Concussion is the most common pathological condition among the consequences of traumatic effects on the skull and brain tissue. This pathology is considered a relatively mild and reversible disorder of brain function, however, insufficient diagnosis of the consequences of injury can cause severe disturbances in its further activity.
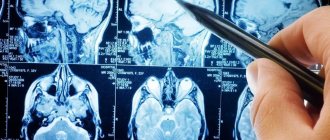
In this regard, MRI for concussion, which is performed painlessly and does not pose a risk to the patient’s health, serves as a reliable technique that allows us to fully assess the traumatic consequences.
Physiological manifestations of concussion
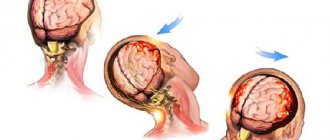
Pathology arises, as mentioned earlier, as a result of trauma, which can be of a different nature and affect any part of the patient’s skull. In this case, a lightning-fast increase in intracranial pressure develops, which is considered a direct etiological factor causing further functional disorders - loss of intercellular connections of brain structures, disruption of cellular nutrition, physicochemical transformations.
After a concussion, MRI is also performed to identify more serious consequences, including rupture of intracranial vessels and irreversible traumatic changes in areas of the brain. It is this type of research that is most informative regarding morphological and structural changes.
How to cure?
UGM is considered a mandatory indication for sending the victim to the hospital. Monitoring the patient and prescribing the correct course of treatment is provided by doctors from the neurological, surgical and rehabilitation departments. The conservative technique consists of the following rules:
- Corrective measures to normalize hemodynamic data with regular blood pressure checks.
- Help with respiratory functions.
- Monitoring and correction of intracranial pressure.
- The use of pharmacological drugs of a neuroprotective nature,
- Taking medications to adjust body temperature, relieve the patient from seizures, relieve pain in the head area, and prevent gag reflexes.
- Sometimes surgery is prescribed.
Surgical intervention is prescribed in 20% of cases. It is indicated in the case of progression of brain compression and the formation of dislocation syndrome during the presence of a lesion larger than 30 cubic centimeters with a displacement of the median elements by more than 5 millimeters. They may be accompanied by the development of worsening neurological symptoms. The operation is performed using craniotomy technology. If multiplication of disorders is detected, doctors remove this place. An osteoplastic intervention is performed during which bone and skin-aponeurotic tissues are reinstalled.
Symptoms
The symptoms of a concussion are pronounced and characteristic. In the first minutes after injury, the following clinical picture develops:
- vomit;
- pronounced increase in breathing;
- disturbances in the rhythm of the pulse (slowing or, on the contrary, increasing);
- partial or complete loss of memories of immediate events preceding the injury.
Most often, the patient’s recovery period is not accompanied by deviations from the norm in body temperature and blood pressure, but the following characteristic symptom complex of the rehabilitation period is observed:
- severe, varied headaches;
- dizziness;
- nausea;
- general weakness;
- inhibition of cognitive processes;
- noise in ears;
- sweating
It should be noted that all of the above symptoms are characteristic exclusively for patients of the young and middle age groups, while newborns and elderly people demonstrate a slightly different clinical picture. The fundamental difference here is the absence of a symptom of loss of consciousness.
After injury, young children exhibit frequent regurgitation, weakness and drowsiness, while older people report impaired coordination of movements and disorders of mental activity, including memory. Due to the uncharacteristic clinical picture and the vulnerability of the body, patients in this age group first of all need tomography for a concussion.
Material and methods
For 2 years, 87 patients, 65 (74.7%) men and 22 (25.3%) women, aged from 16 to 75 years (average - 36.0±1.5 years) with prolonged post-traumatic coma were observed. In 8 (9.2%) patients, the level of depression of consciousness in the acute period of injury corresponded to a mild coma (coma I), in 79 (90.8%) - moderate (coma II). The duration of coma in all patients exceeded 7 days (on average 13.4±2.7 days).
Analysis of the clinical and neurological picture in patients after an episode of prolonged coma was carried out on the basis of the dynamics of vital functions, neurological status and the patient’s reactions to the presentation of external stimuli. VS was diagnosed taking into account the criteria of the Multisociety Task Force on Persistent Vegetative State (MSTF on PVS, 1994) [1]. The diagnostic criteria for VS were the lack of conscious perception of one’s own personality and the surrounding world, voluntary, purposeful movements, both spontaneous and in response to external stimuli, verbal expression and understanding of spoken speech; the presence of intermittent episodes of wakefulness observed during the sleep-wake cycle, preservation of the autonomic functions of the hypothalamus and brain stem to the extent that allows maintaining the patient’s vital activity during medical therapy, dysfunction of the sphincters, various variants of spinal and brain stem reflexes.
Low consciousness was diagnosed based on the Aspen Working Group criteria [3]. The criteria for its diagnosis were the patient’s execution of simple/monosyllabic commands (show tongue, open/close eyes, close/open mouth, etc.), verbal and gestural responses/reactions of the patient of the yes/no type (despite the accuracy of their execution), an episode of meaningful verbalization, simple reactions/answers of the patient, related in content to the presented tasks/stimuli and different from reflex ones (emotional reactions (smile/crying) in response to a corresponding visual or verbal external stimulus, but not an external stimulus of a neutral nature; purposeful movements; holding objects in a way/manner corresponding to the size and shape of the object; fixation and consistent movement of the gaze in response to addressing or approaching the patient). The listed clinical signs may not be constant, but they are necessarily reproducible.
A level of functioning of patients higher than “low consciousness” was determined based on the constant ability to functional interactive communication (through verbalization, writing, gesturing) and/or functional use of at least two everyday objects.
Dysautonomia was diagnosed when patients had at least five of seven criteria: tachycardia (more than 120 beats per minute), tachypnea (>30 breaths per minute), increase in muscle tone, appearance of decortication or decerebrate posture, arterial hypertension (BP system. more than 160 mm Hg), profuse sweating, hyper- (>38 ° C) or hypothermia.
Does an MRI show a concussion?
Since a concussion is usually not accompanied by morphological disorders, conducting research is most important in order to exclude the development of complications. It is worth conducting an MRI in case of a concussion first of all to exclude a dangerous pathology - brain contusion. Doctors recommend resorting to this technique in case of danger of intracranial hemorrhages, severe traumatic brain injuries and ischemic conditions. Due to the fact that the magnetic resonance imaging technique is extremely informative, it is always useful to conduct an MRI if the patient has hit his head.
The examination will take about 15 minutes, during which the patient remains under the influence of the electromagnetic field of the tomograph - it is completely safe and painless. At this time, the doctor receives three-dimensional images of the skull bones and brain tissue.
The feasibility of MRI for head injuries has been confirmed by leading world research and is explained by the information content of this modern diagnostic method.
CT signs of brain contusion
What can be seen on a CT scan in case of a brain contusion? On computed tomograms, the focus of the bruise (contusion) looks like alternating hyperdense areas (hematomas) and hypodense areas (detritus). Concussion foci are formed both on the side of the impact (application of force) and on the side of the counter-impact. Perifocal ischemia from compression of blood vessels by a hematoma increases the area of pathologically altered tissues and causes the severity of brain dislocations.
The existing classification of brain contusions according to Kornienko, which is not universally accepted, provides for four types of lesions: contusions of the first type look like homogeneous hypodense areas and are very similar in appearance to cerebral infarction. Bruises of the second type look “motley” due to multiple small hematomas located in the detritus area. Contusions of the third type are large multiple hematomas against the background of detritus, and contusions of the fourth type are actually parenchymal hematomas.
The most common foci of contusion, such as intracerebral hematoma, evolve as follows: in the period of 1-3 days, a hypodense zone appears around the hematoma, caused by perifocal cerebral edema, then, in a period of several weeks to a month, lysis of the hematoma and resorption of blood occurs, the opposite of the development of ischemic changes. The result may be the formation of a cyst or glial scar.
Signs of brain contusion on CT scan. The focus of brain contusion is similar to a parenchymal hematoma, surrounded by a zone of perifocal edema. On the opposite side, you can also see a focus of contusion and an area of subarachnoid hemorrhage.
results
Taking into account the time of onset and duration of the course of individual symptoms and phenomena in general, the clinical picture after a long coma had certain patterns of progression. Immediately after an episode of prolonged coma, patients were found to have stabilization of vital functions, restoration of brainstem reflexes, and episodes of spontaneous opening of the eyes without signs of consciousness or emotional reactions. The clinical picture of the disease corresponded to the generally accepted criteria for VS. 64 (73.6%) patients were diagnosed with signs of dysautonomia.
The phenomenon of spontaneous opening of the eyes without signs of consciousness is the result of restoration of the function of the reticular formation of the brain stem. The stabilization of vital functions and the revival of previously suppressed brainstem reflexes, detected in patients after a long coma, are a consequence of the restoration of the activity of the centers for the regulation of vital functions and the nuclei of the cranial nerves located in the brainstem. Thus, the clinical signs detected in patients immediately after an episode of prolonged coma reflect the restoration of the functions of the brain stem regions.
In 13 (14.9%) patients, recovery of vital functions was incomplete, which was manifested by episodes of arterial hypotension and/or repeated disturbances in external respiration. In 65 (81.3%) patients, asymmetry of the brainstem and/or incomplete restoration of the protective blink and/or indicative sound reflexes were detected.
In 19 (21.8%) patients, restoration of brain function was completed at the level of brain stem function.
68 (78.2%) of those examined, following the stage of reintegration of the function of the brain stem, noted the following changes in the clinical picture: complete or partial regression of signs of dysautonomia, clinically manifested by complete or partial stabilization of autonomic functions; the appearance of such primitive (unconscious) emotional reactions as a grimace of pain to a painful stimulus (discomfort) and/or mimicry.
Various elements of sensation (pain, discomfort, well-being) are realized in the thalamus, acquiring a connection with a specific feeling. The cerebral center for regulating the autonomic functions of the body is the hypothalamus. Therefore, we regarded the appearance of unconscious emotional reactions in patients and the stabilization of autonomic functions as clinical manifestations of restoration of the functions of the thalamic and hypothalamic structures of the brain; and the stage following the restoration of the functions of the brainstem was called the stage of restoration of the functions of the diencephalon. The clinical picture of the disease in patients at this stage of recovery corresponded to the criteria of a vegetative state, since no conscious reactions were detected in patients.
At this stage, 27 (39.7%) patients had a short-term reflex fixation of the gaze on a moving object. In 56 (82.4%) patients there was a reaction to external stimuli in the form of a general increase in muscle tone. In 11 (16.2%) of the examined, defensive reactions were manifested by mild, non-purposeful movements in the limbs, the stereotypes of which changed even during the day.
In 26 (29.9%) patients, restoration of brain functions was completed at the stage of restoration of diencephalon functions.
In 42 (48.3%) patients, signs of consciousness were revealed over time. Its first manifestations were episodes of clear, repeated fixations of gaze on surrounding objects and differentiated vegetative-emotional reactions to loved ones and relatives. 26 of these victims required constant care due to low consciousness and/or severe disturbances in movement and muscle tone. In 16 patients, restoration of a higher level of functioning was noted.
Considering the obligatory participation of telencephalon structures in the implementation of conscious reactions, this period was called the stage of restoration of telencephalon functions.
The main clinical and neurological characteristics of the various stages of restoration of brain function in patients after a long post-traumatic coma are presented in Table. 1.
Table 1. Neurological characteristics of the stages of restoration of brain functions in patients after prolonged post-traumatic coma
Table of contents
- In what cases is a CT scan prescribed, and in which MRI?
- Contraindications
- Advantages of each type of tomography
- Technical specifications
- Advantages of carrying out the procedure at MEDSI
Computed tomography
is a type of study in which a layer-by-layer scan of the patient’s organ is performed. A multislice computed tomograph is used to carry out the procedure. The principle of its operation is based on the reflection of X-ray radiation from tissues and bones. The result of the study is presented as a 3D image on the doctor’s monitor and can be recorded on disk.
The CT machine is a circle around a table with movable sensors, which, rotating during the examination, take pictures from different angles.
Since using this method the patient receives a certain dose of radiation, the study is not recommended to be done frequently.
Magnetic resonance imaging
is an examination based on the effect of magnetic resonance, which is reflected differently from more or less dense tissues.
A tomograph is also used for this, but of a different, often closed type. It is equipped with a retractable table on which the patient is placed, and a tube-shaped apparatus into which this table is pushed.
This is a fairly safe examination method, although there are a number of limitations in its use, mainly related to the presence of metal implants in the body.
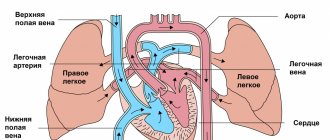
Venous and arterial aneurysms on MRI scans
Aneurysmal dilations of blood vessels have a special morphology - neck, body, dome. The cause of the disease is deposits of fatty complexes inside the vascular wall. The disease is called atherosclerosis and causes many complications in the brain and heart. Damage to the wall leads to disruption of permeability. Blood entering the interstitium causes dissection. Clots and formed elements accumulate between the individual layers. The movement of blood creates pressure on the thin wall. At a certain point, the vessel may not hold up. The appearance of a small rupture is accompanied by hemorrhage. Massive bleeding leads to death.
Contrast MRI for brain aneurysm is the best option for diagnosing the pathology. Tomograms reflect the full morphology - saccular, fusiform expansion of the arterial wall. Even a native MRI scan can reliably verify an aneurysm. Contrast improves visualization.
Tomograms show the size of the aneurysm. Formation over 10 mm is dangerous due to rupture.
Practical features of MRI of aneurysm after trauma:
- The spatial structure and relationships of individual parts are revealed by MR angiography. A bolus injection of contrast agent creates a clear image of the arteries and veins;
- Thrombosed and non-thrombosed aneurysmal dilatation is identified by taking multiple sections. The 3D modeling mode allows you to build a spatial projection of an object. The procedure helps determine the shape and size of the aneurysm;
- A combined study (CT and MRI) after head injuries allows you to diagnose thrombosed areas of the artery, measure the length of the neck, and verify the dimensions.
After severe trauma, angiography is performed to study the spatial relationships between various physiological and pathological formations. Magnetic resonance neuroimaging is performed to verify rupture, thrombosis, and aneurysmal dilatation of the artery. The study additionally reveals a whole list of pathologies.
Spasmodic contractions of arteries and veins of individual brain segments are diagnosed using a combination of methods - MR angiography, CT angiography, catheterization angiography. On the recommendation of a radiology doctor, additional examinations (MR spectroscopy, tractography) may be prescribed.