Diseases of the nervous system, incl. neuroinfections, brain cysts and arachnoiditis are the specialization of our clinic. We will clarify the reason for the formation of the cyst in your case, conduct an examination for neuroinfections and the necessary treatment of the brain cyst, etc. We will be happy to help you.
- Brain cyst is a consequence of the disease
- Do brain cysts grow?
- Symptoms
- Examination and diagnosis
- Brain cyst: treatment at the Echinacea Clinic
Brain cyst is a consequence of the disease
There are two main types of cysts:
1. An arachnoid cyst is a bubble of fluid accumulated between the adherent layers of the meninges. Such cysts remain after inflammation of the meninges , hemorrhage or injury. Arachnoid cyst of the brain is not a completely correct redundant expression, since the name “arachnoid” comes from the name of the arachnoid membrane of the brain (arachna - spider). If the fluid pressure in the arachnoid cyst is higher than the general intracranial pressure, it can compress the cerebral cortex and cause unpleasant symptoms.
MRI scan of the brain. The brain is shown in grey, the fluid in black. 1 – normal slit-like fluid space between the temporal and parietal lobes of the brain. 2 – arachnoid cyst of the brain, an accumulation of fluid is visible in the substance of the brain.
2. Cerebral or intracerebral cyst (corpus callosum, subcortical nuclei, hemispheres, cerebellum, brain stem, etc.) is an accumulation of fluid at the site of a dead area of the brain. Thus, the fluid replaces the lost volume of brain matter. The cause of death should be clarified, and further destruction of the brain should be prevented. Common causes of cysts are cerebrovascular insufficiency, stroke, trauma, inflammation (encephalitis), and surgery in the cranial cavity.
MRI scan of the brain. 1 – normal fluid cavities (ventricles of the brain). 2 – Intracerebral fluid cyst at the site of a dead area of the brain.
An arachnoid cyst of the brain is always located on the surface of the brain, in the area of the membranes. Cerebral intracerebral cyst - in the thickness of the brain substance.
Causes
There are several ways of developing inflammation of the arachnoid membranes and it has been established that arachnoiditis is polyetiological and can occur as a result of such factors as:
- past acute and chronic infectious processes (including influenza , rheumatism, measles , fever , sepsis , pneumonia , syphilis , tuberculosis , brucellosis , toxoplasmosis , osteomyelitis of the skull bones);
- inflammatory diseases of the nasal paranasal sinuses;
- acute or more often chronic suppurative otitis media , especially caused by low-virulent microorganisms or toxins;
- complication of suppurative otitis media, for example, labyrinthitis , petrositis , sinus thrombosis ;
- complication of cured purulent meningitis or brain abscesses;
- chronic intoxication with alcohol, lead, arsenic ;
- various injuries - craniocerebral and spinal cord (mainly as residual effects);
- reactive inflammation caused by slowly growing tumors or encephalitis, most often non-purulent otogenic.
Do brain cysts grow?
A brain cyst is not a cancer. The size of the cyst can be easily monitored using MRI or CT scanning. If the size of the cyst has become larger over time, it means that some damaging factor continues to act on the brain. In this case, we look for and treat the causes of cysts.
The main reasons for the growth of arachnoid cysts in the brain:
- The fluid pressure in the cyst increases;
- Inflammation of the meninges continues (arachnoiditis, infection);
- Concussion in a patient with a previously formed cyst.
The main reasons for the growth of intracerebral cysts (and/or the appearance of new cysts):
- Cerebrovascular accidents continue, new foci of micro-strokes appear;
- The infectious or autoimmune process of destruction of brain matter continues (multiple sclerosis, multiple encephalomyelitis, neuroinfection).
The causes of the appearance or growth of brain cysts can usually be determined by the results of MRI, blood tests, and studies of blood flow through the vessels of the brain. Treatment is based on research results.
Classification
According to the International Classification of Diseases (ICD-10), pathology is assigned code Q04.6.
The classification of the disease is related to the location of the pathology, and the following types are distinguished:
- Arachnoid - located between the three membranes of the brain; in children, this neoplasm can provoke hydrocephalus and an increase in the volume of the skull. When diagnosing a cyst in adults, treatment is most often not required, of course, if there is no growth of pathology.
- Retrocerebellar - localized inside the organ, this neoplasm can lead to the death of brain cellular structures.
- Subarachnoid is a congenital neoplasm that can cause unsteadiness in gait, convulsions and pulsating sensations inside the skull.
- Arachnoid cerebrospinal fluid cyst - occurs in people of an older age group or those with atherosclerotic changes.
In accordance with the causes of the pathology, arachnoid cystic pathologies are divided into:
- congenital - their development occurs during the period of fetal growth in the mother’s womb, as well as during asphyxia of the child.
- acquired - develop after certain diseases, as well as under adverse environmental influences.
There is a classification of cysts according to symptoms: progressive - clinical signs increase, which is mainly due to an increase in the volume of the cystic cavity; frozen - are in a latent state and do not increase in size.
Important! To choose the correct and most effective therapy, it is very important to correctly classify the cyst.
Symptoms of a brain cyst
Symptoms are determined by the underlying disease that caused the cyst to appear. Therefore, they are diverse and nonspecific.
One or more of the following symptoms may occur:
- Headache;
- Feeling of fullness or pressure in the head;
- Sensation of pulsation in the head;
- Noise in the ear with intact hearing;
- Hearing impairment (sensorineural hearing loss);
- Visual disturbances (double vision, spots before the eyes, etc.);
- Symptomatic epilepsy;
- Paresis (partial paralysis) of an arm and/or leg, permanent or transient;
- Episodes of loss of consciousness;
- Balance imbalance;
- Numbness of any part of the body, permanent or transient.
If the brain cyst is a trace of a long-term illness, there may be a complete absence of any symptoms.
Diet for arachnoiditis
Diet for the nervous system
- Efficacy: therapeutic effect after 2 months
- Timing: constantly
- Cost of food: 1700-1800 rubles per week
Treatment of arachnoiditis is best combined with a diet based on the principles of healthy eating:
- limited consumption of seasonings and salt;
- products containing refined sugar, butter, flour are excluded;
- meat should be of dietary grades - rabbit, turkey, chicken, etc.;
- no sausages or smoked meats;
- there should be fresh vegetables and fruits on the table;
- You need to enrich your diet with baked potatoes, cabbage and carrot salads, spicy and leafy greens;
- you need to add currants, sea buckthorn, persimmons, grapes, and raisins to dishes and teas.
Examination and diagnosis
MRI or CT will provide unambiguous information about the presence, size and location of the cyst. A study with intravenous contrast helps to distinguish a cyst from a tumor You can perform such a study at the Clinic of the Academy of Sciences .
MRI scans of the brain. 1. Cyst after cerebral hemorrhage 2. Cerebellar cysts after ischemic stroke (blockage of cerebral arteries) 3. Cystic adhesive arachnoiditis
To avoid the enlargement and appearance of new cysts , we must clearly understand and treat the root cause of their occurrence. Therefore, we carefully examine you for circulatory disorders, infections, and autoimmune diseases.
Doppler ultrasound of the head and neck vessels (USDG) will help detect narrowing of the vessels that supply the brain with arterial blood. Lack of blood supply can lead to focal death of the brain matter and the appearance of cysts.
Heart studies (ECG, Echo-CG) . The brain may not have enough blood supply due to rhythm disturbances or heart failure.
Blood test for clotting and cholesterol. An increase in cholesterol concentration in the blood and increased clotting are the main causes of blockage of brain vessels with subsequent formation of cysts. This problem is easily solved with the help of modern medications.
Blood pressure monitoring. Episodic increases in pressure are a common cause of strokes and post-stroke cysts. A monitor is a small device that is constantly with you for 1 day and records your blood pressure on a memory card. The data is then read by a computer and gives the doctor a complete picture of the pressure for the day.
blood tests for infections and autoimmune diseases of the nervous system in cases of suspected neuroinfections, arachnoiditis, and multiple sclerosis.
In children
In children, this neoplasm is diagnosed based on symptomatic manifestations and the child’s medical history.
The specialist will find out whether the child has had injuries or operations in the brain, whether he or she also suffered from meningitis, or whether there have been hemorrhages.
After this, a neurological examination is performed, and a CT or MRI is also prescribed.
It must be said that this pathology is dangerous for the child. It consists in provoking persistent neurological disorders and epileptic seizures.
Under no circumstances should parents independently treat their child, much less let the disease take its course. The baby urgently needs to be shown to a doctor who will prescribe the correct treatment regimen. If the clinical picture is pronounced, surgical intervention may be required.
Clinical picture in a newborn baby:
- strong pulsation in the fontanel region;
- limbs are flaccid;
- unoriented look.
One of the clearest signs of a cyst in a newborn is severe regurgitation during or after feeding.
Useful video on the topic:
Brain cyst: treatment at the Echinacea Clinic
The first thing we will do is find out whether your cyst needs treatment and whether your poor health is associated with it. More than half of all cysts do not require treatment at all. Treatment is necessary if the cyst causes any symptoms, increases in size, or is at risk of developing new cysts. Treatment of a brain cyst is carried out regarding the underlying disease that caused its formation.
Resorption of adhesions of the meninges in arachnoid cysts - more details on the page of our website about arachnoiditis. For this purpose, we use two powerful absorbable drugs: Karipain (Karipazim) or Longidaza.
If we are talking about an infectious or autoimmune process , it is necessary to find and eliminate chronic foci of inflammation in the body. Treatment with antibiotics alone is practically useless. If arachnoiditis occurs, it means there is a gap in the immune defense, and first of all it is necessary to restore the body’s immune shield and reduce autoimmune aggression. All of our neurologists have specialized training in immunology. Based on the results of a blood test for immune status and infections, we will offer you a consistent and safe course of anti-infective and immunomodulatory treatment.
Treatment of cerebrovascular accidents requires the fulfillment of three conditions: reduction of coagulation, reduction of blood cholesterol concentration, normalization of blood pressure. Nootropics ( improve the supply of brain cells with oxygen and glucose) and Antioxidants (increase the resistance of brain cells to increased intracranial pressure) are used
In our clinic you can contact any neurologist. Be sure to take with you all the medical documents available to you, even those that, at first glance, are not related to the brain .
Retrocerebellar type formation
This is a fairly rare pathology, which is diagnosed in 5% of the population.
This neoplasm combines several types of neoplasms that differ in location:
- arachnoid,
- intracerebral - can form in any part,
- inferior retrocerebellar.
This cyst is spoken of when the tumor is localized only in the cerebellum. In this case we observe:
- migraine;
- vomit;
- paralysis and paresis;
- problems with balance;
- the image before your eyes becomes unclear;
- decreased concentration;
- deterioration of character;
- loss of consciousness;
- twitching of the eyeballs;
- deterioration of thinking;
- violation of orientation in space and time;
- decreased muscle tone.
Choroid papilloma
Choroidpapilloma is a rare tumor of the central nervous system and accounts for about 1% of all intracranial neoplasms.
It usually occurs in the ventricular system, since the site of initial growth of this neoplasm is the choroid plexus. I. Nakao et al described a unique case of ectopic choroidpapilloma located in the posterior parts of the third ventricle without connection with the choroid plexus. The tumor consists of papillary processes that are histologically similar to a normal choroid plexus. It is not characterized by invasion of the surrounding brain parenchyma. These tumors are more common in patients under 10 years of age, with a slight predominance in boys. The malignant form, choroid carcinoma, is rare and accounts for about 10-20% of choroid plexus tumors.
The most common site of choriopapilloma is the lateral ventricles in children and the fourth ventricle in adult patients. Choroid papilloma located in the third ventricle is rare (about 10% of all choroid papillomas). A careful analysis of published cases (about 80 patients) with choroid papillomas of the third ventricle showed that most of the tumors are located in the anterior parts of the third ventricle with attachment to the choroid plexus in this area.
Choroid papilloma on computed tomography (CT)
and
magnetic resonance imaging ( MRI)
is presented as well-demarcated formations located in the ventricular cavity.
The treatment method for papillomas and carcinomas of the choroid plexus is their surgical removal. In case of total tumor removal, the prognosis is generally good. Rarely, relapse may occur due to wall invasion or metastasis along the cerebrospinal fluid pathways.
In our series of patients, in one case, an 8-year-old girl was found to have choroid carcinoma of the posterior parts of the third ventricle, which was successfully removed using an infratentorial supracerebellar approach (Fig. 184).
Fig. 184. Choroid carcinoma of the pineal region.
MRI in T1 mode (a,c) reveals a heterogeneous tumor with cysts. The tumor is clearly demarcated. In T2 mode, the tumor is represented by a sharply hyperintense signal (b). MRI after total tumor removal (d).
In the postoperative period, remote gamma therapy was performed with a local field of 7x8 cm with a dose of 49 Gy. The patient was discharged from the hospital in satisfactory condition. Unfortunately, it was not possible to obtain information about the further fate of the child after discharge.
We operated on one patient with choroidpapilloma of the middle sections of the third ventricle. This case is not included in the study series, but is interesting, since the tumor was removed using an occipital transtentorial approach (Fig. 185).
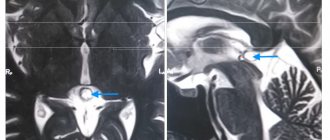
Fig. 185. Choroid papilloma of the middle parts of the third ventricle. MRI in the sagittal projection (a) reveals a small tumor in the middle parts of the third ventricle. There is pronounced hydrocephalic dilatation of the ventricular system with a breakthrough of cerebrospinal fluid into the quadrigeminal cistern through the posterior wall of the third ventricle (arrow). The presence of a large defect in the posterior wall of the third ventricle determined the choice of a posterior approach to the third ventricle
Possible complications
A progressive tumor, when it reaches a certain size, begins to compress nearby vessels and tissues. When the cerebellum is affected, a person does not properly maintain balance when walking, and fine motor skills (precise movements of the arms, hands, and fingers) are impaired.
Compression of veins and arteries leads to frequent headaches which there is no cure. Infringement of the cranial nerves means a violation of visual, auditory, and swallowing functions. Seizures can develop into epilepsy .