Causes of development of lateral neck cyst
A lateral neck cyst or branchiogenic tumor (the name of the disease comes from the Greek word “kystis” - bubble) refers to congenital benign tumor formations, which is a consequence of pathological embryonic development of the fetus. Long-term studies indicate a direct connection with abnormal intrauterine development of the fetus in the early stages of pregnancy.
Already from the fourth week of pregnancy, the formation of the gill apparatus in the embryo occurs, consisting of 5 pairs of cavities or “gill pockets”, gill slits and arches connecting them, involved in the development and formation of the structures of the child’s head and neck. With normal anatomical development of the fetus, the gill pouches gradually become overgrown, but in some cases, they persist and form various types of cysts (lateral, median).
1.What is an arachnoid cyst and its causes?
Brain cyst
It is a connective tissue capsule filled with fluid.
The cyst can be located in any part of the brain. An arachnoid cyst
is a formation formed between the meninges, i.e. in the subarachnoid space. Depending on the time of occurrence, it can be primary (formed in utero) and secondary (acquired during life under the influence of certain factors). Arachnoid cysts are not dangerous, since cases of their degeneration into malignant formations are very rare, but over time the cyst can increase in size. This carries the risk of compression of brain tissue and problems with cerebral circulation.
Causes of the appearance and enlargement of arachnoid cysts
Primary
Brain cysts are formed during fetal development under the influence of radiation, toxic substances, infectious diseases of the mother, medications and alcohol taken during pregnancy.
Secondary
cysts appear as a result of injuries, brain infections (meningitis, encephalitis), as a result of certain types of surgical treatment, after strokes, or in areas of the brain with impaired blood circulation.
The growth of an arachnoid cyst is influenced by:
infections affecting brain tissue, trauma and concussion, gradual increase in fluid pressure inside the cyst.
The growth of the cyst requires regular monitoring using MRI diagnostics. An enlarged cyst usually indicates that the negative factor that caused its occurrence continues to affect the brain.
A must read! Help with treatment and hospitalization!
Signs and symptoms of lateral neck cyst
The lateral neck cyst is a painless, round-shaped formation with clear boundaries, having a dense and elastic consistency, which is located in the area of the so-called “carotid triangle of the neck.” As a rule, the skin over the lateral cyst is quite mobile and does not change the color of the skin. Clinical practice shows that lateral cysts can reach significant sizes, which leads to compression in the area of the larynx and trachea and causes not only dysphagia, impaired respiratory function, but also a disorder in human speech. Usually, the presence of a lateral neck cyst does not pose a health risk, but nevertheless, due to the latent form of the disease, a cervical cyst can develop into a malignant tumor.
The early stage of development of a cervical cyst can be extremely difficult to detect. This is due to the fact that there are quite a few other diseases that have similar symptoms. However, there are parameters for the symptoms of the presence of a lateral neck cyst, which manifest themselves as a result of various infectious inflammatory processes or trauma:
- the appearance of a small swelling in the area of the carotid artery; — violation of the swallowing process of food; - pain due to pressure on the neurovascular bundle; - sensation of an elastic, painless neoplasm of a mobile nature upon palpation; - enlarged lymph nodes in the neck; - displacement of the larynx; - impaired breathing and diction, the presence of stridor (a whistling sound when breathing); - suppuration with the formation of an abscess in case of infection of the cyst.
Is a brain cyst always a dangerous diagnosis?
The substance of the human brain is thin and delicate. Any foreign formation, be it a tumor or fluid, leads to disruption of the functioning of this organ, sometimes threatening the vital functions of the human body.
What is a brain cyst and how dangerous is it? Is surgery always necessary for a brain cyst or can it be done without surgery? These questions worry many. We will find out the answers to them from the executive director and chief physician of MRT Expert Lipetsk LLC, Oksana Egorovna Volkova.
— Oksana Egorovna, what is a brain cyst?
A cyst (translated from Greek as a bubble) is one of the most common pathological formations that can occur anywhere in our body. Indeed, the cyst is like a balloon filled with water, expanding as fluid enters.
This pathology actually appears quite often in the brain. If we talk specifically about a brain cyst, then more often it is a cavity filled with cerebrospinal fluid (CSF) washing the brain and spinal cord.
The symptoms of a brain cyst are very varied and depend on the location and compression of the area of the skull. However, over a long period of time, a bubble filled with fluid may not cause concern and can only be detected during an MRI of the brain.
You can sign up for a head MRI here
— How does a cyst differ from an abscess?
Abscesses on MRI look like large or small cysts, but are filled with purulent contents and surrounded by a zone of pronounced edema of the brain substance.
— What types of brain cysts are there and for what reasons do they occur?
Cysts are divided into congenital and acquired.
Congenital brain cysts are the result of a violation of the intrauterine development of the membranes of the brain. Most often, these types of cysts are localized in the temporal regions, in the posterior cranial fossa, the so-called pineal region (or pineal region). Intraventricular cysts are also congenital.
Acquired cysts are usually tumor cysts, and in this case the cyst is a “product” of tumor growth. The locations of such cysts are the lobes of the brain: frontal, temporal, parietal, occipital; cerebellar hemispheres.
Acquired cysts can also be post-traumatic in nature and occur after healing of areas of brain contusion.
Also in our practice, we encounter cysts that appear after strokes. In this case, transformation of the ischemic focus is noted. If the ischemic stroke was extensive and localized closer to the cortex, its outcome is cystic-glial changes, representing several small or large cysts, like a bunch of grapes. I note that such changes can also be a consequence of brain injuries, including in children.
What is the difference between ischemic and hemorrhagic stroke? Find out here
In some areas of our country, where a number of infectious diseases are endemic, parasitic cysts, for example, hydatid cysts, are common. Such cysts are filled with fluid, which is a waste product of this parasite.
— Are cystic-gliotic changes an accidental finding?
Yes, if a person suffered a stroke “on his feet”. Not long ago, a young patient came to our center and was treated for hypertension for three weeks. She complained of unsteady gait, dizziness, weakness, headaches and high blood pressure. The local doctor, deciding that the symptoms indicated a hypertensive crisis, prescribed appropriate treatment.
The patient made the decision to undergo an MRI of the brain on her own. We identified a fairly large area of recent cystic-gliotic changes, which allowed us to conclude that at the moment when the woman had a sharp increase in pressure, a stroke occurred. Consequently, the treatment tactics had to be different. The patient was saved from serious consequences by the fact that the stroke occurred in an area of the brain in which there are no vital centers. We can say that she was “born in a shirt.” But this doesn't always happen. Therefore, if you are not feeling well - your blood pressure is fluctuating, you are dizzy and have a headache, you are feeling weak - do not delay contacting the MRI diagnostic center. Based on symptoms alone, it is often difficult to make a correct diagnosis.
— What types of so-called “non-dangerous cysts” of the brain do doctors encounter most often?
We often find arachnoid cerebrospinal fluid cysts in our patients, as a variant of congenital formations. In the pictures we see that one of the brain lobes is larger than the other, and the free space is filled with cerebrospinal fluid. Such cysts appear due to the fact that during intrauterine development the brain was formed asymmetrically and do not entail any problems for human health.
I have met patients who were missing a fourth of their brain on one side. But at the same time, such an arachnoid cerebrospinal fluid cyst did not affect their well-being and mental activity in any way. This happens because the compensatory capabilities of the central nervous system are high. Therefore, it is not entirely correct to talk about the size that is normal for this type of cyst. From the case that I described, it is clear that even a huge arachnoid liquor cyst may not cause a person any discomfort, except headaches in case of increased intracranial pressure. Prescribing medications to normalize the outflow of cerebrospinal fluid helps such patients relieve headaches.
Epiphysis microcysts are another type of harmless cyst that is often detected during MRI studies. Their size is usually from 3 to 5 mm. If the formation is larger than the specified parameters, we recommend performing a contrast-enhanced MRI. This is necessary in order to exclude oncology.
When is the use of contrast in MRI necessary? Find out here
Large epiphysis cysts need to be observed dynamically; microcysts do not require such attention.
— What are the symptoms of brain cysts?
As for congenital ones, these are mainly “silent” cysts, which extremely rarely increase in size and lead to some kind of symptoms. This type of cyst does not pose any threat in terms of malignancy.
Secondary cysts can give symptoms, sometimes quite severe. More often these are headaches; if liquorodynamics are disturbed, there is nausea and vomiting, and focal convulsions may appear in the face, arm or leg. If the size of the cyst is so large that it leads to displacement of certain brain structures, this can lead to paresis, paralysis, and depression of consciousness.
How to relieve tension headaches? Find out here
- Can MRI determine the type of cyst?
MRI of the brain with intravenous contrast on a device with a power of at least 1.5 Tesla allows you to determine the type of cyst with high accuracy. Each type of cyst accumulates contrast agent in its own way.
— Is the diagnosis of “brain cyst” always an indication for surgery?
No. For congenital cysts that do not cause symptoms, surgery is not performed. These cysts are indicated for observation with MRI examinations every 6 or 12 months.
With acquired cysts, if we are talking about cystic forms of metastatic tumors, primary glial tumors, parasitic cysts or abscesses, the neurosurgeon often decides in favor of surgical intervention. And colloid cysts of the third ventricle are urgent situations requiring urgent surgical intervention.
— When performing surgery for brain cysts, is craniotomy always performed?
No. This depends on the location and type of cyst. For some types of cysts, cystoperitoneal shunting or microsurgical fenestration of the basal cisterns is indicated.
— Which specialty doctor should you consult if the diagnosis of “brain cyst” is indicated in the report after magnetic resonance imaging?
See a neurologist or neurosurgeon. As a rule, in recommendations, both written and oral, we indicate what specialization the patient needs to consult with a doctor.
In the photo: Volkova Oksana Egorovna
Other related articles:
What does an MRI of the pituitary gland show?
What is the difference between open and closed tomography?
Diagnosis of lateral neck cyst
To confirm the diagnosis of “ lateral neck cyst ,” a differential approach to medical examination is required using modern diagnostic equipment - computed tomography, ultrasound, and, if necessary, puncture.
As a rule, the diagnosis of a lateral neck cyst is performed if the patient has a complication in which a noticeable increase in the size of the cyst, phlegmon or a characteristic abscess is already observed. When diagnosing a neck cyst, it is very important to exclude other diseases in the neck area that have similar manifestations and similar symptoms. A branchiogenic cyst can be differentiated from the following neck diseases: neck lipoma, lymphosarcoma, lymphangioma, neck teratoma, lymphadenitis, including the nonspecific tuberculous form, glomus tumor (vagus nerve), branchiogenic carcinoma, metastases from thyroid cancer.
Diagnosis of a lateral neck cyst consists of the following steps:
- complete collection of medical history, including hereditary factors; — external examination with palpation of the neck and lymph nodes; — computed tomography of the neck with contrast to clarify the size of the tumor, its location, type of fistula, contents of the cavity; — Ultrasound of the neck; — cyst puncture (according to indications); - fistulogram or staining of the fistula tract.
Diagnostics
Most often, arachnoid cysts are localized in the middle cranial fossa where they prolapse into the widened Sylvian fissure, but can occur in other areas, including:
- interhemispheric fissure
- convexital surface of the cerebral hemispheres
- posterior cranial fossa cistern magna
- cerebellopontine angle
CT scan
Arachnoid cysts are clearly demarcated formations with non-visualizable walls, causing displacement of adjacent structures, and when large in size, causing bone remodeling at a given level. CT cisternography can help identify the connection between the subarachnoid space and the cyst.
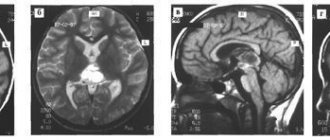
Magnetic resonance imaging
Because arachnoid cysts are filled with cerebrospinal fluid, they have similar signal characteristics including FLAIR and DWI sequences, which allows them to be differentiated from epidermoid cysts. Since their walls are very thin, it is extremely rarely possible to visualize them and only the displacement of adjacent structures allows us to suspect their presence. The absence of a solid component causes the absence of contrast enhancement. Phase contrast images can be used not only to determine the communication of the cyst with the subarachnoid space, but also to localize this connection. MR cisternography: high-resolution sequences such as CISS or FIESTA allow the walls to be defined in relation to adjacent anatomical structures.
Treatment of lateral neck cyst
Treatment of a lateral (branchiogenic) cyst is carried out only surgically. To avoid complications, the development of inflammatory processes and suppuration, surgery to remove the cyst should be performed as early as possible. Nowadays, operations for radical dissection of the cyst are not complex surgical interventions, but require high professionalism, attention and experience, since the remaining particles of the neoplasm epithelium can subsequently cause a relapse with subsequent surgical treatment.
These operations are performed under endotracheal anesthesia (tracheal intubation), the duration of the operation is from 30 minutes to one hour, depending on the location of the tumor, the age of the patient and the complexity of the case. At the end of the operation, the patient is given antibacterial and anti-inflammatory treatment. Physiotherapeutic procedures and UHF. Five to seven days after surgery, the sutures are removed. To exclude relapse, the patient is under clinical observation for one year.
Features of the development of cervical cysts and treatment in childhood
Lateral neck cysts in newborns and young children occur in a latent form and are not expressed by clinical symptoms until a provoking factor appears - trauma to the child, the appearance of a respiratory infection or other inflammatory processes. Sometimes hormonal changes in the body can become such a factor.
Clinical practice shows that in children the formation of a lateral cyst is always preceded by acute respiratory infections, influenza and other diseases of the upper respiratory tract. There is a connection between the tumor and the lymphatic tract, during which microbes of a pathogenic nature penetrate into the internal cavity of the cystic formation, causing suppuration.
In childhood, surgical treatment of a lateral cyst is carried out from three years of age outside the acute stage. But in case of serious complications leading to a threat to life, surgical intervention is indicated at an early age of the child.
Prognosis for treatment of lateral neck cyst
The prognosis of a lateral neck cyst depends on the following factors:
- general health of the patient; - age; - the size of the cyst and its localization in relation to important organs and large vessels; — duration of cyst development; - forms of cysts - inflammation, suppuration; - contents of the cavity - pus or exudate; - type of fistula; - presence or absence of chronic diseases.
In general, the prognosis for treatment of a lateral neck cyst can be considered favorable. The risk of a lateral cyst degenerating into a malignant form is extremely low.
Differential diagnosis
- expansion of subarachnoid spaces (for example, mega cisterna magna)
- epidermoid cysts often have a more heterogeneous signal on FLAIR
- pronounced restriction of diffusion
- have a more lobed structure
- cover adjacent arteries and cranial nerves
- The MR signal is different from the cerebrospinal fluid signal
- pilocytic astrocytoma
- neuroenteric cyst
- usually multiple when localized in the subarachnoid spaces
Is there a way to prevent branchiogenic cervical cysts?
Unfortunately, there are no preventive measures to prevent the development of this disease due to its nature of abnormal intrauterine conception. Most likely, this is a question for geneticists dealing with the problems of the etiology and pathogenesis of congenital anomalies of embryonic development. But, if a lateral cyst is nevertheless identified, then dynamic observation is recommended for children up to three years of age with periodic examinations every 3 months. Children should undergo regular medical examinations with a mandatory examination by an ENT doctor who can monitor the development of the tumor and eliminate various risks and complications.
Clinical case in the larynx department of the Federal State Budgetary Institution National Medical Research Center of the Federal Medical and Biological Agency of Russia
Patient M. , 26 years old, on June 20, 2016, sought medical help from specialists from the Department of Laryngeal Diseases of the Federal State Budgetary Institution National Medical Research Center for Medical and Biology of the Federal Medical and Biological Agency of Russia with a complaint about the presence of a mass on the right side of the neck. According to the patient, the formation appeared in September 2015, and gradual growth was noted. After an MRI examination and ultrasound of the neck, a diagnosis of “lateral neck cyst” . On the right side of the neck, the contours of the cyst are visualized from the mastoid process of the temporal bone to the clavicle; upon palpation it is dense, the surface is smooth.
View of the patient's neck before surgery | MRI images of patient M. | |
On June 21, 2016, the patient underwent removal of a benign neck tumor.
Surgery to remove a lateral cyst in patient M. | ||
Size of removed tumor: 20 cm by 6 cm
In the postoperative period, patient M. received antibacterial therapy, the suture was removed on the 7th day.
She was discharged on June 29, 2016 with improvement.
Photo of the patient immediately after surgery | Photo of the patient upon discharge |