Make an appointment by phone: +7 (343) 355-56-57
+7
- About the disease
- Cost of services
- Sign up
- About the disease
- Prices
- Sign up
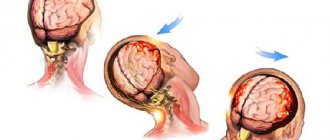
A concussion is a form of traumatic brain injury. In which short-term memory loss may occur, brain dysfunction is reversible. Usually the cause is various traumatic situations. In case of injury, the protective fluid is not able to prevent the impact of brain tissue on the bone tissue of the skull. The injury requires hospitalization and consultation with a specialist.
Classification
Concussion is classified into three degrees:
1.
Mild degree.
The victim is conscious, and within half an hour after the injury there are typical complaints of headache, dizziness, nausea, and disorientation in space. After half an hour the condition returns to normal. 2.
Average.
Consciousness is preserved, short-term memory loss occurs, the symptoms are similar to mild, dizziness persists, there may be a headache, nausea, the victim is disoriented in space. 3.
Severe degree. For her, loss of consciousness lasting a couple of minutes, maybe several hours, is accompanied by retrograde amnesia. Symptoms of headache, dizziness, nausea, disorientation in space can remain for two or three weeks, problems with sleep, and loss of appetite occur. Organic brain lesions lead to the appearance of vascular dementia. This is a secondary disease, that is, occurring against the background of some pathological process. The main reason is a previous ischemic or hemorrhagic stroke.
Recommendations for the treatment of concussions
If hospitalization is not required, with the permission of a doctor, a mild concussion can be treated at home:
- Bed rest and rest are required, no work. Long sleep is very important.
- You cannot read, watch TV, play computer games or use gadgets.
- Under no circumstances should you play sports.
- You are allowed to listen to music, but not through headphones.
- You can use herbal sedative drops or herbal infusions.
- In your diet, you should give preference to dairy and plant products, limit salt intake - to prevent increased pressure, including intracranial pressure.
If the patient seeks medical help in a timely manner and all recommendations are followed, recovery will occur quickly and without complications.
Symptoms of a concussion
General symptoms:
The victim complains of memory loss, dizziness, tinnitus, double vision, intense headache, nausea leading to vomiting, and fatigue. There is sleep disturbance, daytime sleepiness, irritability, and emotional lability. After the injury, confused speech appears, short-term memory loss (retrograde, anterograde amnesia), increased sensitivity to light, noise, balance is disturbed, uncoordinated movements, smell and taste are lost.
Symptoms that may bother you for a longer period:
- intense headache, may be migraine;
- difficulties with reading, remembering, writing;
- absent-mindedness, difficulty concentrating;
- nausea, vomiting;
- drowsiness, weakness;
- dizziness.
Causes of a concussion
Regardless of how the bruises were received, they end with the brain hitting the inner walls of the skull. The result is not long in coming, expressed in swelling of varying intensity. It is the swelling that causes the leading symptoms of a concussion to appear.
An external mechanical influence due to increased pressure on the head can provoke such a phenomenon. This definition even includes everyday hits against lockers or during a game of football. Sometimes this pathology is a consequence of a sharp fall or sudden braking of a vehicle.
In ordinary life, most often the victims of the condition are children of approximately school age who do not control their strength during various outdoor games, as well as elderly people who suffer from unsteady gait and often fall.
If you use the diagram of the main signs of a concussion, you can diagnose it for almost any person. The sooner medical care is provided to the victim, the faster he will complete his rehabilitation course. Even with consistently positive dynamics, recovery will take about a week. Reducing these periods threatens the development of complications.
It is impossible to predict how serious the consequences of ignoring an injury may be. It is believed that in the absence of timely medical care, patients in the future will not be able to quickly cope with even the simplest tasks. Such inhibition can be observed for months.
Also, untreated patients have an increased risk of developing:
- alcohol addiction;
- Parkinson's disease;
- sudden death.
To prevent a sad outcome, it is worth learning to recognize threatening symptoms and provide quality first-aid care.
Diffuse axonal brain injury
Diffuse axonal brain damage is typically characterized by a prolonged coma after a traumatic brain injury, as well as pronounced brain stem symptoms. Coma is accompanied by symmetrical or asymmetrical decerebration or decortication, both spontaneous and easily provoked by irritations (for example, painful ones). Changes in muscle tone are very variable (hormetonia or diffuse hypotension). A typical manifestation is pyramidal-extrapyramidal paresis of the limbs, including asymmetric tetraparesis. In addition to gross disturbances in the rhythm and frequency of breathing, autonomic disorders also appear: increased body temperature and blood pressure, hyperhidrosis, etc. A characteristic feature of the clinical course of diffuse axonal brain damage is the transformation of the patient’s condition from a prolonged coma to a transient vegetative state. The onset of this state is indicated by spontaneous opening of the eyes (with no signs of tracking or fixation of gaze).
Diagnosis
The CT picture of diffuse axonal brain damage is characterized by an increase in brain volume, as a result of which the lateral and third ventricles, subarachnoid convexital spaces, and also the cisterns of the base of the brain are under compression. The presence of small focal hemorrhages in the white matter of the cerebral hemispheres, corpus callosum, subcortical and brain stem structures is often detected.
Brain compression
Brain compression develops in more than 55% of cases of traumatic brain injury. The most common cause of brain compression is an intracranial hematoma (intracerebral, epi- or subdural). Rapidly increasing focal, brainstem and cerebral symptoms pose a danger to the life of the victim. Availability and duration of the so-called the “light gap” - expanded or erased - depends on the severity of the victim’s condition.
Diagnosis
A CT scan reveals a biconvex, less often a flat-convex, limited zone of increased density, which is adjacent to the cranial vault and is localized within one or two lobes. However, if there are several sources of bleeding, the area of increased density can be significant in size and have a crescent shape.
Treatment of traumatic brain injury
When a patient with a traumatic brain injury is admitted to the intensive care unit, the following measures must be taken:
Examination of the victim’s body, during which abrasions, bruises, joint deformities, changes in the shape of the abdomen and chest, bleeding and/or liquor leakage from the ears and nose, bleeding from the rectum and/or urethra, and a specific odor from the mouth are detected or excluded.
Comprehensive x-ray examination: skull in 2 projections, cervical, thoracic and lumbar spine, chest, pelvic bones, upper and lower extremities.
Ultrasound of the chest, ultrasound of the abdominal cavity and retroperitoneal space.
Laboratory tests: general clinical analysis of blood and urine, biochemical blood test (creatinine, urea, bilirubin, etc.), blood sugar, electrolytes. These laboratory tests must be carried out in the future, daily.
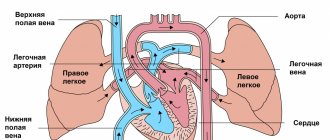
ECG (three standard and six chest leads).
Testing urine and blood for alcohol content. If necessary, consult a toxicologist.
Consultations with a neurosurgeon, surgeon, traumatologist.
A mandatory method of examining victims with traumatic brain injury is computed tomography. Relative contraindications to its implementation may include hemorrhagic or traumatic shock, as well as unstable hemodynamics. Using CT, the pathological focus and its location, the number and volume of hyper- and hypodense zones, the position and degree of displacement of the midline structures of the brain, the condition and degree of damage to the brain and skull are determined. If meningitis is suspected, a lumbar puncture and dynamic examination of the cerebrospinal fluid are indicated, which allows monitoring changes in the inflammatory nature of its composition.
A neurological examination of a patient with a traumatic brain injury should be performed every 4 hours. To determine the degree of consciousness impairment, the Glasgow Coma Scale is used (state of speech, response to pain and ability to open/close eyes). In addition, the level of focal, oculomotor, pupillary and bulbar disorders is determined.
For a victim with impaired consciousness of 8 points or less on the Glasgow scale, tracheal intubation is indicated, due to which normal oxygenation is maintained. Depression of consciousness to the level of stupor or coma is an indication for auxiliary or controlled mechanical ventilation (at least 50% oxygen). With its help, optimal cerebral oxygenation is maintained. Patients with severe traumatic brain injury (hematomas, cerebral edema, etc. detected on CT) require monitoring of intracranial pressure, which must be maintained below 20 mmHg. For this purpose, mannitol, hyperventilation, and sometimes barbiturates are prescribed. To prevent septic complications, escalation or de-escalation antibacterial therapy is used. For the treatment of post-traumatic meningitis, modern antimicrobial drugs approved for endolumbar administration (vancomycin) are used.
Patients begin feeding no later than 3 days after TBI. Its volume is increased gradually and at the end of the first week following the date of the traumatic brain injury, it should provide 100% of the patient’s caloric needs. The route of nutrition can be enteral or parenteral. To relieve epileptic seizures, anticonvulsants are prescribed with minimal dose titration (levetiracetam, valproate).
The indication for surgery is an epidural hematoma with a volume of over 30 cm³. It has been proven that the method that provides the most complete evacuation of the hematoma is transcranial removal. Acute subdural hematoma with a thickness of more than 10 mm is also subject to surgical treatment. In comatose patients, acute subdural hematoma is removed by craniotomy, retaining or removing a bone flap. An epidural hematoma with a volume of more than 25 cm³ is also subject to mandatory surgical treatment.
Prognosis for traumatic brain injury
Concussion is a predominantly reversible clinical form of traumatic brain injury. Therefore, in more than 90% of cases of concussion, the outcome of the disease is the recovery of the victim with full restoration of ability to work. Some patients, after the acute period of concussion, experience certain manifestations of post-concussion syndrome: disturbances in cognitive functions, mood, physical well-being and behavior. 5-12 months after a traumatic brain injury, these symptoms disappear or are significantly smoothed out.
Prognostic assessment in severe traumatic brain injury is carried out using the Glasgow Outcome Scale. A decrease in the total number of points on the Glasgow scale increases the likelihood of an unfavorable outcome of the disease. Analyzing the prognostic significance of the age factor, we can conclude that it has a significant impact on both disability and mortality. The combination of hypoxia and arterial hypertension is an unfavorable prognosis factor.
Diagnostic measures
To establish a correct diagnosis, the patient undergoes a series of tests. These include:
- X-ray of the skull and cervical spine shows the presence of cracks or displacements.
- Encephalography and echoencephaloscopy - helps to identify hidden lesions.
- Fundus examination - checking the vessels and optic nerve head to exclude bleeding or lamellar hematoma.
- Computer scanning - in severe stages of damage to examine hard-to-reach areas of the brain.
You can sign up for diagnostics using the search service mrt-mozga.ru. Here you will find information about the number of vacancies, current price lists, customer reviews and receive professional advice from company operators.
How to help the victim?
The first step is to call an ambulance, even if the person refuses, claiming that he is already better. Delay often leads to subsequent difficulties in carrying out diagnostic measures.
But giving any painkillers or other medications before the doctors arrive is strictly prohibited. In the best of circumstances, pharmacological agents will only blur the overall clinical picture. But in a more serious scenario, they will only harm a weakened body.
While others are waiting for specialists to arrive, the patient will need to provide:
- cold;
- hunger;
- peace.
It is better to start with the last point, which provides for mandatory bed rest in the safest possible environment. Moreover, it is extremely important not just to send a person to sit without unnecessary movements, but to move him to a horizontal position, limiting his mobility.
Recommends applying cold to the head. A heating pad with ice water, pre-wrapped in a towel, is best suited for these purposes. If you don’t have ice on hand, a simple cold compress made from a rag will do. Exposure time is up to 5 minutes.
It is also important to ensure that the victim’s head is slightly higher than the body itself. Open a window to allow fresh air to enter.
When, during the initial examination, it turns out that the patient is unconscious, the first task of those around him is to bring him to his senses. Having shifted the person to his side, it is worth going for ammonia. A cotton swab is moistened with the solution and then brought to the patient’s nose.
If a person constantly falls into an unconscious state, then it is better to leave him to continue lying on his right side, bending his left arm and leg 90 degrees. The head should be directed towards the floor. This will ensure complete intake of air into the lungs, as well as prevent tongue retraction or suffocation due to uncontrolled release of vomit.
You should not give the patient any alcoholic drinks “for courage,” as this will only increase the already significant load on the cardiovascular system, increase blood pressure, and increase cerebral edema. In cases where outpatient therapy is indicated, the person is not allowed to return to their usual pace of life.
During treatment, you will have to give up any physical activity, and also not watch TV or strain your eyes when working with a computer. If you follow such a simple rehabilitation program, you will be able to recover in approximately 2-4 weeks.
In some cases, for final confirmation of recovery, it is necessary to undergo auxiliary instrumental diagnostics. This can be either computed tomography or magnetic resonance imaging.