Concussion is one of the most common diagnoses in pediatric traumatology. Overall, traumatic brain injury (TBI) ranks first among all childhood injuries requiring hospitalization. Approximately 120 thousand children with concussion are admitted to Russian hospitals every year.
According to the severity, traumatic brain injury is divided into mild (concussion), moderate (mild to moderate brain contusion, with possible fractures of the cranial vault) and severe (severe brain contusions, intracranial hematomas with compression of the brain, fractures of the base of the skull). Fortunately, up to 90% of childhood TBIs are concussions, which is what this article will discuss.
The high level of injuries in children is explained by the child’s increased motor activity, restlessness and curiosity, which is combined with imperfect motor skills and coordination of movements, as well as a reduced sense of danger and fear of heights. In addition, in young children, the head has a relatively large weight, and the skill of belaying with hands has not yet been developed, so small children, as a rule, fall upside down and do not use their hands.
The causes of childhood TBI are very specific to each age group. Newborns in the total mass of victims make up 2%, infants - 25%, toddlers - 8%, preschool children - 20% and school-age children 45%.
Injuries in infants are primarily the result of the inattention and carelessness of their parents. Children under 1 year of age most often (more than 90%!) receive head injuries after falling from changing tables, beds, from parents' arms, from strollers, etc. You should never leave your baby alone in a place where he could fall. If you need to move away from your child at a distance greater than an outstretched hand, do not be lazy, put him in a crib, in a stroller with sides, in a playpen! One or two seconds is enough for the baby to roll to the edge of the changing table and fall.
From 1 year
babies begin to walk. The main cause of TBI is a fall from one’s own height, and a little later - falls from stairs, trees, roofs, windows, slides, etc. The episode of TBI itself is not always possible to identify. It should be borne in mind that if the child remained under the supervision of relatives, neighbors or a nanny, then they can hide from the parents the fact that the baby fell.
Older children
For various reasons, they themselves often hide the trauma.
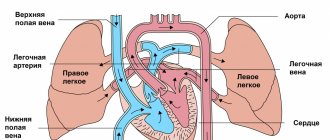
In addition, children may experience brain damage without direct head trauma. These injuries usually occur when a child's body is subjected to sudden acceleration or deceleration (shaken baby syndrome). “Shaken baby” syndrome is most often observed before the age of 4-5 years
and can occur with rough handling, jumping from heights, and in young children even with excessively intense rocking.
Manifestations of a concussion
With a concussion, there are no gross, irreversible changes in the brain, and such an injury, being the most common, has the best prognosis and very rarely leads to complications.
It should be remembered that the brain of a child (and especially an infant) is significantly different from the brain of an adult. The course of a concussion in adults differs significantly from the course of this injury in a child.
In adulthood, a concussion is manifested by the following main symptoms: an episode of loss of consciousness from a few seconds to 10-15 minutes; nausea and vomiting; headache; amnesia (loss of memory) of events associated with the trauma (before the trauma, the trauma itself and after the trauma). In addition, some specific neurological symptoms are detected, such as nystagmus (twitching of the eyeballs), impaired coordination of movements and some others. The picture of a concussion in a child is completely different.
In children under 1 year
A concussion, as a rule, is asymptomatic. Loss of consciousness often does not occur; single or repeated vomiting, nausea, regurgitation during feeding, pale skin, causeless restlessness and crying, increased drowsiness, lack of appetite, and poor sleep are noted.
In preschool
More often it is possible to establish the fact of loss of consciousness, nausea and vomiting after injury. They experience headaches, increased or slow heart rate, instability of blood pressure, pale skin, and sweating. In this case, moodiness, tearfulness, and sleep disturbance are often noted.
Sometimes children experience a symptom such as post-traumatic blindness. It develops immediately after the injury or a little later, persists for several minutes or hours, and then disappears on its own. The reason for this phenomenon is not completely clear.
The characteristics of a child’s body lead to the fact that a long-term state of compensation can be replaced by a rapid deterioration of the condition. That is, immediately after the fall the child feels satisfactory, but after a while symptoms appear and begin to rapidly increase.
First aid
After an injury, parents should pay close attention to the child’s condition. Symptoms of a concussion in a 5-year-old child are easier to recognize. The baby can already describe his feelings.
You must not allow panic, fuss, or upset or frighten the child. It is important to ask him, if possible, about the existing complaints and the reasons for what happened. It is necessary to call an ambulance and while waiting for doctors to arrive, it is not recommended to do the following:
1. Carry out independent treatment.
2. Shake the child when he loses consciousness.
3. Place the baby on his back.
4. Leaving the child unattended.
5. Give anesthetics.
6. Take the child to the medical facility yourself.
If a child loses consciousness after an injury and vomits, it is allowed to lay him on his side until the doctors arrive. The legs should be bent at the knees and the hands should be placed under the head. The child's position must be stable. Next, parents need to take the following steps:
1. Inspect the head for bone damage.
2. If there is a wound, it is treated with an antiseptic solution. This could be hydrogen peroxide or chlorhexidine.
3. Apply a bandage to the wound.
4. Apply ice to the injured area.
5. Don't let your child sleep.
6. Limit movements.
7. Keep the child's condition under control.
Every parent should know the signs and symptoms of a concussion in a child.
It is advisable that parents master the technique of artificial respiration, as well as indirect cardiac massage. This may be necessary to carry out resuscitation measures until paramedics arrive. After calling an ambulance, parents should:
1. In case of fainting, place the child in such a way that the head is not higher than the body.
2. Measure your pulse.
3. Determine the presence of heartbeat and breathing.
4. Examine the child for fractures and injuries to other parts of the body.
5. Question witnesses to the incident, if any.
Doctors will also conduct an initial examination of the child and hospitalize him along with his parents, who must provide a complete medical history of the victim.
We are taking urgent measures
What should parents do if their child has suffered a traumatic brain injury? There is only one answer: the child should definitely and urgently be shown to a doctor. It is best to immediately call an ambulance, which will definitely take the child to a hospital with pediatric neurosurgeons or neurologists. And this measure is not unnecessary. With minimal symptoms and complaints, the baby may have severe brain damage. The long-term visible well-being of the child, the absence of symptoms, especially with hemorrhages in the brain, often after a few hours and even days is replaced by a progressive deterioration of the condition, which begins with a change in the child’s behavior, his increased excitability, there may be nausea, vomiting, nystagmus, and in infants the fontanelle bulges , then drowsiness appears, depression of consciousness is observed.
Do they put you in hospital?
And if so, in which department are patients with a similar diagnosis located? Moderate or severe concussions require hospital treatment. Such patients are placed in a traumatology, neurosurgical or neurological department.
What are they doing in the hospital? The main task of doctors and nurses is to exclude the presence of severe injuries and provide the patient with strict bed rest for at least the first few days.
Typically, the range of medications prescribed on admission includes painkillers, sedatives and sleeping pills, mainly in the form of injections and tablets. Nursing care means that the nurse brings medications prescribed by the doctor and monitors his compliance with bed rest.
Diagnosis of concussion
In the hospital, the child is examined by a pediatric neurologist, neurosurgeon or traumatologist. He carefully ascertains complaints, collects anamnesis (history of the disease), and conducts a general and neurological examination. Additional diagnostic methods are prescribed. The main ones are skull radiography, neurosonography (in young children), echo-encephalography (Echo-EG). If necessary, computed tomography of the brain (CT), magnetic resonance imaging (MRI), electroencephalography (EEG), lumbar puncture.
Radiography
skull is performed in most patients. The purpose of this study is to identify skull fractures. The presence of any damage to the bones of the skull automatically transfers the injury to the category of moderate or severe (depending on the condition of the child). Sometimes in young children with a favorable clinical picture, linear fractures of the skull bones are revealed on radiographs. It is impossible to judge the state of the brain substance from radiographs.
Neurosonography
(NSG) is an ultrasound examination of the brain.
Neurosonograms clearly show the substance of the brain and the ventricular system. You can identify signs of cerebral edema, areas of contusion, hemorrhages, and intracranial hematomas. The procedure is simple, painless, quickly performed, and has no contraindications. It can be done multiple times. The only limitation of neurosonography is the presence of so-called “natural ultrasound windows” - a large fontanelle or thin temporal bones. The method is very effective in children under 2 years
. Later, ultrasound becomes difficult to pass through the thick bones of the skull, which dramatically degrades image quality. Equipment for performing neurosonography is available in most children's hospitals.
Echo-encephalography
(Echo-EG) is also an ultrasound research method that allows you to identify displacement of the structures of the midline of the brain, which may indicate the presence of additional space-occupying formations of the brain (hematomas, tumors), and provide indirect information about the state of the brain substance and the ventricular system. This method is simple and fast, but its reliability is low. Previously, it was widely used in neurotraumatology, but with the availability of modern diagnostic tools, such as neurosonography, computed tomography and magnetic resonance imaging, it can be completely abandoned.
The ideal method for diagnosing brain damage and diseases is computed tomography.
(CT). This is an x-ray research method in which high-definition images of the skull bones and brain matter can be obtained. CT can diagnose almost any damage to the bones of the vault and base of the skull, hematomas, bruises, hemorrhages, foreign bodies in the cranial cavity, etc. The accuracy of this study is very high. Its main disadvantage is that the CT machine is expensive, and not every hospital has it.
Magnetic resonance imaging
(MRI) is the most accurate, but complex and expensive method of examining the central nervous system. It is rarely used to diagnose acute traumatic brain injury because it does not allow the bones of the skull to be seen, is less accurate for recognizing acute hemorrhages, takes longer than computed tomography, and often requires anesthesia when examining small children - the child must lie absolutely still for 10 -20 minutes, but small children cannot do this; In addition, very few clinics can boast of having magnetic resonance imaging scanners.
Advertising
Electroencephalography
(EEG) allows you to study the bioelectrical activity of the brain. It is used for special indications to assess the severity of traumatic brain injury and identify foci of epileptic activity. A focus of epiactivity is an area of the cerebral cortex with pathologically altered activity of neurons (nerve cells), which can lead to epileptic seizures.
Lumbar puncture
- this is the collection of cerebrospinal fluid (the fluid that bathes the brain and spinal cord) from the spinal canal at the lumbar level. Changes in the cerebrospinal fluid may indicate injury or hemorrhage (the presence of blood) or an inflammatory process, meningitis. Lumbar puncture is performed extremely rarely and only for special indications.
What do they do in the hospital with such patients?
How does a doctor determine a concussion?
Let's look at how a specialist determines whether a patient has a concussion. The primary goal of the attending physician during a concussion is to rule out the presence of skull fractures, intracranial hematoma, or subarachnoid hemorrhage. Before treatment for a concussion of any severity, a brain examination is performed.
First of all, if cracks or fractures of the skull bones are suspected, bone x-rays are prescribed . Brain tissue damage and possible hematomas are examined using CT and MRI. It is possible to use Doppler ultrasound to examine vascular changes. But first of all, the study is carried out by interviewing the victim and those who were nearby at the time of the injury. Mild and moderate concussions usually have no obvious symptoms.
If there is no fracture of the skull bones, the patient’s blood pressure has returned to normal, then to confirm the diagnosis, the doctor interviews the victim and his relatives in detail about the state of health and the circumstances of the injury.
Concussion is a clinical diagnosis; it is most often established on the basis of complaints and external examination data. After the examination, the doctor will prescribe a course of treatment. If the concussion is mild, he will be sent for treatment at home.
How are they treated?
In the absence of severe symptoms, the doctor will prescribe drugs that improve blood circulation in the brain, nootropic drugs - if there are memory problems, anticonvulsants, non-narcotic painkillers and anti-inflammatory drugs to relieve headaches.- They will also recommend mild sedatives - teas with mint and lemon balm, valerian tablets.
- He will recommend staying in bed for several days, not reading books or watching TV, categorically prohibiting working at the computer and prescribing additional medications depending on the patient’s complaints.
Classification of traumatic brain injuries
According to one classification, traumatic brain injuries are divided into:
- Open TBIs are head injuries in which the integrity of soft tissues and skull bones is damaged. If the dura mater is also damaged, the injury is called penetrating. In other words, the traumatic agent penetrates not only into the cranial cavity, but also reaches the brain. There is a threat of infection, which dramatically aggravates the injury.
- Closed head injuries are injuries to the head in which the integrity of the soft tissues (or there are only minor abrasions or scratches) and the bones of the skull is not compromised. Most often, when falling from a height, children in the first year of life receive closure of the TBI.
1Dura mater - one of the three membranes of the brain, the outer one, adjacent in the cranial cavity to the inner surface of the bones, consisting of dense fibrous connective tissue; has a protective function.
In turn, closed injuries are divided into:
- concussion (without division into severity);
- mild, moderate and severe brain contusion;
- brain compression.
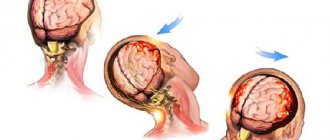
Concussion (commotio) is a mild form of traumatic brain injury. Damage to the brain occurs at the molecular level (molecules are shaken), and its functions are disrupted, but there are no obvious changes in the structure of the brain substance.
Brain contusion (contusio) is a brain injury characterized by the appearance of a focus/foci of destruction of the brain matter of varying severity. The lesions can be single, multiple, different in depth and location.
In this case, the patient develops neurological disorders (for example, the inability to follow moving objects with the eyes, etc.) and/or psychological changes.
Compression of the brain (commpressio) is a severe damage to the substance of the brain, which, as a rule, occurs against the background of a brain contusion and is extremely rare without it. The cause (pressure of the brain) may be the accumulation of blood inside the skull as a result of a ruptured vessel, or the brain may be compressed by fragments of the skull in a so-called depressed fracture.
Typical cases of traumatic brain injury in infants
- The baby lies on the changing table or on the sofa, the mother turns away for a few moments, and the baby falls on his butt.
- The baby is left unattended in a high chair. He pushes off the table with his feet and falls on his back along with the chair.
- The baby is trying to get up in the crib. Something on the floor interested him, and he hangs over the side and falls.
- The little one was left sitting in the stroller, not expecting that he would try to stand up in it and, not finding support, would fall down.
Drug treatment
Conservative treatment of concussion symptoms in children aged 3 years aims to improve the general condition of the sick child. All this helps prevent the consequences of injury. The most commonly prescribed drugs are:
1. Nootropics aimed at improving blood circulation in the brain and metabolic processes - “Pantogam”, “Cavinton”.
2. Diuretics that prevent edema - Diacarb, Furosemide.
3. Sedatives that help relieve nervous excitability - “Tenoten for children”, “Phenibut”.
4. Potassium-containing ones help regulate blood pressure and prevent increased fatigue - “Asparkam”, “Panangin”.
5. To speed up recovery after injury, children are prescribed various vitamin complexes, such as Pikovit, Alphabet, etc.
In addition, symptomatic treatment is carried out, including:
1. Painkillers – “Baralgin”, “Sedalgin”.
2. “Cerucal”, which prevents vomiting.
3. Antihistamines with a hypnotic effect - “Diazolin”, “Suprastin”.
"Pantogam" can be prescribed to children from the first days of life. The drug is produced in the form of a sweet syrup and is quite often used in neonatological practice when nursing premature babies. Nootropic drugs have a number of features. They help increase brain activity, improve memory, and also have an anticonvulsant and sedative effect. Treatment with Pantogam can be long-term and up to six months.