Hippocampal sclerosis or Ammon's horn sclerosis, or medial temporal sclerosis is a set of changes characterized by a decrease in the volume of nervous tissue and loss of neurons in the medial temporal lobe. Clinically, hippocampal sclerosis manifests itself as epilepsy, often uncontrollable with medications, but in a significant number of cases curable with surgery.
The very first macroscopic description of a densified and reduced volume of the hippocampus in patients with epilepsy was made in 1825 by Bouchet and Cazauvieilh. In 1880, Sommer first described the microscopic picture of the sclerotic hippocampus in epilepsy, including noting that the loss of neurons in the hippocampus is segmental in nature, and the greatest loss of neurons occurs in the Sommer sector or CA1 segment of the hippocampus. A clinical description of epileptic seizures in patients with temporal lobe pathology was made by Hughlings Jackson in 1885, and in 1935 Stauder identified a connection between FH and the clinic of temporal lobe epilepsy. Sano and Malamud in 1953 confirmed the connection of hippocampal sclerosis with electroencephalographic signs of temporal lobe epilepsy. In the 50s of the 20th century, with the development of epilepsy surgery, intravital diagnosis of FH became possible. This is how Penfield described the so-called incisural sclerosis - thickening of the hippocampus, amygdala, and uncus, which was noted intraoperatively during surgery for temporal lobe epilepsy. Falconer proposed temporal lobectomy (removal of the anterior 2/3 of the temporal lobe neocortex and medial structures) for the treatment of temporal lobe epilepsy, with the most common histological diagnosis in his series of patients being hippocampal sclerosis. Later, more selective surgical techniques were proposed, which consisted in removing only the medial structures of the temporal lobe.
Today, hippocampal sclerosis is the most common histological diagnosis in adult patients undergoing surgery for epilepsy. The hippocampus is located in the medial parts of the temporal lobe and consists of two bent strips of nervous tissue nested inside each other: the dentate gyrus and the hippocampus itself (Ammon's horn or cornu Ammonis (CA)). In histological terms, the hippocampal cortex belongs to the archicortex, represented by three layers of neurons. The outermost layer of the hippocampus, forming the medial wall of the temporal horn of the lateral ventricle, is called the alveus and is formed by axons emerging from the hippocampus. This is followed by the stratum oriens (represented by axons and interneurons), then the layer of pyramidal cells, which are the main cellular elements of the hippocampus, and finally the deepest layer of the stratum lacunosum and moleculare, represented by dendrites, axons and interneurons. Important for understanding the various types of damage to the horn of Ammon during its sclerosis is the division of the pyramidal layer into 4 sectors proposed by Lorente de No (CA1, CA2, CA3 and CA4). The most pronounced layer of pyramidal cells is located in the CA1 sector, which continues into the part of the parahippocampal gyrus called the subiculum. The CA4 layer is adjacent to the concave part of the dentate gyrus. The dentate gyrus is a C-shaped structure with three layers of cells: the outer molecular, middle granular and inner layer of polymorphic cells, which merge with the CA4 layer of the hippocampus.
Structural changes in hippocampal sclerosis can vary from minimal, limited to one of its SA sectors, to severe, extending beyond the medial temporal lobe. The description of pathological changes in the structure of brain tissue in hippocampal sclerosis is distinguished by an exceptional variety of terms and the presence of several classifications with different concepts describing the same histological substrate.
Hippocampal sclerosis - what is it?
Hippocampal sclerosis is a form of epilepsy that is characterized by a decrease in the volume of nervous tissue and loss of neurons in the medial temporal lobe. Clinically, this pathological process is manifested by attacks of epilepsy. Sometimes this condition can be controlled with medication, but in some cases surgery may be required.
Hippocampal sclerosis often occurs in older people after a stroke. At risk are those people who suffer from high blood pressure or diabetes.
Causes
The following causes of hippocampal sclerosis are known:
- hereditary predisposition;
- hypoxia of brain tissue;
- brain injuries;
- infections.
Today, the following theories of the development of hippocampal sclerosis are considered the main ones:
- the influence of febrile seizures, leading to regional metabolic disorders and swelling of the temporal lobe cortex. Neuronal death occurs, local gliosis and atrophy develop, resulting in a decrease in the volume of the hippocampus and a reactive expansion of the sulcus and the inferior horn of the lateral ventricle.
- acute circulatory disorders in the basin of the terminal and lateral branches of the posterior cerebral artery cause basal ischemia of the temporal lobe, secondary diapedetic sweating, neuronal death, gliosis and atrophy occur.
- disruption of the development of the temporal lobe during embryogenesis.
Why choose MRI?
For pathologies localized in the brain, doctors recommend choosing magnetic resonance imaging. This is due to a number of advantages of the technique:
- Thanks to MRI, it is possible to obtain a number of images, including cross-sectional images.
- High image quality and detail.
- If necessary, a contrast agent can be used, which increases the information content of magnetic resonance imaging.
- This type of diagnosis has a small list of contraindications and does not cause any side effects.
- The procedure is completely non-invasive. Accordingly, the research process does not cause pain or discomfort.
- Magnetic resonance imaging is considered absolutely safe because it excludes exposure to radiation to the body.
- Possibility of identifying a pathological process even at an early stage of development.
VideoEEG monitoring solves several problems:
1. Allows you to exclude pseudo-seizures and non-epileptic paroxysms, including when they are combined with actual epilepsy.
2. Makes it possible to evaluate in detail the semiology of the attack and compare it with the dynamics of its epiactivity: its lateralization and regional localization.
3. Long-term recording makes it possible to determine the lateralization and localization of interictal activity. The most successful option in terms of a favorable outcome of epilepsy surgery is the coincidence of lateralizing and localizing symptoms in an attack with the data of the ictal and interictal EEG and MRI patterns. In the presurgical examination, the issue of duration of videoEEG monitoring is significant. It is known that the probability of registering a paroxysm on a 30-minute EEG with a frequency of attacks once a week is about 1% [19], and long-term videoEEG monitoring with an average duration of 7 days does not reveal interictal activity in 19% of patients [20]. The question of the required duration of video-EEG monitoring is important from the point of view of the mandatory recording of ictal events on the EEG when determining indications for surgery. A number of epileptologists believe that with a characteristic clinical picture and history of the disease, a picture of hippocampal sclerosis on MRI, registration of an ictal event is not necessary when there is more than 90% lateralization of interictal epiactivity in the temporal region on the affected side [21]. In most cases, the resolution of scalp EEG is sufficient to correctly lateralize the seizure onset zone in temporal lobe epilepsy and, in the context of consistent seizure semiology and MRI data, to determine a surgical treatment strategy.
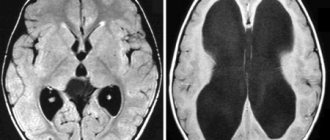
MRI diagnosis of HS is the next fundamental stage of presurgical examination. It should be performed according to an epileptological protocol, the main characteristics of which include small slice thickness and high magnetic field strength [6]. The optimal condition for performing MRI is the interaction between the epileptologist and the radiologist, when the planning of the study is carried out taking into account the expected localization of the epileptogenic zone. Hippocampal sclerosis on MRI has characteristic signs: a decrease in the volume of the hippocampus and disruption of the structure of the SA layers, a hyperintense signal in T2 and FLAIR mode [6] (Fig. 4). Atrophic changes are often detected in the ipsilateral amygdala, pole of the temporal lobe, fornix, and mamillary body. High-resolution MRI also aims to detect other epileptogenic brain pathologies located outside the hippocampus, i.e., dual pathologies such as focal cortical dysplasia. Without this task, an MRI examination will be insufficient to make a decision about surgery, even if it reveals signs of hippocampal sclerosis.
Rice. 4. MRI anatomy of normal and sclerotic hippocampus. a — T2, coronal section. Sclerosis of the right hippocampus: a decrease in its volume is determined, the absence of internal structure compared to the left hippocampus; b - the same section with explanations. The red line outlines the hippocampi (you can see a decrease in the volume of the right hippocampus), the blue line outlines the subiculum on the left. The yellow line in the center of the hippocampus is drawn along the deep part of the hippocampal sulcus (in Fig. “a” this sulcus is not defined in the right hippocampus). FG—fusiform gyrus, ITG—inferior temporal gyrus; c — coronal section in FLAIR mode, a decrease in volume and a hyperintense signal from the right hippocampus are visible.
A fundamental point in understanding the electrophysiology of medial temporal lobe epilepsy is the fact that scalp EEG itself does not reveal epiactivity in the hippocampus, as has been demonstrated in numerous studies using intracerebral electrodes. For epiactivity to appear in the temporal region on scalp EEG, it requires its propagation from the hippocampus to the adjacent temporal lobe cortex [22]. Moreover, the main clinical manifestations of an attack in medial temporal lobe epilepsy are associated with the spread of epiactivity to certain parts of the brain associated with the hippocampus: déjà vu is associated with excitation of the entorhinal cortex, a feeling of fear - with the amygdala, abdominal aura - with the insula, oroalimentary automatisms - with the insula and frontal operculum, dystonia in the contralateral hand - with the spread of excitation to the ipsilateral basal ganglia [6]. These anatomical and electrophysiological features may cause the patient to have seizures that are very similar to temporal paroxysms, but actually have an extrahippocampal and extratemporal onset.
As experience in the surgical treatment of temporal lobe epilepsy accumulated, it became obvious that removal of the medial structures of the temporal lobe makes it possible to get rid of seizures completely in 50-90% of patients, but in some cases the frequency of seizures does not change at all [6]. Data from studies of electrical activity of the brain using intracerebral electrodes and analysis of unsuccessful surgical outcomes have shown that in some cases the reason for the persistence of seizures after removal of the SG is the presence of a larger epileptogenic zone that extends beyond the hippocampus. Regions of the brain anatomically and functionally connected to the hippocampus, such as the insula, orbitofrontal cortex, parietal operculum, and the junction of the parietal, temporal and occipital lobes, can generate seizures that are similar in clinical and EEG picture to temporal paroxysms [23]. The concept of “temporal lobe epilepsy plus” has been proposed to describe situations where hippocampal sclerosis exists alongside an extratemporal seizure initiation zone. In this regard, it is important to determine the indications for invasive EEG studies for temporal lobe epilepsy caused by S.G. Warning symptoms are a taste aura, an aura in the form of vertigo, and noise. Interictal epiactivity is most often localized bilaterally in the temporal regions or in the precentral region. Ictal epiactivity in “temporal plus” forms is more often observed in the anterior frontal, temporoparietal and precentral regions [24]. Differential diagnosis of temporal lobe epilepsy from “temporal lobe epilepsy plus”, carried out by a qualified epileptologist, is key in planning surgical intervention and predicting the outcome of treatment.
Treatment of epilepsy associated with hippocampal sclerosis
The standard of care for patients with drug-resistant medial temporal lobe epilepsy is referral to a specialized center for presurgical examination and surgical treatment. Among the enormous number of publications confirming the effectiveness of surgery for temporal lobe epilepsy, it is advisable to note two key studies with the maximum level of evidence. S. Wiebe et al. [25] in 2001 conducted a randomized controlled trial, which showed that surgery for temporal lobe epilepsy in hippocampal sclerosis can get rid of seizures in 58% of cases, and with drug therapy - only in 8%. The basis for another study was the fact that the average duration of illness in patients treated with surgery is 22 years, and 10 years or more elapse between diagnosis of drug-resistant epilepsy and surgical treatment. J. Engel et al. [26] in a multicenter randomized controlled trial showed that continuation of pharmacotherapy when two drugs are ineffective in medial temporal lobe epilepsy is not accompanied by remission of seizures, while surgical treatment in such situations can be effective (in 11 out of 15 patients seizures stop).
Surgery for temporal lobe epilepsy has two obvious goals: 1) ridding the patient of seizures; 2) discontinuation of drug therapy or reduction of the drug dose. According to the literature, about 20% of patients stop taking anticonvulsants after surgery, 50% remain on monotherapy and 30% receive polytherapy. The third goal, less obvious but of fundamental importance, is to reduce the risk of sudden unexplained death in epilepsy (SUDEP), which is associated with a sharp reflex depression of cardiorespiratory function in patients with drug-resistant epileptic seizures [27].
The goal of surgical treatment of temporal lobe epilepsy includes complete removal of the epileptogenic cerebral cortex with maximum preservation of functional areas of the brain and minimization of neuropsychological deficits. There are two surgical approaches in this regard: temporal lobectomy and selective amygdalohippocampectomy. Both operations involve removal of the uncus, amygdala, and hippocampus. Selective access to the medial temple can be achieved through several different approaches. Temporal lobectomy also involves removal of the lateral neocortex of the temporal lobe (from 3 to 5 cm depending on the dominance of the hemisphere). Proponents of the selective approach proceed from the fact that preservation of the lateral neocortex allows minimizing neuropsychological deficits, in particular a decrease in verbal memory [28]. On the other hand, as already noted, pathological changes can extend beyond the hippocampus into the amygdala, pole of the temporal lobe and lateral neocortex. Invasive EEG studies using depth electrodes have shown that in 35% of cases with hippocampal sclerosis, epiactivity occurs in the pole of the temporal lobe earlier than in the hippocampus [29]. Also, based on the analysis of data from deep electrodes, several types of temporal lobe epilepsy have been identified: medial, medial-lateral, temporopolar, and the already mentioned “temporal lobe epilepsy plus” [23]. Thus, when choosing surgical treatment tactics, one should take into account the likelihood of a larger epileptogenic zone extending beyond the sclerotic hippocampus, which may make lobectomy more effective [28]. However, there is currently no class 1 evidence to support the superiority of any technique in terms of seizure control, neuropsychological outcome, or the need for postoperative antiepileptic drugs, so the choice of surgery depends on the surgeon's preference [28].
Surgery for temporal lobe epilepsy with hippocampal sclerosis, with sufficient experience of the surgeon, has minimal risks of neurological deficit (persistent hemiparesis - less than 1%, complete hemianopsia - 0.4%) [30]. An unresolved problem remains predicting the risk of memory impairment after surgery. It is known that after resection of the hippocampus of the speech-dominant hemisphere, about 35% of patients demonstrate worse performance in neuropsychological assessment of verbal memory [31]. The risk of verbal memory decline is increased in the case of late onset of the disease, high preoperative testing scores, SH of the dominant hemisphere, minimal changes in the hippocampus on MRI - these circumstances indicate that the epileptogenic hippocampus can maintain functional activity [31, 32]. However, it is difficult to determine the extent to which decline in verbal memory affects postoperative quality of life. To a large extent, the patient’s quality of life after surgery depends on careful control of attacks and elimination of concomitant depressive and anxiety disorders. Determining the indications for surgery in high-risk patients should be carried out with particular care, since if the epileptological outcome is unsuccessful, the patient will also experience cognitive deficits, which sharply reduce the quality of life. In this regard, it should be emphasized that a necessary condition for organizing surgical care for patients with epilepsy is the formation of a team approach to each clinical case, close interaction between an epileptologist, surgeon, neuroradiologist and neuropsychologist.
There is no conflict of interest.
Indications for the study
As mentioned above, the most informative method for diagnosing hippocampal sclerosis is magnetic resonance imaging. As a rule, a referral for research is issued by a neurologist, less often by a psychiatrist or oncologist. MRI of the hippocampus is most often part of a comprehensive diagnosis of the brain, but in some cases the doctor may prescribe a study of this particular area.
The study is prescribed for obvious signs of this pathological process.
The main symptom of hippocampal sclerosis is epileptic seizures. This condition may cause additional symptoms, for example:
- Severe memory loss.
- Periodic convulsions.
- The occurrence of panic attacks.
- Insomnia.
- Frequent headaches that do not go away even after taking painkillers.
- Dizziness may occur from time to time.
- Impaired concentration.
- Intellectual thinking suffers.
Magnetic resonance imaging can also be prescribed before surgery to clarify the location of the pathological focus. Diagnosis is also carried out in the postoperative period.
Contraindications
Before diagnostics, you should make sure that you have no contraindications to MRI.
Magnetic resonance imaging is not performed in the following cases:
- The presence of a pacemaker or metal structures in the body (non-removable type).
- Women do not undergo MRI during the first trimester of pregnancy; diagnosis can only be carried out as prescribed by a doctor.
- Magnetic resonance imaging in a closed tomograph is not performed if you are afraid of closed spaces.
- It is not recommended to do an MRI if there are serious abnormalities in the functioning of the nervous system or psyche.
If there is a need to use a contrast agent, you should ensure that:
- An allergic reaction to the drug used.
- Kidney or liver failure.
- Pregnancy and lactation.
Preparation rules
Here are some tips for preparing for a magnetic resonance imaging scan:
Clinic and diagnostics
The history of epilepsy due to hippocampal sclerosis is described mainly on the basis of numerous studies evaluating the effectiveness of surgical treatment of temporal lobe epilepsy. A frequent event in the anamnesis is an indication of an acute pathology of the central nervous system suffered in childhood (usually up to 5 years): febrile seizure status, neuroinfection, head injury. Stereotypical seizures begin between the ages of 6 and 16 years, and there may be a so-called latent period, which is determined by the time between the initial precipitating damage and the development of the first seizure. It is also not uncommon for situations when between the first seizure and the development of pharmacoresistance, a period passes, designated as “silent”. This feature of the course of the disease indicates its progressive nature. A characteristic cognitive deficit in FH may be memory loss, especially during uncontrolled attacks.
Diagnosis of epilepsy caused by hippocampal sclerosis is based on three main principles. The first is a detailed analysis of the sequence of symptoms in an epileptic attack or semiology, which depends on which areas of the brain the epileptic activity spreads to. The second is the analysis of EEG data and their comparison with the semiology of the attack and the third is the identification of epileptogenic lesions on MRI. Speaking about the semiology of an attack in temporal lobe epilepsy associated with HS, it is necessary to remember that, firstly, each of the symptoms individually is not specific, although there is a typical pattern in the course of an attack. Secondly, symptoms in a seizure appear when epileptic activity spreads to parts of the brain associated with the hippocampus, which itself does not produce clinical manifestations. The characteristic onset of a temporal lobe attack is an aura in the form of a rising sensation in the abdomen. Fear or anxiety is also possible if the amygdala is involved at the beginning of an attack. At the beginning of the attack, there may be a feeling of “already seen” (déjà vu). An alarming diagnostic aura is an aura in the form of dizziness or noise, which may indicate an extrahippocampal onset of an attack. The preserved ability to name objects and speak during an attack is an important lateralizing sign of damage to the non-dominant hemisphere. The change in consciousness is accompanied by a cessation of activity, while the patient has a frozen gaze with eyes wide open (staring). The next symptom after the aura and cessation of activity are automated actions: oroalimentary automatisms with chewing, smacking lips. Dystonia in the hand also often occurs on the contralateral side of the sclerosed hippocampus, which is associated with the spread of epiactivity to the basal ganglia and manual automatisms also appearing in the form of fingering objects with the hand in the ipsilateral hand. Among the lateralizing symptoms, postictal paresis, which indicates involvement of the contralateral hemisphere, and postictal aphasia with damage to the dominant hemisphere are important. These symptoms must be considered in the context of EEG data.
The basis of electroclinical diagnosis for hippocampal sclerosis is videoEEG monitoring, which consists of simultaneous video recording of an epileptic seizure and electrical activity of the brain. VideoEEG monitoring solves several problems: 1. It allows you to exclude pseudo-seizures and non-epileptic paroxysms, including when they are combined with actual epilepsy 2. It allows for a detailed assessment of the semiology of the attack and its comparison with the dynamics of seizure epiactivity: its lateralization and regional localization, 3 Long-term recording makes it possible to clarify the lateralization and localization of interictal activity. The most successful option in terms of a favorable outcome of epilepsy surgery is the coincidence of lateralizing and localizing symptoms in an attack with the data of the ictal and interictal EEG and MRI picture. A pressing issue in presurgical evaluation is how long videoEEG monitoring should be carried out. It is known that the probability of registering a paroxysm on a 30-minute EEG with a frequency of attacks once a week is about 1%, and long-term videoEEG monitoring with an average duration of 7 days does not reveal interictal activity in 19% of patients. An acute question in the presurgical examination for temporal lobe epilepsy concerns the required duration of video-EEG monitoring: is it a strict requirement to record ictal events on the EEG or can the decision about surgery be made based on the analysis of interictal activity. A number of epileptologists believe that with a characteristic clinical picture and history of the disease, the presence of hippocampal sclerosis on MRI, registration of an ictal event is not necessary when there is more than 90% lateralization of interictal epiactivity in the temporal region on the affected side on MRI. In most cases, the resolution of the scalp EEG is sufficient to correctly lateralize the seizure onset zone in temporal lobe epilepsy and, in the context of seizure semiology and MRI data consistent with it, to determine a surgical treatment strategy.
MRI diagnosis of hippocampal sclerosis is the next fundamental stage of presurgical examination and should be performed according to an epileptological protocol, the main characteristics of which include small slice thickness and high magnetic field strength. The optimal condition for epileptological MRI is the interaction between the epileptologist and the radiologist, when the planning of the study is carried out taking into account the expected localization of the epileptogenic zone. Hippocampal sclerosis on MRI has characteristic signs: a decrease in the volume of the hippocampus and disruption of the structure of the SA layers, a hyperintense signal in T2 and FLAIR mode. Atrophic changes are often detected in the ipsilateral amygdala, pole of the temporal lobe, fornix, and mammillary body. The purpose of high-resolution MRI also includes the detection of other epileptogenic pathology of the brain located outside the hippocampus, i.e., dual pathology, for example, focal cortical dysplasia, which makes a non-epileptological MRI study insufficient for making a decision about surgery, even if it reveals signs of hippocampal sclerosis.
How is an MRI done?
Magnetic resonance imaging is performed in a special diagnostic room with a closed-type tomograph. Before starting the study, the specialist will tell you about some of the features of magnetic resonance imaging:
- The patient's main task is to remain still. Even the slightest body movements can lead to blurred images and a decrease in the information content of the procedure.
- If loud noises frighten you, it is better to take earplugs with you, as there is a loud noise during operation of the tomograph.
- If you feel unwell during the examination, you have the opportunity to pause the examination at any time by pressing the panic button.
Let's take a step-by-step look at how magnetic resonance imaging works:
- First, the patient must change into clothes without metal fittings - hospital clothes or his own.
- You need to take off your shoes and lie on your back on a retractable table.
- If necessary, a contrast agent is injected into the vein.
- The lower and upper limbs are secured with soft straps.
- The table automatically moves inside the tomograph.
- The duration of the diagnostic study is from 30 to 40 minutes.
At the end of the diagnosis, you need to wait for the results of the examination. If necessary, tell your doctor that you want your results digitally.
MRI with contrast
In most cases, the diagnosis of hippocampal sclerosis is carried out with an additional contrast agent. This makes it possible to get more informative and clear pictures. The contrast agent is injected into the patient’s vein immediately before the start of the diagnosis. MRI with contrast is completely safe for the body. The contrast does not accumulate in the tissues; within 24 hours the drug is completely eliminated from the body. To speed up this process, it is recommended to drink more water. Before MRI with contrast, it is necessary to consult a doctor and exclude contraindications.
Decoding the results
After all the images are received, the doctor’s task is to correctly interpret them and make a diagnosis. Using magnetic resonance imaging, you can find out the exact dimensions of a given part of the brain and identify even minimal changes in the structures of the hippocampus and neighboring areas. Detailed photographs of this area of the brain of the organ give your doctor the opportunity to determine the diagnosis and treatment tactics.
We recommend seeking medical help as soon as the first warning signs appear. Be healthy!
Treatment
To reduce the symptoms of the disease, neurologists at the Yusupov Hospital prescribe antiepileptic drugs. The drug of first choice is Carbamazepine. Second-choice drugs include Valproate, Diphenin and Hexamidine. After treatment, some patients stop having attacks and go into long-term remission.
In cases of resistance to therapy and progression of hippocampal sclerosis, surgical treatment is performed in partner clinics. It involves removing the temporal lobe of the brain (lobectomy). After surgery, the number of attacks decreases in 70-95% of cases. If you are faced with the problem of hippocampal sclerosis and would like to receive qualified specialized medical care, call us. You will be scheduled for a consultation with a neurologist at the Yusupov Hospital.