How to treat intercostal neuralgia on the right or left?
Intercostal neuralgia is a reflex pain syndrome that occurs when the intercostal nerves are compressed, irritated or inflamed. Otherwise it is also called thoracalgia. This phenomenon is unpleasant, as it is accompanied by intense pain.
Clinical manifestations are very similar to the symptoms of a number of diseases of internal organs, in particular the heart. That is why many patients, frightened by an attack of intercostal neuralgia, turn to a cardiologist or begin to self-medicate by taking heart medications. The latter, along with the lack of correct diagnosis and adequate treatment, does not bring relief, but only aggravates the patient’s condition.
Since thoracalgia is quite common among older and older adults, being fully aware of it will ensure health and well-being during these stages of life.
Causes and risk factors
Intercostal neuralgia is not inherently an independent disease. From a medical point of view, this is a complication caused by the underlying disease or pathological process occurring in the body.
The human chest has twelve pairs of ribs, which are attached to the thoracic vertebrae of the spinal column at the back. The thoracic nerves, exiting through the intervertebral (foraminal) foramina and branching, are located between the ribs.
The mechanism of occurrence of intercostal neuralgia is simple. Seizures can be caused by:
- pinching or inflammation of nerve endings in the intercostal space;
- pinching of the roots of the thoracic spinal nerves at the point of their exit from the spinal canal.
The most common causes of neuralgia of the intercostal nerves are:
- osteochondrosis, spondylitis, ankylosing spondylitis and other diseases of the thoracic spine;
- excessive physical activity;
- tumors of the thoracic spinal cord;
- chest injury;
- sudden unsuccessful movement;
- general hypothermia of the body, hypothermia of the chest and back;
- pathologies of the upper gastrointestinal tract;
- forced awkward body position;
- herpetic infection.
The contributing factors are:
- age-related changes in blood vessels;
- metabolic disorders (diabetes mellitus);
- diseases of the nervous system;
- infectious and inflammatory diseases;
- immunodeficiency;
- intoxication of the body;
- uncomfortable workplace.
In women, intercostal neuralgia can be caused by wearing tight underwear, as well as being underweight. In children and adolescents, intercostal neuralgia can occur during a period of intensive growth of the bone skeleton.
What is intercostal neuralgia
Intercostal neuralgia (scientifically known as thoracalgia) is a pathology in which the roots or the entire length of the nerves located between the ribs are compressed and irritated. A person experiences severe chest pain. Very often, patients think that this pain is cardiac, since the discomfort is felt specifically in the heart area.
Middle-aged and elderly people suffer from the disease more often due to degenerative changes in the body, affecting nerve fibers. Also, tumors and inflammation of peripheral nerve trunks contribute to the manifestations of intercostal neuralgia. Women during pregnancy may also experience characteristic symptoms. This is caused by the expansion of the chest and abdominal muscles.
Factors in the development of pathology are:
- Injuries to the spine, ribs.
- Pinched nerves.
- Atherosclerosis and hypertension.
- Spinal diseases (osteochondrosis, scoliosis, hernias, disc protrusions, arthritis, osteoporosis, ankylosing spondylitis, tumors in the thoracic region).
- Diseases of the gastrointestinal tract (pancreatitis, ulcers).
- Lack of minerals and vitamins in the diet.
- Frequent stress.
- Local hypothermia.
- Diabetes.
- Prolonged and severe cough.
- Inflammation or excessive tension in the back muscles.
- Poisoning by poisons, drugs or microbial toxins.
- Injury to nerves located in the thoracic region.
Congenital malformations and spinal injuries, weak immunity, diseases of the cardiovascular system and bad habits create the preconditions for the development of intercostal neuralgia.
In the vast majority of cases, the disease occurs as a result of irritation or pinching of the nerve by the intercostal muscles.
In this state, a large number of impulses arrive at the nerve endings, a lack of oxygen appears, and as a result, severe pain.
Symptoms of intercostal neuralgia
The main symptom of intercostal neuralgia is pain along the intercostal space. The intensity of pain can vary: from sharp, acute, severe, shooting (more often) to constant, medium intensity. The pain intensifies when the patient moves, when coughing and sneezing, and even when breathing. Often a person takes a forced position: leans towards the affected side in order to minimize the range of movements in it. Some patients, when coughing, laughing or sneezing, press their palm firmly against the affected intercostal space for the same purpose: to reduce the range of movements in this area so that it hurts less.
When the intercostal nerve on the left is damaged, the pain often imitates the sensations of angina pectoris: patients evaluate the pain as burning, with irradiation (spread) to the left arm, scapula, and spine. However, angina pain still does not depend on movements, coughing, laughter, etc., and, moreover, decreases after the patient takes nitroglycerin tablets or its analogues. However, in order not to miss such an important cardiac pathology, in doubtful cases the doctor prescribes an ECG for the patient. It is important not to confuse intercostal neuralgia with myocardial infarction, because the pain with it is also not reduced by nitroglycerin. Therefore, if pain suddenly arises in the heart area, you should not tempt fate, hoping for the best, but you need to play it safe: call an ambulance and undergo an electrocardiogram.
Differential diagnosis based on clinical manifestations is an important step in the treatment of patients. First of all, it is necessary to exclude heart pathology, since the treatment of intercostal neuralgia and heart diseases require different methods of therapy, and incorrect diagnosis and lost time in case of cardiac pathology can be decisive for the patient’s condition. The differences are primarily that:
- with neuralgia, chest pain persists for a long time, both day and night;
- the pain intensifies when changing the position of the body in space, coughing and sneezing, deep inhalation and exhalation, sudden movements, when palpating or squeezing the chest.
In case of heart disease, in particular angina pectoris, the resulting pain quickly passes after 5-10 minutes or is relieved by taking nitroglycerin. Movements and changes in body position, coughing and deep breathing do not cause increased heart pain, but may be accompanied by disturbances in heart rhythm and changes in blood pressure. To exclude the possibility of cardiac pathology in the presence of pain in the chest or under the left shoulder blade, it is necessary to urgently perform an electrocardiogram, and sometimes an x-ray.
Intercostal neuralgia: symptoms, diagnosis and treatment
Chest pain is always alarming. As a rule, the first thing a person thinks about is the heart. Statistics, widely revealed thanks to the media, also echo such fears: deaths from cardiovascular diseases confidently remain at the top of the sad list.
However, it is not only the heart that can hurt in the chest. Natalya Vladimirovna Umerenkova, a neurologist and leading specialist in the neurology department at the Expert Clinic Kursk, told us about intercostal neuralgia, one of the symptoms of which is chest pain.
— Unexpected chest pain is always alarming. What can hurt your chest?
Such pain is a signal for both the doctor and the patient. Many anatomical structures can hurt in this area. This is the heart in case of ischemic disease (angina pectoris, heart attack), large vessels (in case of dissecting aortic aneurysm). Pain occurs with tracheitis, pneumonia, accumulation of air in the pleural cavity (pneumothorax) and its inflammation, tumors of the lungs and mediastinal organs, pulmonary embolism, mediastinitis, pathology of the esophagus (inflammation, peptic ulcer).
You can read about the symptoms, diagnosis and treatment of pneumonia here
Pain can also be “reflected” into the chest when the pancreas, gall bladder, or stomach pathology are affected (peptic ulcer).
Sometimes pain can be of a psychogenic nature - for example, with an imbalance of the autonomic nervous system (also known as vegetative-vascular dystonia).
Vegetative-vascular dystonia - diagnosis or fiction? Read here
Accompanied by chest pain and diseases of the osteochondral structures of the chest and nerve trunks - including intercostal neuralgia.
— How do you understand that chest pain is threatening and an ambulance should be called immediately?
Here it is important not to miss, in particular, such pathologies as unstable angina, myocardial infarction, pulmonary embolism, and thoracic aortic aneurysm.
For this group of diseases there are common manifestations - “alarm signals” that you should definitely pay attention to. This is most often a fairly severe, acute pain, which differs from the pain noted earlier (if it was noted), and does not go away while taking nitrates. The pain may be accompanied by nausea, vomiting, sweating, and pale or bluish skin. Rapid heartbeat often develops, shortness of breath, suffocation, hemoptysis, drop in blood pressure, pre-syncope or fainting are possible. These signs are a reason to immediately call an ambulance.
— What is intercostal neuralgia?
Intercostal neuralgia is a complex of manifestations that develops when the intercostal nerve or nerves are irritated or compressed. There are doctors who regard it as an independent disease with a clearly defined picture, while others consider it a syndrome that can be caused by a variety of disorders. In any case, intercostal neuralgia is coded in ICD 10 (code G58.0).
— What kind of pain occurs with intercostal neuralgia? By what signs can it be distinguished from other pain?
Intercostal neuralgia is often characterized by a unilateral location of pain (right or left), which is semi-encircling in nature. The patient can describe it quite clearly, i.e. indicate its location, the course of distribution (usually along the intercostal space).
The pain is quite acute, can be constant (with periods of worsening) or paroxysmal. Longer than that with stable angina (with the latter, the pain usually goes away after 3-5 minutes at rest).
Pain with intercostal neuralgia has periods of worsening/improving, is quite clearly associated with physical activity, changes in body position, and can be provoked by coughing, sneezing, or deep breathing. In addition to pain, symptoms such as numbness, burning, pulsation, and involuntary muscle contraction are often encountered in the intercostal space.
The difference between pain in intercostal neuralgia and cardiac pain (in particular angina) also lies in the absence of irradiation to the left arm and lower jaw; no fluctuations in blood pressure; The duration of the pain syndrome also differs (with neuralgia, pain can be bothersome for a long time), there is no effect from taking nitrates, there are no symptoms signaling a serious pathology of the heart and blood vessels. The provoking factors in the occurrence of pain also differ (awkward movement and a deep breath can trigger an attack of pain with intercostal neuralgia); Adopting a pain-relieving position minimizes it in case of intercostal neuralgia, but does not affect the intensity of “heart” pain.
How to avoid running to a hospital bed? What do you need to know about health before buying a gym membership? Read more
— Can there be an increased body temperature with intercostal neuralgia?
No. If such a manifestation occurs, you need to look for another cause of pain in the chest.
— Why does intercostal neuralgia occur?
The mechanisms leading to intercostal neuralgia may be irritation or compression of the intercostal nerve. This may be due to osteochondrosis of the spine, curvature of the spinal axis, spondylosis, damage to the transverse costal joints; after injury to the ribs and chest, excessive muscle tension (in particular intercostal muscles); with excessive mobility of parts of the ribs on the lateral and anterior surface of the chest; Infringement of the 7th-12th nerves in the connective tissue sheaths of the rectus abdominis muscle is less common.
Does osteochondrosis exist? Find out here
Sometimes the cause of intercostal neuralgia can be the herpes zoster virus. In this case, it is coded in a different section of ICD-10, but the manifestations will be generally the same.
In some cases, intercostal neuralgia can occur after suffering from influenza and a number of infectious diseases.
Additional risk factors for the occurrence of intercostal neuralgia may include diabetes mellitus, alcoholism, and impaired absorption of B vitamins.
“Triggering” moments can be a combination of factors: hypothermia, sudden and/or awkward movement, interventions on the thoracic spine (not entirely correct manual therapy, surgery, etc.).
— Can intercostal neuralgia go away on its own or does it need to be treated?
Sometimes it can go away on its own. However, in the absence of treatment, it is likely that the duration of the disease and the treatment time will increase (with therapy, the period of temporary disability is usually 7-14 days), and the process may become chronic, when the pain can last for weeks, and in the case of the herpetic nature of the disease - for months and years.
The question is also that during self-diagnosis, i.e. when the patient decided that he had intercostal neuralgia and did not go to the doctor to prescribe treatment, you can “miss” some other, often serious, diagnosis that resembles neuralgia in its manifestations. At the same time, the consequences without treatment may not be so harmless, and, in addition, time will be lost.
— What is the risk of intercostal neuralgia if it is not treated? How dangerous is this diagnosis?
If left untreated, recovery time may increase or the pain may become chronic.
— Which doctor should you contact for symptoms of neuralgia?
Since intercostal neuralgia can be confused with much more serious, life-threatening diseases, you should first immediately consult a physician or general practitioner. And only after excluding these pathologies, see a neurologist.
You can make an appointment with a therapist here
Please note: consultations are not available in all cities
Occasionally, when there is a need for therapeutic blockades, the help of a neurosurgeon or traumatologist may be needed.
— How is intercostal neuralgia diagnosed?
An ECG and chest x-ray are required, and body temperature is measured.
Are x-rays dangerous? Yulia Aleksandrovna Rutskaya, head of the radiation diagnostics department, tells
"Clinics Expert Kursk"
According to indications - radiography or MRI with myelography of the thoracic spine. Sometimes tests are prescribed to confirm/exclude an acute inflammatory process.
— What should you never do if you have intercostal neuralgia? For example, is it possible to warm the area of pain with a heating pad? Exercise? Go to the bathhouse?
None of the above.
— What is the prognosis for this disease? Is intercostal neuralgia successfully treated?
With correct diagnosis and timely treatment, the prognosis is favorable. This pathology is highly treatable.
— What needs to be done to prevent the development of intercostal neuralgia?
For prevention, it is necessary to avoid hypothermia, sudden and awkward movements (especially if they are unfamiliar, insufficient training or “warming up” before training; within the framework of the work performed); optimize body position in the workplace; engage in physical therapy; undergo regular medical examinations; do not hesitate to consult a doctor if any health symptoms appear.
For reference:
Umerenkova Natalya Vladimirovna
In 2004 she graduated from Kursk State Medical University.
In 2004-2005, she completed an internship in neurology at the above-mentioned university.
Since 2015, he has been working at Clinic Expert Kursk LLC, and is a leading specialist in the neurology department. Receives at the address: st. Karl Liebknechta, 7
Localization of pain
- Referred pain. Referred pain, as a rule, is a consequence of the development of a pathological process in the internal organs (diseases of the retroperitoneum, aortic aneurysm, pathology of the digestive tract, coronary artery disease).
- Radiating pain. The mechanism of development of this pain has not been fully studied to date. According to experts, parts of the nervous system may misinterpret the source of pain due to the presence of common pathways through which both visceral and somatic pain are carried out. Referring pain, resulting from stretching, irritation or compression of a somatic nerve or nerve root, is more intense. With physical activity, sneezing or coughing, the pain may intensify, and can often spread to the affected area of the body.
- Local pain. Its cause can be any pathological process aimed at pain receptors of various tissues, muscles, ligaments, skin, tendons, bones, joints, etc. In this case, pain develops directly in the area of damage.
Symptoms
The symptoms of this phenomenon can be either obvious or disguised as diseases of internal organs and other pathologies. Often, treatment for a pinched nerve in the thoracic spine is needed by people who have gone to the doctor with complaints about the heart, stomach and other internal organs, since the pain innervates them. It is worth knowing how a pinched nerve manifests itself in order to recognize the condition in time and consult a neurologist
.
Chest pain
Symptoms of pinching in the thoracic spine are often very similar to symptoms of an angina attack. The person complains about the following:
- there is severe pain and burning under the shoulder blade and in the chest;
- there is not enough air and you can’t breathe in completely;
- hands go numb;
- Cold sweat appears on the body.
To exclude the condition that occurs with angina pectoris, you can put two nitroglycerin tablets under your tongue. If you have heart problems, this remedy will eliminate them within 5 minutes, but if you have a pinched nerve, then the situation will not improve. In this case, there will be severe pain in the vertebral area.
Problems with the gastrointestinal tract
A person who is experiencing digestive problems due to back pain may need to find out what the symptoms and treatment of pinched thoracic spine may be. A person may note:
- Pain in the intestines when trying to change position.
- Spasmodic pain in the abdomen.
- Stool disorders.
Such symptoms may indicate not only pinching, but also a more serious condition - prolapsed intervertebral hernia or displacement of the vertebrae.
Diagnostics
After the doctor has collected the patient’s complaints and history of the development of the disease, additional examinations must be carried out to confirm the diagnosis.
The most informative and used of them:
- Chest X-ray - reveals disturbances in the structure of bone tissue, as the main cause of the development of neuralgia;
- Bacteriological blood test - if the cause of thoracalgia is an infection, it reveals the causative agent of the disease, in other cases the analysis remains unchanged;
- Complete blood count - normal values are typical, or a slight increase in leukocytes in the case of an inflammatory reaction in the nerve area;
- Magnetic resonance imaging - determines bone and cartilage changes, swelling, pinching or inflammation of the intercostal nerve;
- Computed tomography is a more accurate method compared to x-rays; it reveals smaller abnormalities in the structure of bone tissue;
- Ultrasound – used to differentiate neuralgia from other pathologies, with thoracalgia it remains unchanged;
- Electrospondylography – determines the pathology of the intervertebral discs and spine;
- Myelography - the spinal cord and intercostal nerves are examined using a contrast agent on an X-ray machine, and allows you to identify changes in the nervous tissue;
- Electromyography - determines abnormalities in muscle fibers along the affected nerve.
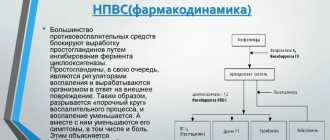
Drug treatment
For neuralgic pain, drug treatment at home is the main thing. Typically, the following drugs are prescribed for neuralgia:
- Anti-inflammatory drugs: piroxicam, diclofenac, indomethacin, ibuprofen and voltaren. These medications are used externally in the form of ointments, and internally in the form of capsules, tablets and injections.
- Medicines that relieve the main symptom – pain: spasgan, sedalgin or analgin.
- Muscle relaxants sirdalud, baclofen, clonazepam (relieve one of the causes of neuralgia - muscle spasm).
- Medicines such as viperalgin, vipratox, apizartron and virapin, containing bee and snake venom, significantly alleviate the condition of patients.
- Anesthetics (lidocaine and novocaine), which are used to perform blockades in acute conditions, injecting them intramuscularly.
- B vitamins, the deficiency of which negatively affects the nervous system and provokes intercostal neuralgia.
- Sedatives are prescribed for insomnia caused by excruciating neuralgic pain.
Non-drug therapy
Intercostal neuralgia can be treated without the use of medications using the following methods:
- Using massage movements of the hands with a warming ointment or cream applied to them, deep warming and relaxation of the muscles that create a protective “corset” (or, conversely, leading to compression of the intercostal nerve) is achieved. It is performed in a sitting position with rubbing and stroking the intercostal spaces with the fingertips and subsequent kneading of all the spinal muscles.
- Unlike the previous method, acupressure applies pressure to the physiologically and bioenergetically massaged chest points associated with the diseased organ, leading to pain relief, relaxation and a quick effect by stimulating the body’s own defense mechanisms.
- Similar physiologically and bioenergetically justified effects are the methods of acupuncture (acupuncture), cauterization, and laser therapy, which make it possible to quickly neutralize muscle imbalance in the deep back muscles with the elimination of pain.
- Treatment of intercostal neuralgia by placing massage cups on the back pursues the same goals, being a simple and harmless technique for the body (provided there are no contraindications to its use).
- Manual techniques are resorted to after the end of the acute period. They consist in returning to their proper places the bone structures and muscles and ligaments that serve them that have been displaced during the disease and are carried out exclusively after manual diagnosis. As a result of the impact, the diameter of the narrowed tunnels (bone-tendon and musculoskeletal) returns to normal and the function of the pinched nerve is restored.
Like all the above methods, physiotherapeutic methods using:
- magnetic or electromagnetic field;
- ultrasonic, ultraviolet and infrared radiation;
- electro- and iontophoresis, with a dose of the drug substance that is minimal for the risk of the fetus.
Tablets for intercostal neuralgia
Of the medications that alleviate the course of this disease, the first place goes to analgesics (analgin, sedalgin) and non-steroidal drugs (ibuprofen, piroxicam, indomethacin), which have anti-inflammatory properties. They should be taken regularly for pain prevention purposes, without waiting for a new attack to occur.
Drugs that belong to the group of muscle relaxants (tizanidine or baclofen) help not only eliminate pain, but also relieve muscle spasms in the area of injury. Medicines in this group must be used with caution, especially for people driving and associated with work involving a high concentration of attention.
To relieve nervous tension, you can take sedatives. Be sure to carry out vitamin therapy . Complexes containing daily dosages of B .
Intercostal neuralgia with unbearable pain can be successfully relieved with lidocaine or novocaine blockades . These procedures are usually performed in specialized centers. But in particularly severe cases of the disease, the prescription of steroids, usually prednisone, is indicated.
A good effect is achieved when physiotherapeutic methods . They include UV irradiation of the corresponding paravertebral region, electrophoresis with lidocaine, especially in the acute period. When the phase transitions from acute to subacute, darsonvalization, microwave therapy, and phonophoresis are prescribed. Reflexology is widely used for this pathology.
Treatment of intercostal neuralgia using traditional methods
There are many folk recipes that can be used to treat intercostal neuralgia at home. However, I would like to note that since the reasons causing it are quite serious, you should not self-medicate and check whether the disease can go away on its own. Secondly, it is necessary to accurately confirm the diagnosis, excluding pathologies of the cardiovascular system and other disorders. Otherwise, the underlying disease can be triggered.
- Sage baths with sea salt help relieve tension and reduce pain.
- Rubbing with tincture of valerian or infusion of birch buds is effective - their effect is in no way inferior to industrially produced ointments. However, it is better not to apply alcohol compresses at night - prolonged exposure to alcohol can lead to burns.
- Warming up also helps, but the thermal effect for intercostal neuralgia should not be direct, that is, do not apply a heating pad, hot potato or egg, but wrap yourself in a downy scarf or knitted woolen item. If you heat the painful area too much, the pain will go away for a short time and then such an effect will only increase the swelling of the soft tissues and bring even greater pain.
- For topical application to affected areas, use black radish juice or horseradish juice. Compresses based on steamed flax seeds help a lot.
To prevent chronic neuralgia, it is important to eliminate the effects of harmful concomitant factors, such as psycho-emotional stress, heavy physical activity, alcohol abuse, and also to treat existing diseases of the nervous system, systems and organs, etc.
Osteochondrosis of the chest. Intercostal neuralgia
Osteochondrosis is a degenerative-dystrophic disease of the cartilage tissue of the human body, affecting the most mobile joints. Most often, the cervical and lumbar spine suffer from the disease. treatment of osteochondrosis of the thoracic region is noted by statistics much less frequently, but due to the anatomical specificity of the structure of this segment, in most cases the disease is diagnosed quite late and requires more time and effort to cure the patient.
Features of the structure of the thoracic spine
The thoracic segment of the spine contains 12 vertebrae connected to the ribs and sternum, forming a rather rigid structure designed to protect the internal organs (lungs, heart, liver, digestive system, etc.). Functionally, the chest is inactive, especially when compared with the cervical spine, and does not experience such significant mechanical stress as the lower back. Therefore, the symptoms of osteochondrosis in this area in the early stages of the disease do not cause much discomfort, and therefore practically do not alarm patients with their severity.
Pathology is usually discovered unexpectedly for the patient, during an x-ray or when serious pain has become a signal of the development of complications such as: protrusion or herniation of intervertebral discs, spinal canal stenosis, displacement of vertebral bodies, etc. Provocateurs of damage to the thoracic spine can be youthful postural disorders, such as scoliosis or Scheuermann-Mau kyphosis.
Symptoms of osteochondrosis of the thoracic region
Symptomatic manifestations of the disease can be different and are directly related to the location of the lesion. First of all, these are pain sensations of a chronic, aching nature, especially after prolonged physical exertion, and acute pain with sudden movements (turning, bending, lifting weights, sometimes even when sneezing or coughing). Stiffness and spasms of muscles, limited movements become the body's response to pain.
When the upper vertebrae of the thoracic region are affected, the pain is localized in the shoulder girdle, and tingling occurs between the shoulder blades or in the sternum. Damage to the middle areas usually manifests itself as pain in the heart area (which has nothing to do with diseases of the cardiovascular system) and intercostal space or girdle pain just below the heart (resembling hepatic colic). The appearance of osteochondrosis in the lower part of the chest affects the functioning of internal organs and can radiate pain to the abdominal cavity or lower abdomen.
Spasms of muscle structures and circulatory disorders in the affected area provoke a lack of supply of cartilage tissue with water and nutrients. Gradually, the intervertebral discs dry out, lose mobility and elasticity, and over time, their walls (fibrous rings) crack and the gelatinous substance (nucleus) filling them protrudes outward, forming an intervertebral hernia, the treatment of which requires a more serious approach, and in some cases, surgical intervention .
Depending on the location of the formation of herniated discs, they can cause compression of nerve endings and the manifestation of neurological symptoms, such as decreased sensitivity in the upper girdle of the extremities, slowing down of reflex reactions, radiating pain from the shoulder to the hand, etc. Protrusion of the herniated formation into the spinal canal causes compression of the spinal brain and leads to partial or complete immobility (paresis, paralysis) of the upper half of the body and/or disruption of the functioning of internal organs.
Compression of blood veins or arteries often provokes headaches, surges in blood pressure, interruptions in the blood supply to the brain and other vascular pathologies. Quite often, osteochondrosis is accompanied by treatment for intercostal neuralgia or thoracalgia (these are severe pain caused by compression or irritation of the intercostal nerves).
intercostal neuralgia (thoracalgia)
Thoracalgia is one of the most powerful pain syndromes of an acute, piercing, aching, burning, paroxysmal or periodic nature, with difficulty and limitation of respiratory capabilities. It may be accompanied by increased sweating, pulsation or spasms of muscle tissue, decreased sensitivity, paleness or, conversely, redness of the skin. When palpating the spine in the thoracic area along the intercostal spaces, the patient feels a dull pain.
Tissue numbness is observed directly at the site of compression or nerve damage. The feeling of pain with neuralgia can be felt not only in the heart area, but can be felt under the collarbone, in the lower back, under the shoulder blades. In this case, a neurologist or chiropractor must clearly differentiate clinical symptoms to exclude heart pathologies or peptic ulcers.
The main signs for diagnosing thoracalgia:
- The pain syndrome does not go away for a long time (does not weaken either day or night). With angina, the pain subsides 15-20 minutes after taking nitroglycerin.
- The pain syndrome intensifies with changes in the position of the body, sudden movements, deep inhalations and exhalations, coughing, sneezing, and slight squeezing of the chest or pressing on it. Heart attacks do not give such a reaction to movements of the body in space, but may be accompanied by arrhythmia or surges in blood pressure.
- Pain caused by stomach colic is quickly relieved with antispasmodic drugs, but for neuralgia, such drugs will have no effect.
- The reasons for this condition of the patient are pinching of the nerve roots of the intercostal system at the point of their exit from the spinal column by intervertebral discs damaged or flattened by osteochondrosis, herniated formations, overgrown osteophytes (bone formations on the vertebrae), tumors or injuries of the chest.
- Thoracalgia, as a rule, affects older people, when all the reasons for the progression of the disease intensify against the background of age-related changes (slowdown of metabolic processes, inactivity, accelerated leaching of calcium and other trace elements from the body, changes in the cardiovascular system, etc.). In children and adolescents, intercostal neuralgia is practically not observed.
Treatment of the disease
It should be noted that with both thoracic osteochondrosis and intercostal neuralgia, it is necessary to treat osteochondrosis, since neuralgia is only a pain symptom caused by degenerative-dystrophic changes in cartilaginous tissues. As practice has shown, traditional conservative treatment of the spine still remains quite effective.
During the acute period of the disease, the patient is prescribed complete rest, a maximum reduction in physical activity in combination with medications. Medicines used for neuralgia:
- analgesics - orally, intramuscularly, locally (in the form of novocaine or lidocaine blockades);
- non-steroidal anti-inflammatory substances - to relieve inflammation and swelling of soft tissues;
- muscle relaxants - to eliminate muscle spasms and release nerve roots;
- complexes of microelements and B vitamins - for general strengthening of the body and calming the patient’s nervous system.
When the pain syndrome subsides, you can begin the main therapy. It will consist of physiotherapeutic procedures, special dosed physical activity, exercise therapy, massages, attending manual therapy sessions, and diet.
An important role in the treatment of osteochondrosis of the thoracic spine is played by the patient’s attitude, his desire to recover and return to normal life.
It requires a rethinking of some life habits, awareness of giving up bad habits, increased physical activity, good nutrition, morning exercises, constant monitoring by the attending physician and an annual sanatorium-resort vacation. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Exercises
Physical therapy (physical therapy) is an effective way to treat neuralgia due to the anatomical structure of the human body. The nerves are located in the grooves of the ribs, which are covered by muscles. Spasmed muscles put pressure on nerve trunks, which causes pain. Exercises relax the muscles of the back and chest, improve blood circulation, and as a result the pain goes away. Gymnastics are prescribed only after acute pain has been relieved.
When performing physical exercises, you must consider some rules:
- Classes begin with a light warm-up - the body should be warmed up.
- The load must be increased gradually.
- You can't exercise through pain.
- Movements should be careful and smooth.
- Exercises should be aimed at strengthening the back muscles and stretching the spine.
- When performing exercises, you need to relax your back muscles as much as possible.
- You need to study every day, without skipping.
Gymnastics using the method of Dr. Bubnovsky is very effective. The essence of his technique: no medications, the medicine will be exercises, including those performed on special simulators. These exercises increase blood circulation and relax the deepest muscles.
How to treat?
It is necessary to choose a treatment method depending on what preceded the pinched nerve in the thoracic spine. However, there are general rules for treating pinched nerve roots that will help you get rid of the unpleasant condition.
Drug treatment
If you go to the doctor with complaints of back pain and you are found to have an injury, you will be prescribed a list of medications. These will be:
- antispasmodics;
- drugs to improve blood circulation;
- medications for inflammation;
- vaso-strengthening.
Additionally, painkillers may be prescribed depending on the general condition of the patient. As soon as the condition improves, other treatment methods can be used.
Physiotherapy
Physiotherapy is combined with gymnastic exercises, which allow you to recover and prevent recurrent injuries in the future. If you are experiencing pinching in the thoracic spine, you may be prescribed physical therapy:
- ultrasonic;
- laser;
- electrical stimulation of muscle tissue.
However, all these treatment methods can be used only after the patient’s general condition has improved and pain has been relieved.
Surgical intervention
As a rule, during the treatment of pinched nerve tissue, surgical interventions are avoided. But they will be indicated in a number of cases when there is no improvement in the condition for a long time, and the situation is getting worse. Radical treatment methods will be indicated if:
- conservative treatment was not effective;
- the pain spread further;
- the muscles began to atrophy;
- complications have appeared that affect the functioning of internal organs;
- pathological processes occurred in the intervertebral discs.
In such a situation, in addition to surgically eliminating the cause of the pain, surgery may be necessary to enlarge the hole in the intervertebral disc. But most often, treatment with medications and exercises for severe pinching of the thoracic spine can achieve the desired result, and surgery is a last resort.
Prevention
Specific prevention of neuralgia of the intercostal nerves has not been developed; general strengthening measures will help prevent the development of pathology. Recommended:
- avoiding hypothermia;
- hardening of the body;
- a healthy lifestyle, including regular moderate physical activity and a rational, balanced diet;
- measures to help prevent spinal curvature or treat an existing curvature;
- timely treatment of spinal diseases, chest injuries, pathologies of internal organs;
- work in comfortable conditions, with prolonged forced body positions, take breaks for a short warm-up.