Brain contusion is a traumatic brain injury and is accompanied by focal damage to brain tissue and necrosis. The consequences of this condition seriously affect the entire body. The patient may suffer from functional and neurological disorders, and there is also a risk of falling into a vegetative state.
A brain contusion can occur when falling from a great height, due to a strong blow, or during an accident. The condition also varies in severity of consequences.
Mild brain contusions
They are not accompanied by a threat to life and manifest themselves with the following symptoms:
- loss of consciousness, lethargy, drowsiness, memory loss;
- dizziness, vomiting;
- changes in heart function, increased blood pressure;
- neurological disorders (tremor of the eyeballs, lack of pupillary response to light, decreased muscle tone, anisocoria);
- meningeal symptoms (neck muscle tension, Brudzinski and Kernig symptoms).
There are no serious consequences for mild brain contusions. The prognosis for the patient is favorable. Symptoms disappear within 3 weeks.
Main services of Dr. Zavalishin’s clinic:
- consultation with a neurosurgeon
- treatment of spinal hernia
- brain surgery
- spine surgery
Complications of concussion
Among the consequences of a concussion there are numerous and varied complications. Thus, repeated (repeated) concussions cause a condition called dementia pugilistica, or boxer encephalopathy; This is a form of parkinsonism of a post-traumatic nature, characteristic of people who are professional boxers and periodically experience head injuries. The works of G. Martland, who described this syndrome, indicate characteristic signs of post-traumatic encephalopathy: a slight lag in the movements of one leg or “slaps” of the foot in the early stages, sometimes problems with maintaining balance, staggering; Some patients have a clearly noticeable slowness of action and periodic confusion. Sometimes the manifestations of the disease remain mild; in other cases, dragging of the legs, retardation of movements, specific mental disorders (for example, a decrease in the vocabulary used), trembling of the head and limbs are clearly observed.
Complications resulting from a head injury can be the most severe, so to the question of what to do in case of a concussion, the answer is clear: consult a doctor; after all, a traumatic brain injury of any type and severity can lead to changes in the mental component of the personality and/or physical disorders. Such complications include:
- The occurrence of a specific reaction to drinking alcohol or infection of the body: in a drunken state, with the flu or other infectious disease, the patient experiences confusion (delirium), outbursts of overexcitation and other mental disorders.
- Vasomotor type disorders associated with changes in vascular tone. They usually appear:
- persistent, persistent headaches, the intensity of which sharply increases with physical exertion on the body or simply sudden movements;
- dizziness that occurs during physical effort and tilting the body;
- alternating rushes of blood to the head area and subsequent severe pallor with increased sweating (often such manifestations are asymmetrical and involve one half of the head);
- rapid onset of general fatigue, lack of concentration.
- Uncontrollable outbursts of emotions, increased irritability, a person’s tendency to get excited quickly, easily fly into rage, often with aggression towards others. Quite often, aggressive outbursts are followed by a period of repentance, and the patient sincerely apologizes for his behavior.
- The manifestation of concussion symptoms in the form of seizures, similar to epileptic seizures.
- Acquisition of paranoid qualities by the patient’s personality, as well as neurotic states, when a person is overly nervous about any reason, anxious, and fearful. Patients lose the ability to concentrate, complain of headaches, sleep disturbances; Vasomotor disturbances are present.
More rare complications include psychotic disorders (psychoses), when the patient hallucinates, delusions, and has poor perception of reality. In some cases, mental disorders can lead to dementia - acquired dementia, characterized by serious shifts in thinking, memory, loss of a critical attitude and the ability to navigate the real environment, and apathetic states.
More often than others, according to experts, such consequences of a concussion as a specific post-concussion syndrome occur (the name is derived from the Latin words post - “after” and commotio - “shaking”). It can manifest itself a month or a year after the injury in the form of sharp, difficult-to-bear headaches, attacks of dizziness, restlessness and sleep disturbances, and problems concentrating on any usual activity. Psychotherapeutic treatment of concussion (more precisely, its consequences) in this case is rarely effective; Symptomatic treatment is recommended, but it should be remembered that taking strong painkillers can be more dangerous than the disease itself and cause the development of drug dependence.
Moderate brain contusions
This injury usually involves a fracture of the skull bones and is accompanied by subarachnoid hemorrhage. She shows herself:
- loss of consciousness for 1–3 hours, psychomotor agitation;
- amnesia;
- severe dizziness;
- nausea;
- vomiting;
- intense headaches;
- high blood pressure, rapid heartbeat;
- increased body temperature;
- meningeal symptoms;
- severe focal neurological symptoms (changes in muscle tone, paresis, loss of sensation in the limbs, epileptic seizures, speech impairment, etc.).
Signs of moderate brain contusions persist from several weeks to 2 months. The consequence of this condition may be irreversible changes that occurred during the injury.
Short-term complications of concussion
Some patients who have suffered a concussion may experience so-called post-stress disorders:
- persistent headaches lasting 7-14 days, the intensity of which decreases when taking analgesics or painkillers of other groups;
- attacks of dizziness, difficulty concentrating, difficulty performing any normal activities (reading, writing, etc.);
- periodic vomiting for no apparent reason, feeling of nausea.
Most often, the side effects of a concussion disappear after some time without treatment; if they bother the patient for several months, you should visit a doctor and get an appointment for a consultation with a neurologist or a brain tomography (magnetic resonance, computer) to clarify the diagnosis.
Severe brain contusions
Such an injury poses a threat to human life. The consequences of a severe brain injury are serious, and recovery takes several months. Often the victim never fully recovers.
The following signs indicate a severe brain injury:
- loss of consciousness, after which the person is in stupor or a state of stupor;
- temperature rise to 41°C;
- psychomotor agitation, convulsive syndrome;
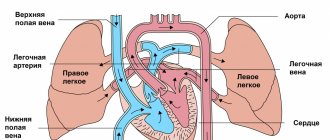
- disturbances in the respiratory and circulatory system (up to the need for artificial ventilation);
- neurological symptoms (dilation or constriction of pupils, “floating” eyeballs, difficulty swallowing, paralysis, loss of speech);
- pronounced meningeal signs.
Severe brain effects regress extremely slowly. Recovery takes a long time. In some cases, the patient becomes disabled.
The most common consequences of brain contusions are:
- inflammation of the meninges;
- epilepsy;
- atrophy (decrease in tissue volume) of the brain;
- hydrocephalus accompanied by intracranial hypertension;
- scars on the meninges and tissues;
- cerebrospinal fluid cysts;
- post-traumatic porencephaly;
- liquorrhea (due to a skull fracture).
These conditions are accompanied by movement disorders, dizziness, impaired coordination, speech, mental disorders, headaches, decreased intelligence, and convulsive seizures.
Traumatic brain injuries. Causes. Symptoms Diagnostics. First aid
home
Traumatic brain injuries are a major socio-medical problem, since their prevalence remains quite high, while injuries most often occur in people of working age, and its consequences can persist throughout life, leading to loss of ability to work and huge economic costs for the rehabilitation of the patient.
In this regard, it is necessary to understand that already the first signs of TBI, and we are talking, first of all, about loss of consciousness, require seeking specialized medical help. And the sooner help is provided and full treatment is carried out, the more effective it will be, and the less likely there will be to develop serious and irreversible consequences of the injury.
Our ambulance is one of the most mobile, and the qualifications of our specialists are beyond doubt. Therefore, we advise you to immediately call our ambulance team if you suspect that a person has suffered a traumatic brain injury before your eyes. And the sooner you make the call, the more effective the help will be.
Causes of traumatic brain injury
In fact, the causes of traumatic brain injury can be very diverse, but the most common are:
- caused by traffic accidents
- may be caused by work-related injuries
- obtained at home
- are the result of sports injuries.
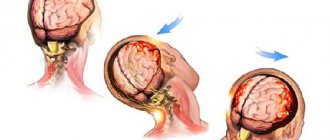
At the same time, the cause of the traumatic brain injury also influences the course of the disease. Thus, when you hit the head with a heavy object or fall, focal lesions or hematomas often occur in the epidural or subdural space, while in road traffic accidents (emergency braking), diffuse brain damage occurs.
In any case, a patient with a traumatic brain injury requires emergency hospitalization , and if not even for treatment (for a mild concussion), then to perform a full examination and exclude the presence of more severe injuries.
Therefore, an ambulance must be called immediately, because only in this case will hospitalization be carried out as soon as possible and in a specialized department. An attempt to independently transport a patient to a hospital often leads to a significant loss of time until the proper department is found, the scope of necessary research is determined, and so on. And lost time means a high probability of developing complications and subsequent disability of the patient.
If a person suffers a severe traumatic brain injury in a motor vehicle accident or for any other reason, resuscitative transport may be required if the patient is unconscious and breathing and cardiac function are impaired. In this case, our paid ambulance will become indispensable, since we have everything necessary to quickly transport the patient to the hospital, as well as provide emergency assistance at the transportation stage.
Symptoms of traumatic brain injury
It cannot be said that traumatic brain injury is manifested by strictly defined symptoms, since the clinical picture depends on the active factor, its strength, the depth of brain damage, the presence of focal changes, and so on.
With closed craniocerebral injuries, the skin and bones of the cranial vault may not be affected, so at first glance there may be no signs of injury, but symptoms of TBI are always observed, such as:
- loss of consciousness for at least a few seconds
- presence of nausea or vomiting
- retrograde amnesia (a person does not remember the events that immediately preceded the injury).
With an open craniocerebral injury, in addition to loss of consciousness, damage to the skin and bones of the skull is observed, while if the dura mater remains intact, then the injury is considered non-penetrating, and if damaged, then penetrating. When the bones of the skull are fractured, external signs of skin damage may not be immediately visible, but a characteristic symptom is the leakage of cerebrospinal fluid (a clear liquid) from the ear canal or nose, and blood may also leak. Also characteristic is the so-called “glasses symptom” - hemorrhages under both eyes.
With diffuse brain damage, general cerebral symptoms will occur, which boil down to:
- severe headache
- possible photophobia
- tinnitus, loss of coordination of movements
- most often there is nausea, in some cases there may be vomiting, which does not bring relief.
If a focal lesion occurs, for example, a hematoma occurs, then the appearance of focal symptoms may be observed:
- paresis or paralysis in the limbs
- sensory disturbances
- facial nerve paresis
- the appearance of drooping eyelids, differences in pupil size, and so on.
The main factor for diagnosis is still the presence of a history of trauma. Therefore, if you witnessed a person fall or get injured in another way, you saw that the person then lost consciousness, then other symptoms are no longer needed to try to call a paid ambulance as soon as possible, in order to provide first aid as quickly as possible and deliver the person to a specialized medical institution.
Please note that sometimes a person can fall due to a brain accident, for example, a stroke, as well as during an epileptic seizure, and so on. In this case, the blow may be such that, against the background of already existing changes, an injury will be sustained. Therefore, the injury may be of secondary origin, but in any case, the patient requires the fastest possible care and hospitalization in order to increase the chances of survival and full recovery.
Diagnostic approaches for TBI
Of course, the main method for diagnosing TBI is an examination by a specialist, since after the first examination by a doctor and clarification of the medical history, one can conclude that there is a TBI or other pathology. In addition, the first examination suggests the presence of a certain type of traumatic brain injury, as well as the degree of its severity.
It is after this that the range of further examinations is determined. Therefore, you need to call a doctor to a patient with a suspected traumatic brain injury as soon as possible. And only a paid ambulance in this case is an adequate solution, since it not only arrives on site in the shortest possible time, but also has all the capabilities to carry out full resuscitation measures that a patient with a traumatic brain injury may need.
Transportation of the victim should be carried out as soon as possible and only to specialized clinics where there are opportunities to conduct research such as:
- radiography of the skull bones
- computed tomography of the brain
- lumbar puncture
— electroencephalography.
Please note that traumatic brain injury can lead to the development of cerebral edema, which requires emergency treatment, but lumbar puncture, which can be fatal, is strictly contraindicated. That is why it is important to take the patient to a specialized clinic and perform the full range of necessary examinations in order to determine emergency measures.
Treatment of traumatic brain injury
Treatment of traumatic brain injury is complex and lengthy, and in many cases also very controversial. Only the mildest concussions do not require specific treatment, while some traumatic brain injuries cannot be treated without surgical intervention.
In any case, the amount of necessary treatment is determined by the doctor after conducting appropriate studies. At the first stages, the two most important tasks are:
— provision of emergency first aid
- emergency hospitalization.
First aid is to:
- place the patient on his back
- turn your head to the side
- stick out your tongue to prevent aspiration of vomit
- unfasten the collar and provide fresh air if the patient is not outside
- try to stop bleeding, if any.
- in the presence of
- administer a painkiller
- Call an ambulance as quickly as possible.
Call our paid ambulance , be confident in the mobility of our teams and the high competence of specialists who have already saved hundreds of lives!
Principles of assisted ventilation.
If modern breathing equipment is available, oxygen therapy should be abandoned during spontaneous breathing of the patient in favor of assisted ventilation.
This eliminates the risk of respiratory depression when using elevated oxygen concentrations. The incoming respiratory mixture is cleaned of foreign impurities, including bacterial ones, by passing through the filters of the respirator. It is possible to accurately dose oxygen and humidify the mixture. In addition, modern respirators make it possible to analyze a number of indicators of pulmonary mechanics (minute volume of ventilation, airway resistance, etc.) and thus monitor the patient’s condition and prevent episodes of apnea and hypoventilation. Assisted ventilation modes are preferred, as this facilitates the synchronization of the patient's breathing attempts and the operation of the respirator. Our special studies have shown that the current ideas about the “harmful” effect of mechanical breathing on ICP are unfounded. ICP increases not due to the transfer of the patient from spontaneous ventilation to support with a respirator, but when the operation of the device and the patient’s respiratory movements are not synchronized. Therefore, the following respiratory support algorithm is recommended. Basic ventilation parameters are set to ensure the supply of respiratory mixture in normal ventilation mode (usually 8-9 l/min). The sensitivity of the respirator is selected, high enough not to cause desynchronization, and “coarse” enough not to cause autocycling of the ventilator (usually 2-4 cm H2O). The patient is provided with a mandatory specified minute volume of breathing. If necessary, the respirator, having detected an additional breathing attempt, increases the supply of the oxygen-air mixture. The mode of auxiliary ventilation is practically irrelevant. Modern ideas about the leading importance of barotrauma in the development of lung damage during mechanical ventilation dictate the need for careful control of peak pressure in the respiratory tract, which should not exceed 30-35 cm of water. Art. From this point of view, pressure ventilation modes are justified. A small (3-5 cm H2O) positive end-expiratory pressure is also necessary to prevent expiratory closure of the airways and the development of macro- and microatelectasis. Our studies have shown that this maneuver does not affect ICP. Not only hypoventilation, leading to hypoxia and hypercapnia, is dangerous, but also hyperventilation. We, as well as other researchers [8], have found that deliberate hyperventilation must be avoided. The resulting hypocapnia causes constriction of cerebral vessels, an increase in cerebral AVPO2, and a decrease in cerebral blood flow. At the same time, if for any reason, for example, due to hypoxia or hyperthermia, spontaneous hyperventilation develops, to stop it, you cannot simply use mi-orel axanthas and “impose” the desired volume of ventilation on the patient using a ventilator. Due to the rapid normalization of carbon dioxide levels in the blood and developing brain hyperemia, there is a serious danger of severe intracranial hypertension. It is necessary to eliminate the reasons for the increase in minute ventilation: relief of hyperthermia, correction of hypoxia (the latter may be due to airway obstruction, insufficient oxygenation of the respiratory mixture, hypovolemia, anemia, etc.). If necessary, it is possible to use sedatives in order to reduce the body's oxygen consumption and reduce the required minute ventilation.
The use of auxiliary ventilation modes makes it possible to facilitate the transfer of the patient to independent breathing by reducing the number of mandatory breaths of the ventilator with a gradual transition to spontaneous ventilation through a respirator in the mode of constant positive pressure in the respiratory tract. But, unfortunately, it is not always possible to use ventilators that provide sufficient humidification of the respiratory mixture and recognition of the patient’s breathing attempts. As a result, sedatives and muscle relaxants must be used to synchronize the patient’s respiratory movements with a respirator. Naturally, this complicates the assessment of the patient’s neurological status, suppresses the cough mechanism, and does not allow the patient to compensate for the occurrence of hypoxia with his own breathing attempts. The use of hyperventilation modes, as recommended by some authors [2], seems even less preferable for the reasons stated above about the undesirability of hypocapnia. In this situation, you can try to limit yourself to the use of inhalers and nebulizers with heating and oxygenation of the respiratory mixture. However, any deterioration of the patient’s condition in the form of increasing depression of consciousness, the occurrence of bronchopulmonary purulent complications, instability of central hemodynamics requires transfer to mechanical ventilation in order to avoid increasing cerebral hypoxia.