels of total cholesterol and LDL fraction is typical. If necessary, myocardial markers are measured.
If cardiac neurosis or peripheral nerve damage is suspected, the patient is referred to a neurologist. In addition to assessing the neurological status, the specialist may prescribe EEG, electroneuromyography, CT and MRI. For psychogenic neuroses, a psychiatrist should participate in the diagnostic search. Signs of articular pathology are an indication for consultation with a rheumatologist.