Concussion in children - symptoms and treatment
When diagnosing SHM, it is necessary to take into account the nature of the injury and interviewing witnesses to the incident. In some cases, traces of trauma on the head and the psychological state of the child may indicate a concussion.
Since the signs of a concussion in a child are not very clear, changes in symptoms over time are important in diagnosis. Their disappearance after 3-7 days is a good reason to suspect SMG.
The difference between SHM and bruise and other forms of traumatic pathology:
- no skull fractures;
- the pressure and composition of the cerebrospinal fluid are unchanged;
- M-echo without offsets;
- CT and MRI without traumatic abnormalities in the parenchyma of the brain and in the cerebrospinal fluid-containing intracranial spaces.
To determine the severity of TBI, the following is assessed:
- duration of loss of consciousness in the acute phase of the injury (if it occurred);
- duration of post-traumatic amnesia (if present) and assessment of vital functions;
- degree of depression of consciousness at the time of examination (Children's Glasgow Coma Scale).
Electroencephalography and ophthalmoscopy can indirectly contribute to the objectification of concussion in the acute phase of TBI. Neurosonography (ultrasound of the brain) has become widespread in the diagnosis of TBI in children .
Ultrasound of the brain is performed on children from the first day of life until the period of closure of the large fontanelle, which is an acoustic window through which the state of all brain structures can be visualized. The study evaluates the cerebrospinal fluid system (lateral ventricles, choroid plexuses, III and IV ventricles, occipital cistern), thalamus, cerebellum, brain parenchyma, cerebral blood flow, the presence of free fluid between the brain parenchyma and the skull, as well as the skull bones.
This study allows us to exclude changes in the brain after injury - swelling of the parenchyma, displacement of the midline structures, fractures of the skull bones, areas of brain contusion and intracranial hemorrhage.[5][13]
Ultrasound signs of brain injury that exclude BMS:
- with edema of the brain parenchyma - a decrease in the echogenicity of the brain parenchyma in the first hours after injury, its increase in dynamics and normalization on days 6-7.
- in case of brain contusions - the presence of hyperechoic inclusions in the brain parenchyma against the background of a general decrease in the echogenicity of parenchyma tissue (intracranial hematomas have a higher echogenicity).
- for severe brain contusions:
- areas of the brain parenchyma of an isoechoic nature, visible only due to their additional volume;
- areas of additional volume with a moderate increase in echogenicity and an unclear contour;
- areas of additional volume with a clearly demarcated contour and an intense increase in echogenicity.
- areas of additional volume with a sharp increase in echogenicity.
- with epidural hematomas - a clearly demarcated spindle-shaped area adjacent to the skull bone, with increased or slightly decreased echogenicity, displacing the structures of the brain;
- for subdural hematomas:
- local changes in density boundaries (usually spindle-shaped), covering the entire hemisphere;
- chronic subdural hematomas with reduced echogenicity;
- for intracerebral hematomas:
- hyperechogenicity stage - lasts up to 8-10 days;
- anisoechoic stage - characterized by the appearance in the center of the lesion of zones of reduced echogenicity with an increase in size over time (10-30 days after injury);
- anechoic stage - only indirect signs of a volumetric process are visualized (1-2 months);
- the stage of subsequent residual changes with the formation of cysts or areas of brain atrophy.
- with intraventricular hemorrhages caused by trauma - the presence of an intraventricular hyperechoic zone, expansion of the lumen of the lateral ventricles and changes in the shape of the choroid plexus (rare, usually occur in the presence of multiple hematomas).[5]
Neurosonography also makes it possible to identify rare variants of the location of hematomas - the posterior cranial fossa, the pole of the frontal lobe with displacement of the echo structures of the brain and the “plus tissue” effect, the presence of free fluid along the anterior surface of the brain parenchyma. If the hematoma is located in the posterior fossa of the skull, signs of hydrocephalus are observed - expansion of the lateral ventricles of the brain and the third ventricle of the brain.[5]
Head injury in a child
The child grows and strives to explore the world. Childhood is the most dangerous period for a child. It is not uncommon for children to suffer head injuries.
A head injury is damage to the head or skull. Traumatic brain injury ranks first in terms of incidence. It accounts for 30–40% of the total number of patient visits. It is necessary to detect TBI in a timely manner, since the injury can cause irreparable harm to the child’s health.
Types of TBI in a child
1. Closed or open injury.
When injured, the integrity of the soft tissues of the head is compromised. There may be damage to bones, a fracture of the base of the skull. 2. According to severity, they are distinguished:
- Mild degree. The damage is not accompanied by complications and often goes away without medical care. Characterized by irritability, sleep disturbances, headaches and dizziness for a short period of time.
- Moderate - severe contusion affecting the brain, such as a skull fracture. Damage can seriously affect your health. Doctors note mental disorders, memory loss, abnormal heart rhythm, paroxysms of the upper and lower extremities, and disturbances in the functioning of the visual apparatus. Recovery takes several months
- Severe degree. It is characterized by serious consequences that affect the quality of life of the victim. There is a possibility of death and coma. It is characterized by loss of sensitivity, deterioration of hearing and vision acuity, disruption of the cardiac system, memory loss, and epileptic seizures.
3. For brain damage:
- shake;
- injury;
- diffuse axonal damage;
- squeezing.
Causes of head injury in children
Injuries to the skull and brain often occur due to reasons unrelated to health:
- a fall;
- road accident;
- blow to the head.
Each age has different reasons. A one-year-old child is just starting to walk, and this is not at all easy. He constantly falls, but persistently goes towards his goal. Parents need to be especially careful and prevent head injuries. At an older age, children begin to go to kindergartens and schools. During this period, blows to the head during the game are possible. There may also be road accidents, which is especially dangerous for a child.
Symptoms of TBI
Based on symptoms, children can be divided into two groups:
- up to two years, when the child cannot yet speak coherently;
- after three, when the child can explain something.
The first group is characterized by the following symptoms:
- cry;
- lethargy;
- drowsiness;
- lack of response;
- temperature increase;
- regurgitation.
For the second group:
- headache;
- dizziness;
- memory losses;
- nausea;
- incoherent speech;
- swallowing disorder;
- temperature increase.
First aid for traumatic brain injury
You need to call an ambulance.
The health of your child depends on the speed of contacting a specialist. If you arrive late at the hospital, complications may arise. Before the ambulance arrives, you can do:
- apply cold to the head;
- transfer the child to a lying position;
- unbutton clothes so that the child can breathe more freely;
Diagnostics
If a child has a head injury, tests are prescribed depending on the nature of the injury.
- EEG. Brain dysfunctions are determined.
- X-ray. The integrity of the skull is revealed.
- CT scan. With its help, the state of the brain is determined.
- Magnetic resonance imaging. Detects brain contusions.
- Ultrasound. Relevant for children under one year old.
General clinical picture of childhood TBI
Key points in the development of pathology:
- Lesions of the cranial plexuses of nerves.
- Confusion of consciousness.
- Focal symptoms.
When damage occurs in any childhood, there is an almost complete absence of any symptoms, even a couple of hours after the injury. This significantly complicates diagnosis and, consequently, assistance to victims.
TBI in children also has its own symptoms that are rarely found in adults. This is due to age-related characteristics - immaturity of brain tissue, incomplete ossification of the cranial bones.
The injured child cannot adequately respond to the survey; it is difficult for him to describe the causes and circumstances of the traumatic injury. In young children, loss of consciousness occurs in almost 90% of cases. In some episodes, increased sensitivity to stimuli (sound, light) may be observed. Neurological symptoms develop incredibly quickly, with general cerebral symptoms (i.e., vomiting, headache) predominant. Moreover, young children often develop hemorrhages, and subsequently cerebral edema, leading to serious complications.
With a mild TBI (concussion), the child’s consciousness does not change.
There are gradations of pathological states of consciousness:
- Clear – the child is active, oriented in time and space, and able to answer questions well.
- Stupor (stunning) - the baby is not fully oriented, drowsy, makes contact with difficulty, answers questions reluctantly, monosyllabically, and is able to follow commands.
- Stupor - consciousness is impaired, the child is unconscious. The defense reaction occurs to a painful stimulus. Pronounced flexion movements predominate in the limbs.
- Coma - the patient is not conscious, does not respond to shouts or other irritations, pain reactions are not expressed, and there are no defensive movements. Disorders of muscle activity are rapidly developing. The respiratory function is sharply depressed, the heart works intermittently. Extension movements of the arms and legs predominate, but they are rare.
- Deep coma - severe disturbances of consciousness. There are no reactions to painful stimuli. The pulse increases and exceeds 140 beats per minute, blood pressure drops rapidly. There is no spontaneous breathing. This condition can easily be fatal even with adequate medical care.
Memory disorder can be either retrograde (loss of memories of events that occurred before the injury) or anterograde (the baby does not remember what happened after the injury itself). Subsequently, with proper rehabilitation of the child, the gaps in memory are successfully filled.
Head pain appears in 100% of cases. It worries all children without exception who have suffered a TBI of varying degrees of severity. Moreover, the characteristics of the pain are as follows: it is diffuse, subsides with complete rest and subject to bed rest.
Vomiting is also the most common symptom belonging to the group of general cerebral manifestations of TBI due to irritation of the nerve nuclei in the brain structure. With minor injuries, vomiting appears along with dizziness and pain. When a child has an extremely serious condition, uncontrollable vomiting may develop, which does not bring the desired relief and exhausts the patient.
When examining a child, you should definitely pay attention to the pupillary reaction to light and other stimuli. In mild TBI, impairments occur that manifest as weak reflexes to light stimuli (i.e., the pupil slowly constricts). In comatose states, there is often a complete lack of reaction to light.
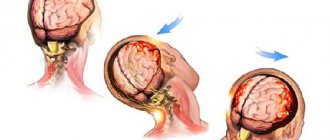
Detection of a dilated one pupil (provided that the second one is of normal size) is an ominous sign of developing complications of injury - dislocation (displacement) of the brain into the foramen magnum and compression of the nerve pathways.
Muscle tone is variable and may be increased. Some children exhibit reflex disturbances, seizures, or, conversely, a complete lack of movement and weakness of the muscular system.
The heart rate with mild TBI is within acceptable values; with more severe injuries, the pulse increases or decreases significantly (in coma). Body temperature remains virtually unchanged. In young children it may increase slightly. If the temperature reaches 40 - 41 C, one should suspect intracranial hemorrhages and the rapid development of extracranial complications.
The listed symptoms are characterized by extreme variability and can be observed in a child in different combinations.
Injury
A bruise is a severe injury that develops due to any deformation of the brain substance. Lesions - single or multiple - are classified according to the depth of damage to the cortex and location.
A mild degree is extremely difficult to differentiate from a concussion, and therefore a number of doctors consider these two pathologies to be synonymous. There is a lesion in the brain that does not penetrate into the deep layers of the cortex.
With a moderate injury, the lesions spread over a large surface, but the membrane of the brain is not damaged.
But in severe cases, the bruise is characterized by multiple foci or one, but occupying a significant surface of the cortex. The soft membrane of the brain is destroyed. Serious complications often develop, as dislocation of the brain occurs, as well as deformation of the trunk.
In the area of hemorrhage, microcirculation is disrupted, which leads to the appearance of a characteristic clinical picture. With multiple injuries, the patient's condition will be extremely serious, in some cases incompatible with life. Tissue hypoxia and cerebral edema develop, the functions of organs and systems are disrupted. With TBI in children, focal symptoms are observed: paresis and paralysis, disturbances in the innervation of the facial nerves, disconnection of reflexes, pronounced pathological changes in breathing and heart function. But it is worth noting that with the development of motor activity disorders, there is a high chance of restoration of function, provided that the necessary therapy and surgical treatment are carried out.
General cerebral signs of injury manifest themselves in the form of pain in the head, repeated vomiting, impaired consciousness and dizziness. However, the symptoms are more pronounced than with a concussion. Loss of consciousness in a child occurs suddenly and for a longer period. When waking up, the baby is also inhibited, unable to adequately talk and assess his condition, or is whiny and capricious (in infants). Vomiting is repeated, indomitable, does not bring the expected relief and occurs even with a sharp turn of the head. Pain in the head accompanies almost the entire duration of the disease and is pronounced.
With brain contusions and rupture of the membranes, bleeding appears. Moreover, the more pronounced they are, the deeper the damage to brain structures and the greater the number of lesions. An increased number of red blood cells is always detected in the cerebrospinal fluid. Blood entering the cerebrospinal fluid leads to additional irritation of the membranes of the brain. All this entails the development of such a syndrome as meningeal. But in some groups of children (mainly primary school age), manifestations of meningism may be completely absent.
The severity criteria for bruises are: severe depression of consciousness, temperature rise above 40 C, increase in the number of heartbeats, rapid breathing, increased blood pressure. In the body, in response to pathological processes, the processes of catabolism (destruction of proteins) become leading. That is why an increase in the level of glucose and nitrogen metabolism products is found in the blood.
When TBI foci in children are localized in the brain stem, the clinical picture is characterized by a decrease in heart rate and respiratory rate, blood pressure rapidly decreases, and temperature drops even below normal values.
Recently, a new type of damage has been highlighted - diffuse axonal. It occurs during an accident during sudden braking of a body moving forward. In this case, microtraumas of the brain stem and nerve bundles occur, as well as microhemorrhages in the nuclei of the brain. Patients experience an extremely serious condition, coma, which in most cases leads to death. The difficulty of diagnosis lies in the fact that such pathology is extremely difficult to notice on MRI and CT. Therefore, the diagnosis is most often made on the basis of pathological autopsy data.