Classification of pathology
All cysts localized in the cerebellum are usually divided into two large groups:
- primary – that is, congenital;
- secondary – acquired pathology.
There are several types of cysts. This classification is based on the causes and location of the pathological formation:
- Cystic-glial formations in the right half of the cerebellum. They arise as a result of previous TBI.
- Cystic-atrophic cysts in the right half of the cerebellum. This pathology is characterized by the presence of necrotic and atrophied areas.
- Cystic-glial formations in the left half of the cerebellum are characterized by severe symptoms.
- Lacunar cyst in the left half of the cerebellum. These are small formations, they are usually single. This form of the disease does not require treatment.
- A retrocerebellar cyst forms in the place where there is tissue necrosis.
- Cyst-like expansion in the subarachnoid space.
- Arachnoid cerebrospinal fluid cyst.
- Pseudocyst is a congenital formation of the cerebellum.
Etiology
The causes of this pathology depend on which group it belongs to. The etiological factors for primary and secondary cysts are different.
Causes of primary formations:
- Anomalies of intrauterine development of the fetus.
- Asphyxia of the child during childbirth. In this case, necrotic areas of tissue are formed that have died from oxygen starvation.
Reasons for the development of secondary cysts:
- Traumatic brain injuries (skull fractures, concussion and bruises).
- Acute cerebrovascular accident (hemorrhagic and ischemic stroke).
- Inflammation in brain tissue.
- Surgical intervention.
- Tissue death as a result of stroke.
- Viral diseases of the brain (meningitis, encephalitis, meningoencephalitis).
- Hemorrhages from formed hematomas.
- Neuroinfections.
Features of a cerebellar cyst
When cysts are localized in areas of the cerebellum, formation occurs from the tissues that make up this organ. The cavity for fluid also acts as an anatomically located depression in the cerebellum.
During inflammatory processes, this cavity is filled with serous fluid, pus, and blood.
Signs of a cyst appear in 2 cases:
- When diagnosing chronic/congenital diseases of brain tissue.
- After a severe cerebellar disease of an inflammatory/bacterial nature.
In other situations, it can be detected after increasing to a critical size, using tomography or patient complaints about accompanying symptoms.
Clinical picture
Primary cysts most often do not manifest themselves in any way and do not interfere with a person’s life. As a rule, this pathology is not treated.
Symptoms of a secondary formation depend on its size and etiology. Small brain cysts do not have pathological symptoms; they are characteristic of large specimens. However, experts have identified several common signs of the disease:
- Severe pain in the head that is not relieved by painkillers.
- Dizziness, in some cases there is loss of consciousness.
- Bursting and pulsating sensations in the head area.
- Periodic nausea. Sometimes it ends in vomiting, which, in turn, does not bring relief.
- Disturbance of sleep and biological rhythms of patients.
- Cramps, tremor of fingers.
- Neurological symptoms.
- In children under one year of age, bulging and pulsation of the large fontanel and frequent regurgitation, in some cases vomiting, are observed.
- Coordination of movements worsens, gait changes.
- Partial or complete paresis and paralysis of the upper and lower extremities occur.
- Some areas of the skin may lose sensitivity.
- Pathological changes in hearing, vision, and speech are possible.
It is also necessary to note individual symptoms of cerebellar cysts depending on their type:
- hallucinations are characteristic of a retrocerebellar cyst;
- when the right half of the cerebellum is damaged, a person becomes quickly fatigued, both physical and mental;
- paralysis is more often observed with the development of pathology in the left half of the organ;
- hydrocephalus is a sign of cyst-like expansion of the subarachnoid space.
2.Characteristics of some common types of brain tumors
Glioma
. The tumor is formed by cells of neuroepithelial tissue, has the property in most cases to grow into surrounding tissues, is benign in nature, but is dangerous due to possible degeneration. Usually located in the cerebral hemispheres or cerebellar hemispheres.
Glioblastoma
. Also refers to glial tumors, but is malignant in nature. Such a tumor grows quickly and is densely penetrated by blood vessels, which is fraught with frequent intratumoral hemorrhages. The course of the disease is rapid, the prognosis is unfavorable.
Medulloblastoma
. It grows from embryonic tissues and is malignant. The tumor is localized in the region of the vermis and cerebellar hemispheres, often growing into the cavity of the fourth ventricle. The vast majority are registered in children. Medulloblastoma tends to metastasize along the cerebrospinal fluid into the soft membranes of the brain, ventricles and spinal cord.
Hemangioblastoma
. It grows in blood vessels and is localized in the cerebellum. The tumor is benign in nature and has some variety: it can be formed by soft tissues, be a smooth-walled cyst, or have a mixed form.
In addition to the above tumors, common brain tumors include meningiomas, papillomas, ependymomas, oligodendrogliomas, pituitary adenomas, etc.
Visit our Neurosurgery page
Diagnostics
When a patient seeks medical help, it is necessary to carry out a number of diagnostic measures to make an accurate diagnosis. First of all, anamnesis is collected (patient complaints, previous injuries, diseases). After which the patient is sent for diagnostic studies:
- Magnetic resonance imaging and ultrasound examination. These methods help to clarify the location and size of the formation, as well as to identify its nature. They should be carried out periodically to monitor the dynamics of the pathology.
- Electroencephalography. With its help, convulsive readiness is revealed.
- NSG (neurosonography). This study is only carried out on children under two years of age.
- Histology determines the nature of the formation (cyst, benign or malignant tumor).
- Laboratory examination of cerebrospinal fluid. The analysis is carried out to detect inflammation and infection.
NEURINOMA OF THE VIII NERVE
I.V. Podporina – otoneurologist of MONIKA Prof. IA Katchkov, Head, Neurosurgical Department, Moscow Regional Research Clinical Institute IV Podporina, Otoneurologist, Moscow Regional Research Clinical Institute Introduction
Neuroma (neurofibroma, neurolemmoma, schwannoma) of the VIII nerve is the most common tumor of the cerebellopontine angle. According to statistics, it accounts for 5 to 13% of all tumors of the cranial cavity and 1/3 of tumors of the posterior cranial fossa. The tumor is benign and very rarely becomes malignant. Most often, the tumor affects people of working age - from 20 to 60 years (average age - 50 years). In women, neuroma of the VIII nerve occurs 2 times more often than in men. Bilateral tumors occur in 5% of cases and more often accompany neurofibromatosis (NF) type II, or “surf noise”, “whistle”, etc., which is sometimes felt for several years, long before the development of symptoms of intracranial hypertension. Noise in the ear usually corresponds to the location of the tumor. Complaints and objective symptoms detected in patients with neuroma of the VIII nerve (according to S. Harnes, 1981)
| Complaints | Number of patients, % | Symptoms | Number of patients, % |
| Hearing loss | 97 | Suppression of the corneal reflex | 37 |
| Balance imbalance | 70 | Nystagmus | 34 |
| Noise in ears | 70 | Hypoesthesia in the trigeminal nerve area | 29 |
| Headache | 38 | Oculomotor disorders | 14 |
| Numbness on the face | 33 | Facial nerve paresis | 13 |
| Nausea | 13 | Papilledema | 12 |
| Ear pain | 11 | Babinski's sign | 8 |
| Diplopia | 9 | ||
| Facial nerve paresis | 9 | ||
| Decreased taste | 9 |
Gradually, the phenomena of irritation of the auditory portion of the VIII nerve are replaced by the phenomena of loss. First, partial deafness develops, mainly in high tones, and then complete loss of hearing and bone conduction on the side of the tumor. Patients do not pay attention to these changes for a long time, and the presence of deafness in one ear is discovered, as a rule, by chance, when there are already a number of symptoms characteristic of a tumor of the cerebellopontine angle. The latter includes a disorder of the vestibular system, expressed in systemic vestibular dizziness and spontaneous nystagmus. In this case, there is an early disappearance of the normal excitability of the vestibular apparatus on the affected side in the form of the absence of experimental nystagmus and the reaction of hand deviation during caloric and rotational tests. Along with dysfunction of the VIII nerve, complaints of pain in the occipital region, radiating to the neck, mainly on the side of the tumor, are often noted. CN compression syndromes
Subsequently, compression of other CNs occurs, while the closest of them,
the facial nerve
, running next to the auditory nerve, suffers relatively little, showing exceptional resistance compared to more distant nerves.
Symptoms from the facial nerve are expressed in mild insufficiency or paresis of its branches on the affected side, less often in spasm of the facial muscles. More severe disorders of the facial nerve develop when the tumor is localized in the internal auditory canal, where the facial nerve is strongly compressed along with its intermediate portion (the so-called XIII SN, or Wriesberg nerve), which is expressed in loss of taste in the anterior 2/3 of the tongue and impairment salivation on the affected side. As a rule, there are changes in the trigeminal nerve
.
Already at the initial stage, a weakening of the corneal reflex and hypoesthesia in the nasal cavity on the side of the tumor are detected. In advanced cases, changes in skin sensitivity are observed in the form of hypoesthesia in the area of the first and second branches, and the absence of a corneal reflex. Motor disturbances are often detected, which are expressed in atrophy of the masticatory muscles on the side of the tumor, determined by palpation, and in deviation of the lower jaw towards paralysis when opening the mouth. The next most common lesions are the abducens and glossopharyngeal nerves. Dysfunction of the abducens nerve consists of transient diplopia and failure of the edge of the iris to reach the external commissure of the eyelid when the corresponding eye is abducted towards the tumor. Paresis of the glossopharyngeal nerve is characterized by a decrease in taste or its complete absence in the posterior third of the tongue. Disorders of the XI and XII pairs of CN are less common. Disorders are detected in those tumors that grow in the caudal direction, as well as in cases where the tumor is large. Paresis of the XI (accessory)
nerve is characterized by weakness and atrophy of the sternocleidomastoid and upper trapezius muscles on the corresponding side.
Unilateral paresis of the XII (hypoglossal) nerve is expressed in atrophy of the muscles of the corresponding half of the tongue and deviation of its tip towards paralysis. Damage to the vagus nerve
is manifested by unilateral paresis of the vocal cords and soft palate with impaired phonation and swallowing.
Brainstem compression syndrome
When the tumor grows medially, disorders of both the brainstem and the corresponding half of the cerebellum simultaneously develop.
Clinical symptoms from the brain stem pathways manifest themselves mildly and often paradoxically. Mild pyramidal symptoms are observed on the side of the tumor, and not contralaterally, due to the fact that the opposite pyramid of the temporal bone puts more pressure on the pathways than the tumor itself. Sensitivity disorders, as a rule, do not occur. Cerebellar compression syndrome
Cerebellar symptoms depend not only on loss of functions of the compressed hemisphere, but also on conduction disturbances in the compressed middle cerebellar peduncle, through which the vestibular pathways pass from the Deiters nucleus to the cerebellar vermis.
The set of cerebellar disorders is expressed by the following symptoms manifested on the side of the tumor: hypotonia of the muscles of the extremities, slowness of their movements and adiadochokinesis, ataxia, overshooting and intention tremor during finger-nose and knee-heel tests, deviation in the Romberg position, often towards the affected cerebellar hemisphere, and spontaneous nystagmus, more pronounced towards the tumor. Intracranial hypertension syndrome
Symptoms of intracranial hypertension, characterized by headaches that worsen in the morning after waking up, vomiting, congestive optic discs, appear on average 4 years after the onset of the disease.
Features of the clinical picture depending on the direction of tumor growth.
Neuromas with lateral and medial growth are distinguished.
Lateral neuromas growing into the internal auditory canal are characterized by early loss of hearing, vestibular function, and taste in the anterior 2/3 of the tongue on the side of the tumor. More often, clear peripheral paresis of the facial nerve is detected. Intracranial hypertension and fundus congestion develop late. Such tumors must be differentiated from tumors of the pyramid of the temporal bone. Neuromas with a mediooral growth direction are characterized by an early increase in intracranial pressure and the early appearance of brainstem symptoms. The history in this case is shorter. Dislocation symptoms are more pronounced on the healthy side. An X-ray of the temporal bone often does not reveal destruction. Oral growth is characterized by the early development of intracranial hypertension and severe dislocation symptoms from the brain stem. Caudal growth is characterized by early gross dysfunction of the glossopharyngeal, vagus and accessory nerves. Features of the clinical picture and tactics depending on the size of the tumor
Depending on the size of the tumor, three stages of its development are distinguished. Stage I (early), tumor size less than 2 cm. Manifested by dysfunction of the trigeminal, facial, auditory nerves and Wrisberg nerve (CN XIII).
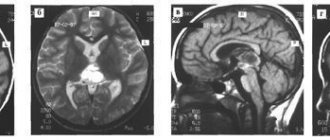
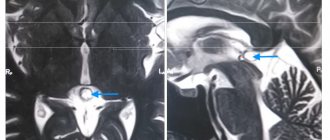
Rice. 1. Neuroma of the VIII nerve. A. MRI in T1 mode without contrast. In the left cerebellopontine angle, an extracerebral tumor is visible (shown by arrows), spreading into the auditory canal and compressing the pons. IN.
The same T1-weighted MRI image after gadodiamide contrast.
The right acoustic neuroma (shown by the white arrow) is better visualized. In addition, after contrast, a small trigeminal neuroma on the left became noticeable (shown by a black arrow). The case is typical for NF type II. MRI in T1 mode without contrast.
In the left cerebellopontine angle, an extracerebral tumor is visible (shown by arrows), spreading into the auditory canal and compressing the pons. The same T1-weighted MRI image after gadodiamide contrast. The right acoustic neuroma (shown by the white arrow) is better visualized. In addition, after contrast, a small trigeminal neuroma on the left became noticeable (shown by a black arrow). The case is typical for NF type II. Rice. 2. Neuroma of the VIII nerve. MRI with gadodiamide contrast. A small intracanalicular neuroma of the right auditory nerve is visible (indicated by an arrow).
Neuromas at this stage usually do not cause compression or displacement of the brainstem, or their effect on the pons, medulla oblongata and cerebellum is minimal. Hypertensive and stem symptoms are absent or mild. The most common local symptoms are lesions of the CN in the cerebellopontine angle, with the most common early involvement of the auditory nerve. Therefore, in patients with unilateral hearing loss, eighth nerve neuroma should be suspected until it has been ruled out. All patients with unilateral hearing impairment should be monitored over time by an otoneurologist or neurologist. At this stage, it is necessary to note the mildness of the damage to the auditory nerve, a large percentage of patients with partial preservation of hearing and vestibular excitability on the side of the tumor. Damage to the facial nerve is minimal. The Wriesberg nerve is often affected. Spontaneous nystagmus may be absent at this stage. Patients at this stage rarely see neurosurgeons, since such tumors are difficult to diagnose. At this stage, otoneurological and audiological examinations and the study of sound perception through bone are especially important. The operation is indicated for those patients in whom the diagnosis during a comprehensive examination is beyond doubt, and during a dynamic otoneurological examination the symptoms progressively increase. At this stage, the tumor must be differentiated from arachnoiditis of the cerebellopontine angle, acoustic neuritis, Meniere's disease and vascular disorders in the vertebrobasilar region. When examining patients at the stage of cochleovestibular disorders, ENT specialists often neglect to perform a caloric test, although it provides valuable information in diagnosing neuromas at an early stage. Such patients often undergo long-term treatment for auditory neuritis without results and miss the favorable time for surgery. Stage II (stage of pronounced clinical manifestations). A tumor larger than 2 cm affects the brain stem, cerebellum, and begins to cause disturbances in liquor circulation. This stage is characterized by complete loss of the auditory and vestibular portions of the VIII nerve, increased damage to the V and VII nerves, and complete loss of taste. Cerebellar and brainstem symptoms are added in the form of multiple nystagmus (clonic horizontal and vertical nystagmus when looking up), and a weakening of the optonystagmus towards the focus is noted. Dysfunctions of the neighboring CNs are more clearly manifested. Stage III (advanced stage). Spontaneous nystagmus at this stage becomes tonic, spontaneous vertical nystagmus appears when looking down. Optonystagmus disappears in all directions, speech and swallowing disturbances appear, cerebellar disorders sharply intensify, and secondary hypertensive-hydrocephalic symptoms are sharply expressed. Dislocation symptoms often appear on the opposite side.
Diagnostics
Early diagnosis of neuromas is fundamentally important, since in the early stages of development (with a tumor size of less than 2 cm), complete removal of the tumor is possible while preserving the function of the facial nerve, and sometimes hearing. Advanced tumors lead to disability; they can only be partially removed, and the facial nerve is almost always damaged. Therefore, in all patients with unilateral sensorineural hearing loss, especially in combination with vestibular disorders, it is necessary to exclude a tumor of the cerebellopontine angle, in particular a neuroma. Magnetic resonance imaging (MRI)
with contrast (gadodiamide) is the method of choice in the diagnosis of neuromas of the VIII nerve, as well as other tumors of the cerebellopontine angle.
MRI allows you to visualize tumors at the earliest stages of development (see Fig. 1, 2). Computed tomography (CT)
with contrast (iohexol) allows you to diagnose tumors measuring at least 1.5 cm. In addition, the method reveals the mass effect of the tumor: compression of the subarachnoid cisterns, hydrocephalus.
Angiography
is rarely used and only for special indications.
X-ray of the temporal bones
according to Stenvers reveals an expansion of the internal auditory canal on the side of the tumor.
Auditory evoked potentials
change in 70% of cases.
Weber's experiment
and the perception of ultrasound through bone.
In Weber's experiment, lateralization of sound may be absent, while ultrasound with neuromas is always lateralized to the better hearing ear. Lateralization of sound in Weber's experience is the main symptom in the differential diagnosis of cochlear and retrocochlear lesions of the auditory nerve. Study of vestibular function.
Unilateral loss of caloric response in all components (nystagmus, reactive deviation of the hands, sensory and autonomic components).
Audiometry.
Audiometry reveals unilateral hearing loss of the sensorineural type.
Differential diagnosis
Brain tumors.
Differential diagnosis is carried out with other tumors of the cerebellopontine angle: neuroma of the fifth nerve, meningioma, glioma, papilloma of the plexus of the fourth ventricle.
The main role here is played by CT or MRI. Lateral tumors of the brain pons. These tumors are characterized by the initial appearance of local symptoms (damage to nuclei VI, VII of the CN), isolated vomiting and respiratory failure. Next comes unilateral dysfunction of the V, IX, X, XI, XII CN. Unilateral paresis or paralysis of gaze towards the tumor develops, combined with alternating syndrome. Auditory and vestibular disorders are particularly severe. The diagnosis is confirmed by MRI or CT. Meniere's disease.
Characteristic is a paroxysmal course with painful dizziness, nausea, vomiting, noise in the ear, imbalance, spontaneous horizontal nystagmus.
Occurs more often after 45 years. In Weber's experiment, sound is laterized into the better hearing ear. Outside of an attack, there is no spontaneous nystagmus, brainstem or cerebellar symptoms. During the period of remission, patients feel good. Acoustic neuritis.
Bilateral involvement is usually observed.
Vestibular and auditory functions are not completely lost. History of previous infections, intoxications, use of ototoxic antibiotics. Absence of brainstem and cerebellar symptoms. There are no changes on the X-ray of the temporal bones. Cholesteatoma.
Cholesteatoma, being a predominantly rare complication of chronic otitis media, is a space-occupying formation and should be included in the diagnostic search with an appropriate medical history.
The disease is quite mild, with remissions, and is more common in men. Radiographs show no expansion of the internal auditory canal, and the hearing does not completely fall out. Clinical manifestation may be associated with the appearance of cerebellar or hydrocephalic symptoms. Aneurysm of the vertebral artery
due to compression of the CN may resemble the course of a neuroma.
The diagnosis is confirmed by cerebral angiography. Tuberculous meningitis.
Fever and night sweats often occur.
Positive tests for tuberculosis and cerebrospinal fluid analysis (lymphocytosis, low glucose and chloride levels) help in diagnosis. Platybasia.
X-rays of the skull and upper cervical spine reveal the following changes: the atlas is fused to the occipital bone, the tooth of the axial vertebra is located above the Chamberlain line. Other diseases with which neuroma must be differentiated are vertebrobasilar insufficiency and syphilitic meningitis.
Treatment
Surgery
– selection method.
In the initial stages of tumor growth, microsurgical removal is possible while preserving the function of the facial nerve and sometimes even hearing. In such cases, a translabyrinthine approach to the tumor is used. Hearing preservation is possible if the size of the tumor does not exceed 2 cm. Otherwise, its total removal from the translabyrinthine approach is extremely difficult. In this case, it is more advisable to use surgical access through the posterior cranial fossa (PCF), using a paramedian incision of soft tissues. The method of tumor removal is determined to a large extent by its size, anatomical and topographical features of its location, the degree of vascularization, and the characteristics of the tumor capsule. The fundamental changes that have occurred in the surgery of neuromas of the VIII nerve are associated with the use of an operating microscope and ultrasonic suction. The incidence of postoperative complications (primarily facial nerve paresis) also depends on the size of the tumor. If the tumor is less than 2 cm, then the function of the facial nerve can be preserved in 95% of cases; if the tumor size is 2–3 cm, in 80% of cases; with tumors larger than 3 cm, intraoperative damage to the facial nerve occurs much more often. Radiological treatment.
Radiation therapy is sometimes used for subtotal tumor removal, but it does not appear to affect the further course of the disease. Some Western clinics use the so-called “gamma knife” to remove neuromas, but in terms of cost and level of complications it is equivalent to conventional surgical resection. Long-term outcomes after stereotoxic radiosurgery are not yet known. Watchful waiting (conservative treatment). Since the tumor grows very slowly, in some cases, especially in elderly patients and in patients with severe concomitant diseases, a wait-and-see approach is possible, which involves monitoring the condition and performing CT or MRI over time. Palliative treatment is shunt surgery to eliminate hydrocephalus.
Literature:
1. Blagoveshchenskaya N.S. Clinical otoneurology for brain lesions. M.: Medicine, 1976. 2. Zhukovich A.V. Private otoneurology. L.: Medicine, 1966. 3. Zimmerman G.S. Ear and brain. M.: Medicine, 1974. 4. Bederson JB, von Ammon K, Wichman WW, et al. Conservative treatment of patients with acoustic tumors. Neurosurgery 1991;28:646–51. 5. Bruce JN, Fetell MR. Tumors of the skull and cranial nerves. In: Merritt's textbook of neurology. 9th ed. Williams & Wilkins 1995;326–9. 6. Collins RD. Algorithmic approach to treatment. Williams & Wilkins, 1997;4. 7. Enzmann DR, O'Donohve J. Optimizing MR imaging for detecting small tumors in the cerebellopontine angle and internal auditory canal. Am J Neuroradiol 1987;8:99–106. 8. Glasscock ME, Hays JW, Minor LB et al. Preservation of hearing in surgery for acoustic neuroma. J Neurosurg 1993;78:864–70. 9. Harner SG, Daube JR, Ebersold MJ et al. Improved preservation of facial nerve function with use of electrical monitoring during removal of acoustic neuromas. Mayo Clin Proc 1987;62:92–102. 10. Harner SG, Laws ER. Jr. Clinical findings in patients with acoustic neuroma. Mayo Clin Proc 1983;58:721–8. 11. Hart RG, Gardner DP, Howieson J. Acoustic tumors: atypical features and recent diagnostic tests. Neurology 1983;33:211–21. 12. Kasantikul V, Netsky MG, Glasscock ME, et al. Acoustic neurolemmoma. Clinical anatomical study of 103 patients. J Neurosurg 1980;52:28–35. 13. Martuza RL, Ojemann RG. Bilateral acoustic neuromas: clinical aspects, pathogenesis and treatment. Neurosurgery 1982;10:1–12. 14. Mikhael MA, Ciric IS, Wolff AP. MR diagnosis of acoustic neuromas. J Comput Assist Tomogr 1987;11:232–5. 15. Moskowitz N., Long DM Acoustic neuromas. Historical review of a century of operative series. Neurosurg Quart 1991;1:2–18.
Treatment
Treatment of this disorder is aimed at eliminating the cause and symptoms, and it is also necessary to stop the growth of the pathological formation.
In this case, two treatment methods are used:
- medicinal – in patients with small cysts;
- surgical – in the presence of large cysts.
Medicines are prescribed only by a doctor, therapy is carried out under the control of laboratory blood parameters:
- Medicines for resolving adhesions and scars (“Longidaza”).
- Antibacterial drugs to eliminate infection.
- Immunomodulators to restore the body's defenses.
- Nootropics provide better nutrition and gas exchange of brain cells.
- It is also necessary to take a number of medications, the action of which is aimed at reducing blood cholesterol, normalizing blood pressure levels and thinning the blood.
Indications for the operation:
- Development of hydrocephalus and hypertension.
- Worsening of focal symptoms.
- The presence of hemorrhage in the brain tissue.
- Cramps.
- Severe loss of coordination and balance.
In modern medicine, three types of operations are used:
- Endoscopic. This method is preferred by neurosurgeons. The operation is minimally traumatic and is performed under visual control. Complications are minimal and are not always detected. The outcome is favorable.
- Microneurosurgical operation.
- Shunting.
The last two types of surgical treatment are performed with mandatory craniotomy, which provides access to the brain.
Brain cyst (Cerebral cyst)
Arachnoid cyst
more often it is congenital or post-traumatic in nature. Located in the meninges on the surface of the brain. Filled with cerebrospinal fluid. According to some reports, up to 4% of the population have arachnoid cysts of the brain. However, clinical manifestations are observed only in the case of a large accumulation of fluid in the cyst, which may be due to the production of cerebrospinal fluid by the cells lining the cyst cavity. A sharp increase in the size of the cyst threatens its rupture, leading to death.
Pineal cyst
(pineal cyst) is a cystic formation of the epiphysis. Anecdotal evidence suggests that up to 10% of people have small, asymptomatic pineal cysts. Cysts with a diameter of more than 1 cm are observed much less frequently and can cause clinical symptoms. When it reaches a significant size, a pineal gland cyst can block the entrance to the cerebral aqueduct and block cerebrospinal fluid circulation, causing occlusive hydrocephalus.
Colloid cyst
makes up about 15-20% of intraventricular formations. In most cases, it is located in the anterior region of the third ventricle, above the foramen of Monroe; in some cases - in the IV ventricle and in the area of the transparent septum. The filling of a colloid cyst is highly viscous. The basis of the clinical manifestations are the symptoms of hydrocephalus with a paroxysmal increase in cephalgia in certain positions of the head. Behavioral disorders and memory loss are possible. Cases of weakness in the limbs have been described.
Choroid plexus cyst
is formed when cerebrospinal fluid fills the space between the individual vessels of the plexus. Diagnosed at different ages. Clinically manifested rarely, in some cases it can give symptoms of intracranial hypertension or epilepsy. Often, choroid plexus cysts are detected by obstetric ultrasound at the 20th week of pregnancy, then they resolve on their own and by approximately the 28th week of intrauterine development they are no longer detected on ultrasound.
Dermoid cyst
(epidermoid) is an abnormality of embryonic development in which the cells that give rise to the skin and its appendages (hair, nails) remain inside the brain. The contents of the cyst, along with the liquid, are represented by elements of the ectoderm (hair follicles, sebaceous glands, etc.). It is characterized by a rapid increase in size after birth, and therefore must be removed.
Consequences
Any consequences are possible if the cyst grows rapidly or ruptures. That is why it is necessary to constantly monitor the condition of this formation and carry out timely therapy.
Consequences of the pathology:
- Impaired blood circulation and movement of cerebrospinal fluid.
- The appearance of tumors at the site of the cyst.
- Disorders of speech, movement, touch and vision.
- Patient death is extremely rare.
If the cyst bursts, quite dangerous complications arise:
- Blood poisoning (sepsis).
- The purulent contents of the cyst enter the cerebrospinal fluid, which leads to inflammation.
- Bleeding inside the skull.
- Complete paralysis.
- Death of the patient.
Forecast
The prognosis depends on the severity of the pathology. If a formation in the cerebellum is detected in the early stages of development before its growth accelerates, then the prognosis is favorable. In this case, patients are cured, complications and cyst ruptures are not observed.
A fatal outcome is possible if the pathology is diagnosed too late or if proper treatment and control are lacking. Rapid growth and rupture of education occur, and pathological changes in the corresponding psychological functions are observed.
Preventive actions
Any unpleasant symptoms should not be ignored. Therefore, if the patient exhibits the above symptoms, it is necessary to seek advice from specialists (neurologist or neurosurgeon).
If a person is diagnosed with a cerebellar cyst, it is important to follow several recommendations that will help avoid complications:
- You need to visit your doctor periodically. This is necessary to monitor the patient’s condition and monitor the formation over time.
- Undergo diagnostic tests prescribed by a specialist.
- Carry out prevention against infectious diseases. You should increase the body's defenses: take vitamins, provide adequate nutrition, and healthy sleep.
- Prevent hypothermia of the body. A person should dress according to the season, avoid drafts, and keep his feet warm.
- Give up bad habits (drinking alcohol, smoking).
- It is necessary to monitor blood counts. If cholesterol or platelet levels increase, you should take medications prescribed by the doctor (prevention of blood clots, ischemia of brain tissue, and so on).
- Monitor blood pressure levels. If hypertension is observed, then constant medication is needed. This will help avoid strong pressure surges.
- If your health worsens, it is important to inform your doctor about it in order to adjust your treatment.