Find out more about diseases starting with the letter “K”: Causalgia, Brain cyst, Cluster headache, Tick-borne encephalitis, Kozhevnikov epilepsy, Colloid cyst of the third ventricle, Coma, Compressive myelopathy, Balo concentric sclerosis, Radicular syndrome, Corticobasal degeneration, Craniovertebral anomalies, Craniospinal tumor, Craniopharyngioma, Myasthenia gravis crises, Hemorrhage into the ventricles of the brain.
Depending on the location of the formation, focal symptoms may be present. The diagnosis is made based on data from computed tomography and magnetic resonance imaging of the head or neurosonography (in children). Therapy consists of aspiration and surgical removal of the formation if complications develop or its growth progresses.
General information about pathology
A cyst is a fluid-filled cavity located in the substance of the brain or its membranes. When the pathology is small in size, it has a subclinical course and is diagnosed accidentally during a neuroimaging examination of the head. Since the intracranial space has limited dimensions, with a significant increase in the volume of the formation, intracranial hypertension develops.
The size of the cavity with liquid is largely determined by the compensatory capabilities of the formation and its localization. Due to the pliability of the skull bones in children at an early age, the cyst may not manifest itself for a long time.
The formation can be found in people of different ages, both in infants and in elderly patients. Even if the fluid cavity is congenital, it can make itself felt only by the age of 30-50.
According to generally accepted practice, treatment is prescribed only in the case of a pronounced clinical picture and when complications develop. If the cavity with fluid is frozen or slowly progressing and its volumes are insignificant, a wait-and-see approach is chosen, which involves regular monitoring of the patient.
3. Symptoms of a brain cyst
Small cysts are asymptomatic and can be accidentally detected during examination. When the tumor reaches a large size, the symptoms that appear depend on its location. Among the most characteristic symptoms are:
- headache, dizziness;
- feeling of fullness in the head;
- auditory and visual impairments;
- convulsions, paralysis of limbs;
- epileptic seizures;
- impaired coordination of movements;
- fainting, hallucinations;
- sleep disorders.
About our clinic Chistye Prudy metro station Medintercom page!
Classification
Classification by location:
- Cerebral (intracerebral). It is formed in areas of dead brain tissue in the internal structures of the brain.
- Arachnoid. It is formed as a result of the accumulation of cerebrospinal fluid in places of adhesions formed as a result of inflammatory processes and in places of their congenital duplication. The advantage is localized in the meninges.
The following types of brain cysts are distinguished separately:
- dermoid;
- colloidal;
- choroid plexus;
- pineal gland.
According to its genesis, a cavity with fluid can be congenital or acquired. In turn, congenital is divided into colloid and dermoid, and due to its formation into post-infectious, post-traumatic, post-stroke and echinococcal.
How to get treatment:
- Make an appointment. By phone (89031830141), make an appointment from the website, by E-mail.
- Consultation. In person or remotely (E-mail, WhatsApp, Viber).
- Examination. Ultrasound of the kidneys and bladder. For proximal hypospadias or in combination with cryptorchidism - endocrinological examination.
- Hospitalization and collection of tests. Collection of necessary tests and preparation for surgery.
- Surgical treatment. Microsurgical reconstructive plastic surgery.
- Extract. Recommendations in the postoperative period.
Etiology and pathogenesis
The causes of a congenital cyst are unfavorable factors that occur during the development of the fetus. These are:
- fetal hypoxia during delivery;
- fetoplacental insufficiency;
- taking a specific group of medications by a pregnant woman;
- Rh conflict between mother and child;
- intrauterine infections.
Factors that provoke the development of a congenital cavity with fluid are drug, alcohol or nicotine addiction of the mother. In this case, the child’s development takes place under conditions of intrauterine intoxication, which negatively affects the brain structures. The causes of the cavity can also be chronic decompensated diseases of the expectant mother.
An acquired cavity with fluid in the head develops as a result of:
- inflammatory diseases (encephalitis, brain abscess, arachnoiditis, meningitis);
- traumatic brain injuries;
- injuries of newborns received during childbirth;
- cerebrovascular accidents (subarachnoid hemorrhage, ischemic stroke, hemorrhagic stroke).
Depending on the etiology, the following types of liquid cavities are distinguished:
- A cyst of iatrogenic origin forms as a complication after brain surgery.
- Parasitic - develops with paragonimiasis, cerebral form of taeniasis and echinococcosis.
A cavity with fluid can also replace cerebral tissue during degenerative and dystrophic processes in the head.
If a cyst is present, there are a number of factors that can trigger its growth. These include obstruction of venous outflow from the skull, strokes and other vascular disorders, as well as head injuries, hydrocephalus, and neuroinfections.
Examination and diagnosis
MRI or CT will provide unambiguous information about the presence, size and location of the cyst. A study with intravenous contrast helps to distinguish a cyst from a tumor You can perform such a study at the Clinic of the Academy of Sciences .
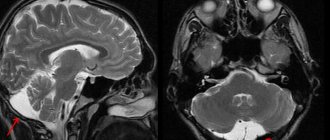
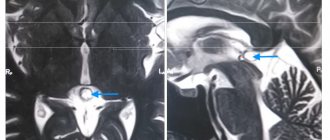
MRI scans of the brain. 1. Cyst after cerebral hemorrhage 2. Cerebellar cysts after ischemic stroke (blockage of cerebral arteries) 3. Cystic adhesive arachnoiditis
To avoid the enlargement and appearance of new cysts , we must clearly understand and treat the root cause of their occurrence. Therefore, we carefully examine you for circulatory disorders, infections, and autoimmune diseases.
Doppler ultrasound of the head and neck vessels (USDG) will help detect narrowing of the vessels that supply the brain with arterial blood. Lack of blood supply can lead to focal death of the brain matter and the appearance of cysts.
Heart studies (ECG, Echo-CG) . The brain may not have enough blood supply due to rhythm disturbances or heart failure.
Blood test for clotting and cholesterol. An increase in cholesterol concentration in the blood and increased clotting are the main causes of blockage of brain vessels with subsequent formation of cysts. This problem is easily solved with the help of modern medications.
Blood pressure monitoring. Episodic increases in pressure are a common cause of strokes and post-stroke cysts. A monitor is a small device that is constantly with you for 1 day and records your blood pressure on a memory card. The data is then read by a computer and gives the doctor a complete picture of the pressure for the day.
blood tests for infections and autoimmune diseases of the nervous system in cases of suspected neuroinfections, arachnoiditis, and multiple sclerosis.
Brain cyst
The growth of the formation at the initial stage is in most cases accompanied by symptoms of intracranial hypertension. Patients constantly complain of nausea, which has nothing to do with food, deterioration in general health and decreased performance, constant cephalalgia and pressure on the eyeballs.
In some cases, the main symptoms include a constant feeling of pulsation in the head, sleep disturbance, mild hearing loss, dizziness, motor dysfunction, fainting and tremors of the limbs. Possible visual impairment, namely double vision, visual hallucinations, deterioration of visual acuity. With high intracranial hypertension, the patient is worried about constant vomiting.
There are cases when the first signs indicating a cavity with fluid are the first occurrence of epileptic paroxysm. Subsequently, epileptic seizures recur. Paroxysms can take the form of focal Jacksonian epilepsy or absence seizures and be of a primary generalized nature.
Compared to general cerebral manifestations, focal symptoms are observed in fewer cases. These may be sensory disorders, monoparesis and hemiparesis, brainstem symptoms. The latter include dysarthria, eye movement disorders, and swallowing disorders.
One of the complications of formation is cyst rupture. In this case, hemorrhage due to rupture of the vessel, compression of the brain, the formation of an epileptogenic focus and occlusive hydrocephalus are possible.
In the congenital form of the cyst, episyndromes and intracranial hypertension are recorded at an early age. Education in the brain can cause the child to develop mental retardation and mental development disorders.
Symptoms of arachnoid cystic formations
Most often, the cyst is insignificant in volume and does not show clinical signs. Congenital pathology can be discovered completely by accident during diagnostic procedures (MRI, neurosonography) for other intracranial abnormalities. Initial symptoms may appear due to disorders of the blood vessels of the brain, trauma or infections.
The growing cerebrospinal fluid provokes an increase in the size of the cyst, and the symptoms become pronounced:
- increased pressure inside the skull;
- cephalalgia (headache);
- feeling of a “heavy” head (dizziness, noise and pounding (pulsation) in the ears and skull).
The growing volume of cystic formation provokes an increase in the intensity of permanent symptoms:
- nausea and vomiting;
- increased fundus pressure;
- bifurcation and spots of visual fields;
- hemiparesis (muscle weakness);
- dysarthia;
- numbness of the arms and/or legs;
- convulsions;
- fainting.
Sometimes the patient experiences hallucinations. Children experience mental retardation (mental retardation).
The consequence of a growing arachnoid cyst can be brain degeneration, rupture of the formation, and death.
Types of brain cysts and their symptoms
Arachnoid - occurs in almost 4% of the population. A cavity with fluid can be congenital or acquired. In the latter case, it develops in response to traumatic brain injury. The formation is localized on the surface of the brain in its membranes. The cavity is filled with cerebrospinal fluid.
In most cases, an arachnoid cyst does not make itself felt for quite a long time and is discovered by chance. Severe symptoms appear only if a large amount of fluid accumulates in the cavity. In this case, cerebrospinal fluid is produced by the cells lining the cavity.
With a sharp increase in the volume of the cavity with liquid, it can rupture and, as a result, die.
Colloid cysts are recorded in 15-20% of all cases of formations inside the ventricles of the brain. Most often it is localized above the foramen of Monroe in the anterior region of the 3rd ventricle. Less common in the area of the transparent cerebral septum in the 4th ventricle.
The liquid filling the cavity of the colloid cyst has high viscosity. Patients experience symptoms of hydrocephalus and, with a certain position of the head, a paroxysmal increase in cephalgia is noted.
In rare cases, memory loss, behavioral disorders and weakness in the limbs occur.
Pineal cyst of the pineal gland - according to statistics, 10% of patients have formations of this type that are small in size and do not make themselves felt. Cystic formations are localized in the epiphysis of the brain, in most cases they are no more than 1 cm in size. Otherwise, symptoms appear. When it grows, it can block the entrance to the “plumbing” of the brain and block the circulation of cerebrospinal fluid, causing occlusive hydrocephalus.
Epidermoid or dermoid is a formation that is an anomaly of intrauterine development. In this case, the cells of the baby's future skin and its appendages remain inside the brain. Accordingly, in addition to liquid, elements of the ectoderm are present, namely sebaceous glands and hair follicles.
After the birth of a child, such a cyst quickly increases in size. The only possible treatment is surgical removal of the formation.
Choroid plexus cyst - forms regardless of the person’s age. In this case, the space between the plexus vessels is filled with cerebrospinal fluid. Symptoms are rarely present, sometimes accompanied by epileptic seizures and symptoms of intracranial hypertension.
With a congenital choroid plexus cyst, the formation is diagnosed at the 20th week of intrauterine development using ultrasound. By the 28th week, such formations resolve.
What is an ovarian cyst
Cysts in the ovaries often occur in women against the background of a seemingly normal cycle. Since it is in the testicles that the follicle is formed, from which the egg is formed, which ruptures the follicular membrane and is released into the uterine cavity during ovulation, cysts are formed here. This happens when the follicle, while maturing, does not rupture. As a result, it fills with liquid. The second type of cyst is a cystic formation of the corpus luteum. This occurs when the egg has left the follicular membrane, but the corpus luteum has filled with fluid.
The reasons for the formation of cysts in the ovaries can be:
- changes in body weight due to hormonal fluctuations or unhealthy eating behavior;
- constant stress;
- excessive physical activity.
Cysts of this kind do not require medical intervention and go away on their own with a cycle. Prescribing hormonal therapy in this case is also not justified, since changes in hormonal levels can negatively affect subsequent cycles and ovulation.
If a functional ovarian cyst is detected, it is necessary to abstain from sexual activity and not lift any heavy objects, so as not to provoke a rupture. In addition, you should not engage in sports, especially if it is running or acrobatics.
Surgical intervention is justified only if the cyst does not go away on its own within 5-6 months, as well as in the case of its internal rupture and release of fluid into the uterine cavity.
Diagnostic measures
A neurologist may suspect the presence of an intracranial formation of significant size based on the patient’s neurological status and clinical symptoms. In this case, the patient is sent for examination to an ophthalmologist and otolaryngologist to check vision and hearing. Specialists perform ophthalmoscopy, audiometry, perimetry and visometry. With severe hydrocephalus, ophthalmoscopy reveals congested optic discs.
By referring the patient for echo-encephalography, it is possible to diagnose increased intracranial pressure. If the patient experiences epileptic paroxysms, he is additionally sent for electroencephalography.
It is extremely important to differentiate a cavity with fluid from a tumor, abscess and hematoma. It is not possible to do this on the basis of collected clinical data alone. Therefore, to make a clear diagnosis, neurologists use neuroimaging diagnostic methods.
By performing an ultrasound examination, it is possible to diagnose certain types of congenital cysts even at the stage of intrauterine development of the fetus. After birth, until the baby's large fontanelle closes, neurosonography is performed to make the correct diagnosis. In adulthood, to visualize a brain cyst, the patient is sent to a magnetic resonance or computed tomography scan of the head.
MRI and CT are performed with contrast in order to differentiate a cyst from a tumor. A cavity with liquid is not able to accumulate a contrast agent, unlike a tumor.
After diagnosis, constant monitoring of the patient with a cystic formation is important. During regular examinations, the doctor monitors the volume of the cyst over time.
If the cyst is a consequence of a stroke, additional vascular examinations are carried out: ultrasound, MRI and CT of vessels, duplex scanning.
Causes of cysts
Congenital formations can be a consequence of an unfavorable pregnancy, complicated by fetal hypoxia, taking teratogenic drugs, Rh conflict and other factors that have a negative impact on the fetus. This also includes the intoxicating effects of drugs, alcohol, and nicotine.
An acquired brain cyst is primarily the result of degenerative processes against the background of:
- TBI;
- abscesses;
- acute brain disorders;
- parasitic infection, etc.
Cyst-forming complications are possible after intracranial surgery. Sometimes an existing cyst is provoked to growth by cranial injuries, infections, inflammations, vascular pathologies, and hydrocephalus.
General principles of therapy
Drug therapy for cystic formations has practically no results. The only possible treatment is surgical removal of the fluid cavity. But, most forms are small in size and remain in a “dormant” state for many years. In this case, no methods of therapy are used; a wait-and-see regimen is chosen and the patient is regularly examined.
Formations that are accompanied by symptoms of hydrocephalus, complicated by bleeding and rupture, compressing the brain and rapidly increasing in size must be removed. Only a neurosurgeon decides which method of surgical treatment to use.
If the patient has a disorder of consciousness (coma or stupor), he is urgently referred to external ventricular drainage. This method allows you to reduce compression of the brain by the cyst and intracranial pressure. If the cyst ruptures or hemorrhages, surgery is performed. The patient undergoes craniotomy and the formation is excised.
In the absence of complications and disturbances of consciousness, the operation is performed planned and endoscopically. The advantage is the patient’s quick recovery period and low trauma. With endoscopic access, a milling hole is made in the skull, through which fluid is sucked out from the cavity. In order to avoid subsequent accumulation of fluid, several holes are made in the cavity (connected to the cerebrospinal fluid space) or cystoperiotoneal shunting is performed (a special shunt is installed).
The postoperative period involves rehabilitation therapy, including exercise therapy, reflexology and massage. The patient is prescribed drugs to improve blood supply to the brain, absorbents and decongestants.
Healing procedures
Conservative methods of treating brain cysts are not effective. A positive result is achieved quickly. However, active therapy is not required if the formation is small and does not increase over time. The patient is under observation with regular instrumental diagnostics to monitor the condition.
Neurosurgical intervention is required if the cyst:
- manifested by signs of hydrocephalus;
- actively growing;
- compresses the tissues inside the skull;
- complicated by hemorrhages or ruptures.
The method of performing the operation is determined by the neurosurgeon based on the patient’s condition: endoscopy, trepanation, external ventricular drainage. Drug treatment is included at the rehabilitation stage. The recovery complex includes exercise therapy, physiotherapy, massage, etc.
Forecasts
In most cases, a frozen cavity with liquid of insignificant size does not bother the patient and does not cause any symptoms. In other cases, with adequate and timely treatment, the outcome is favorable.
In rare cases, patients after surgical removal of a cyst experience a residual moderate-to-severe liquor-hypertensive symptom. If a focal neurological deficit develops, it persists after treatment.
With the removal of the cyst, epileptic paroxysms disappear, but often appear later. This is justified by changes in the operated area of the head, in particular the formed adhesions. Secondary epilepsy is practically uncontrollable by anticonvulsant therapy.
4.Basic treatment methods
As a rule, cysts that do not show a tendency to grow do not require treatment at all. Otherwise, treatment of neoplasms is carried out surgically. It could be:
- transcranial surgery, which provides high efficiency of cystectomy, but is traumatic for the patient;
- shunting the cyst to evacuate the liquid contents, after which its walls collapse;
- gentle endoscopic surgery using special equipment.
Prevention
An acquired cyst most often becomes a consequence of developing inflammatory, vascular, infectious and post-traumatic processes. Therefore, it is absolutely obvious that only correct and timely treatment of any pathologies, including resorption and neuroprotective therapy, can serve as a preventive measure for the development of formations in the brain.
The only measure to prevent congenital cysts is to protect the woman and fetus from exposure to provoking factors. Equally important are correct management of pregnancy and delivery.
Localization
The development of a dermoid cyst is possible in almost any organ or tissue, as doctors note. Most often the presence of cysts is found in:
- the ovarian area in women of reproductive age, which can seriously affect the ability of the fair sex to conceive;
- the lower eyelid area (mostly children are affected, but the pathological neoplasm can be easily removed with the help of surgeons);
- the coccyx area, where the size of the ovarian dermoid cyst rarely reaches large sizes, and the formation can go unnoticed for a long time;
- the area of the anus, where without symptoms of inflammation, pathology is generally detected only by digital rectal examination, etc.
The discovery of dermoid cysts in any organ or tissue makes this pathology quite common. Moreover, as doctors note, the presence of dermoid cysts can either not make itself felt for a long time or cause severe discomfort.
Cyst removal methods
Removal of a dermoid cyst in most cases is not considered a complex procedure in surgical practice. Today, clinics use the laparoscopic method when it comes, for example, to ovarian cysts.
Laparoscopic surgery has become popular due to the fact that the intervention allows for a faster recovery and has a lower risk of complications.
However, if the pathological neoplasm is very large or localized in a hard-to-reach place, it is possible to remove the cyst through classical open surgery.
Women often worry that if the ovary is damaged, they will have to remove it entirely, but this is not always the case. If the surgeon can save the organ while ridding the patient of dermoid cysts, he will do so.